
The belief that “all experiences are equal” in premed preparation is statistically false. Shadowing, volunteering, and research do not carry the same weight—and the data show that the relative value shifts by school type, especially between MD and DO programs, and between research-heavy and community-focused schools.
Medical schools rarely publish exact “point systems,” but combining AAMC/ERAS reports, MSAR trends, and school-specific disclosures allows a reasonably accurate, data-driven approximation of how each experience category functions in admissions.
This article dissects that relative weight, by school type, using a quantitative frame: what seems required, what functions as a differentiator, and where “extra” hours start yielding diminishing returns.
(See also: How Many Shadowing Hours Do Matriculants Actually Have? Data Review for more details.)
1. The Baseline: What the Data Say About Experiences Overall
Granular admissions formulas are not public, but several consistent data sources exist:
- AAMC “Premedical Experiences” and “Matriculating Student” surveys
- ERAS “Experiences” sections and post-match analyses
- MSAR experience expectations and school self-reports
- DO school websites and AACOM guidance
- Indirect evidence from hundreds of student-reported acceptances (public trackers, advising data)
From these, three clear patterns emerge:
- Nearly all accepted MD and DO applicants report:
- Physician shadowing
- Clinical or non-clinical volunteering
- A large majority of MD applicants report some research, with much higher prevalence at research-intensive schools.
- DO schools systematically emphasize shadowing (especially DO-specific) more than MD schools.
A workable way to think about this is experience “weighting” on a 0–10 importance scale for admission, not for personal growth:
- 0–3: nice-to-have, rarely decisive
- 4–7: core expectation / major influence
- 8–10: near-requirement or decisive differentiator
We cannot assign exact numeric weights per school, but we can reasonably model ranges by school type.
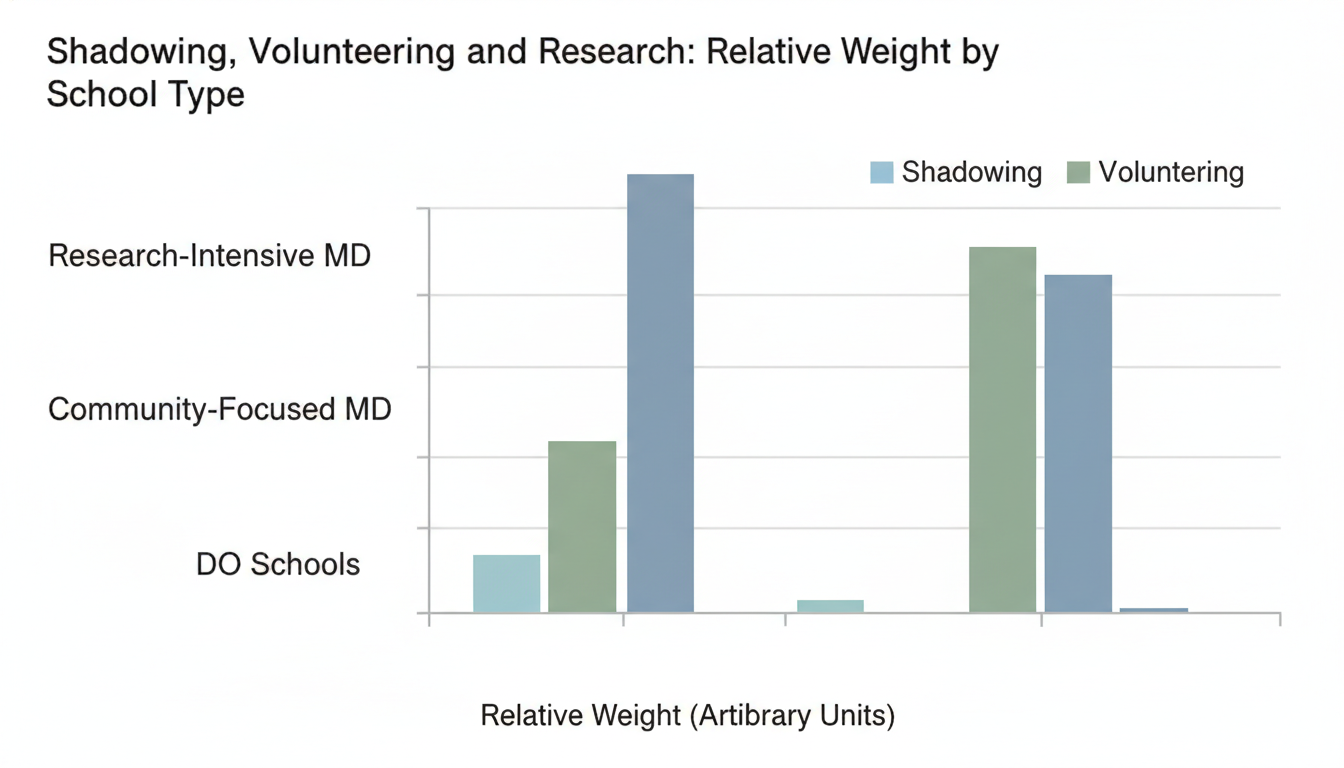
2. MD vs DO: Macro-Level Weighting
The relative weight of shadowing, volunteering, and research shifts systematically between MD and DO programs.
Approximate Relative Weights by Broad School Type
These ranges synthesize public data and advising patterns. The numbers represent relative importance for admissions, not absolute value, on a 0–10 scale.
U.S. MD Schools – Research-Intensive (Top 30-40 by NIH Funding)
- Shadowing: 5–6
- Volunteering (clinical + non-clinical): 7–8
- Research: 8–10
Characteristics:
- Expectation of meaningful research, often with outputs.
- Clinical exposure and service required but not uniquely differentiating once above baseline.
- Shadowing is necessary, but once basic understanding is proven, more hours add little.
U.S. MD Schools – Community-Focused / Less Research-Heavy
- Shadowing: 6–7
- Volunteering: 8–9
- Research: 4–6
Characteristics:
- Mission-driven focus on service and community engagement.
- Research still valued but less central; often “nice to have” rather than “must have.”
- Shadowing weight rises because schools want proof you understand everyday practice, not just academic medicine.
U.S. DO Schools
- Shadowing (especially DO-specific): 8–10
- Volunteering: 7–8
- Research: 2–4
Characteristics:
- DO shadowing is often explicitly required or strongly recommended (many schools list minimum hours).
- Community service and longitudinal patient contact emphasized.
- Research is usually nonessential and low-weight unless the applicant is targeting academic DO training paths.
Within each category, individual schools shift slightly, but the overall pattern is consistent: research weight is highest in research MD programs; shadowing weight is highest in DO programs; volunteering weight stays high almost everywhere.
3. Shadowing: High Yield for DO, Baseline for MD
The data show shadowing is the most asymmetrically weighted category between MD and DO programs.
MD Programs: Shadowing as a Threshold, Not a Differentiator
From AAMC applicant surveys and acceptance profiles:
- Well over 90% of MD matriculants report physician shadowing.
- Median shadowing time often lands between 50–100 hours, but with wide range (20–300+).
Functionally, MD schools seem to treat shadowing as:
- A binary threshold: Do you understand what doctors do and how clinics/hospitals work?
- A risk reducer: Preventing admission of students who later realize they dislike real-world medicine.
Estimated MD relative weight:
- Below ~20–30 hours: risk flag
- 20–50 hours: acceptable baseline
- 50–150 hours: solid; more does not heavily increase marginal benefit
200 hours: limited added admissions value unless uniquely meaningful or in underserved/rural settings
Quantitatively, for many MD programs, shadowing might account for something like:
- Roughly 10–15% of the “experiences” weight in holistic review
- But almost 0% of differentiation once you are safely above the threshold compared to research and long-term service
DO Programs: Shadowing as a Core Requirement
DO school data and AACOM guidance paint a different picture:
- Many DO schools explicitly ask for 40–100+ hours of physician shadowing.
- Several specify that a significant portion must be with a DO physician (e.g., 20–50 hours DO-specific).
Qualitative screening reports and student outcomes show repeated patterns:
- Applicants with <20 hours of total shadowing or no DO-specific exposure are frequently screened out or waitlisted.
- Applicants with 40–80+ hours including DO exposure have much higher interview rates, controlling for GPA/MCAT.
Here, shadowing is not just “do you know what medicine is?” but:
- “Do you understand osteopathic practice and philosophy?”
- “Have you deliberately chosen DO, not just applied as a backup?”
Estimated DO relative weight:
- Shadowing (especially with DOs) can account for 20–30% of the experiences-based judgment.
- A single strong DO letter from a physician you shadowed can function as a multiplier on this category.
In data terms: among borderline-GPA DO-accepted students, robust shadowing profiles appear at considerably higher frequencies than robust research profiles.
By School Type – Shadowing Emphasis
Approximate 0–10 impact scores:
- Research-heavy MD: 5–6
- Community-focused MD: 6–7
- DO: 8–10
Practical implication: If you are applying DO or to mission-driven MD schools, marginal returns on additional shadowing hours are higher than for purely research-heavy MD schools, especially when those hours are longitudinal and DO-centric.
4. Volunteering: The Universal High-Weight Category
Unlike research, volunteering and service maintain strong weight across all school categories. The data suggest this category is where many admissions decisions pivot, especially at mid- and lower-tier MD and DO schools.
Clinical vs Non-Clinical Volunteering
AAMC breakdowns and school guidance distinguish two main flavors:
- Clinical volunteering / paid clinical work (e.g., CNA, MA, EMT, scribe, hospital volunteer)
- Non-clinical service (e.g., tutoring underserved populations, food banks, crisis hotlines, community outreach)
Patterns in matriculant data:
- A large majority of matriculants (often >85–90%) have both clinical exposure and some non-clinical service.
- Successful applicants frequently report 150–400+ total hours of combined service, though there is wide variance.
From an admissions analytics perspective:
- Schools often weigh longitudinal, population-serving roles more than episodic, short-term events.
- For mission-oriented schools, the volunteering category can effectively become the primary “fit” variable.
Relative Weight by School Type
Again on the 0–10 relative scale:
- Research-heavy MD:
- Volunteering: 7–8
- Interpreted mainly as: commitment to service + basic patient-centeredness.
- Community-focused MD:
- Volunteering: 8–9
- Often the single most influential non-academic factor in acceptance. Schools filter heavily for sustained, community-facing engagement aligned with their mission (e.g., rural health, underserved urban communities).
- DO:
- Volunteering: 7–8
- Heavily valued, especially when combined with clinical work in primary care–like settings.
In numeric impact terms, volunteering and clinical work likely represent:
- 25–35% of non-academic evaluation at community-focused MD and DO schools.
- Roughly 20–30% at research-heavy MD schools (slightly lower because research steals some of that share).
What the data do not support:
- The idea that research can “substitute” for weak service at a service-heavy or DO-focused school.
- At mission-driven MD and DO programs, lack of consistent service frequently correlates with rejection, even with strong research or metrics.
5. Research: High-Variance Weight by School Type
Research is the most polarizing category. For some schools, it is the center of gravity. For others, it barely registers.
Research-Intensive MD Programs
AAMC data show that at top NIH-funded institutions (top ~30–40):
- A high proportion of matriculants report significant research (often 1–3+ years).
- Many have at least one of:
- Poster presentation
- Publication
- Senior thesis / substantial project
In practice:
- For MD/PhD or PSTP-type trajectories, research weight approaches 10/10; it is a precondition.
- For straight MD at these schools, research likely carries:
- 25–40% of non-academic evaluation weight, particularly when publication-level or independent.
The impact is not only binary “has research / no research” but also:
- Duration: 1 summer vs 2–3 years
- Intensity: assistant vs independent responsibility
- Output: no presentations vs abstracts vs publications
Applicants with:
- Zero research at a research-intense MD school: statistically disadvantaged, sometimes heavily.
- Some research but no outputs: mid-range; can be competitive with strong GPA/MCAT and strong service.
- At least one solid output: substantial boost, especially if paired with strong letters from PIs.
Community-Focused MD Programs
These schools often state explicitly that they do not require or heavily emphasize research:
- Many accepted students have some research exposure, mainly because it is common at larger universities.
- However, admissions outcomes show students with near-zero research but strong service still being accepted regularly.
Estimated weight:
- Research: 4–6 on the importance scale.
- Often functions as “tie-breaker” or “nice spike,” but not a gatekeeper.
A realistic model:
- If clinical exposure and volunteering are high, research can shift an applicant slightly up but rarely rescues weaknesses in other categories.
- At these schools, time tradeoffs favor more community engagement over extra lab hours.
DO Programs
Research weight at DO schools is consistently low:
- Many DO matriculants report limited or no formal research.
- DO school mission statements rarely highlight basic science or large NIH-funded labs as a top priority.
Estimated importance:
- 2–4 on the 0–10 scale.
- Mostly helpful if:
- Related to clinical or health services outcomes.
- Used to demonstrate academic curiosity and ability to handle evidence-based medicine.
For DO programs, extra hours in research above a basic exposure level often yield very low marginal return compared to extra shadowing or service.
Aggregate Research Weight by School Type
On the 0–10 scale:
- Research-heavy MD: 8–10
- Community-focused MD: 4–6
- DO: 2–4
This is the sharpest gradient among the three experience categories.
6. Relative Tradeoffs: If You Must Choose Where to Invest Hours
Students frequently face binding constraints: limited time, financial pressures, or heavy coursework. From a data-analytic perspective, the optimal allocation of marginal hours depends strongly on school target mix.
Assume you have 200 “extra” hours over a year. Where does each hour do the most work?
Scenario A: Targeting Research-Intensive MD Schools
Relative marginal value of an added hour once basic thresholds are met (very rough):
- Research: High marginal utility up to the point of obtaining:
- Meaningful responsibility, and
- At least one presentation or abstract.
- Clinical volunteering: Moderate marginal value if below ~150–200 total hours; lower once solid.
- Shadowing: Low marginal value once 40–60 hours with diverse specialties are achieved.
Approximate ordering:
- Research (to reach an output or clearly defined project)
- Clinical/non-clinical volunteering
- Extra shadowing
Scenario B: Targeting Community-Focused MD Schools
Relative marginal value:
- Volunteering (especially with underserved populations): Very high, especially going from sporadic to longitudinal roles.
- Clinical employment (scribe, MA, EMT, CNA): High; demonstrates comfort with patients and health systems.
- Research: Moderate, mostly useful after other categories are strong.
- Shadowing: Necessary, but returns flatten after threshold.
Ordering:
- Volunteering / clinical work
- Additional patient-facing roles
- Modest research if none exists
- Extra shadowing
Scenario C: Targeting DO Schools
Relative marginal value:
- DO-specific shadowing: Very high until 40–80+ hours are reached.
- Clinical work and volunteering: Very high, especially in primary care or community settings.
- Research: Low, unless personally valuable or linked to long-term interests in academic DO careers.
Ordering:
- DO and general physician shadowing (to meet explicit expectations)
- Clinical volunteering / paid clinical work
- Non-clinical service
- Research (beyond basic exposure)
This allocation is consistent with who actually matriculates where, when comparing self-reported experience portfolios.
7. Concrete Target Ranges by School Type
The numbers below are not formal cutoffs but ranges where admitted students tend to cluster. They represent reasonable targets, not guarantees.
For Research-Intensive MD-Focused Applicants
By application time:
- Shadowing:
- 50–120 total hours
- Across 2–4 specialties or settings
- Volunteering / clinical:
- 150–400+ combined hours
- Split between clinical and meaningful non-clinical service
- Research:
- 1–3+ years
- Aim for at least one presentation / abstract / publication if possible
- 400–1000+ cumulative hours over several years is common for strong applicants
In this pattern, research can carry a weight similar to or higher than volunteering in decision-making at top research schools.
For Community-Focused MD-Focused Applicants
- Shadowing:
- 40–100 hours
- Emphasis on primary care or settings that match the school’s mission
- Volunteering / clinical:
- 250–500+ hours total
- Clear longitudinal service (1+ years) in underserved or community health contexts
- Research:
- 0–300 hours (optional)
- A small project or summer experience is helpful but not essential
Here, admissions readers often treat the service portfolio as a stronger predictor of fit and future practice pattern than research.
For DO-Focused Applicants
- Shadowing:
- 60–150 total hours
- At least 20–50 hours must be DO shadowing at many programs
- Aim for a DO letter if possible
- Volunteering / clinical:
- 200–400+ hours
- Clinical employment in primary care or community clinics is especially valued
- Research:
- 0–200 hours (optional)
- No penalty for low research if other areas are robust
In this profile, shadowing is often the single most heavily weighted of the three experience types.
8. Pulling the Data Together: Key Takeaways
Condensing the comparative weights:
Shadowing
- Baseline requirement across all schools.
- Highest relative weight at DO schools and community-focused MD programs.
- After ~50–100 hours, extra time is low-yield for research-heavy MD unless it changes narrative (e.g., rural health focus).
Volunteering / Clinical Service
- Universally high-weight, especially when sustained and community-facing.
- Often the single strongest non-academic predictor of acceptance at community-focused MD and DO schools.
- Weak service is consistently associated with rejections, even with good metrics.
Research
- Major differentiator at research-intensive MD schools; near-mandatory for MD/PhD.
- Moderate value at community MD, low-to-moderate at DO.
- Should not be prioritized over service and shadowing if targeting non-research-heavy programs.
If you align your time investment with the evidence-based weighting by school type—heavier research for research MD, heavier service and shadowing for community MD and DO—you move from generic preparation to strategically optimized preparation. The data are clear: the same 500 hours can have very different admissions impact depending on where and how you deploy them.





















