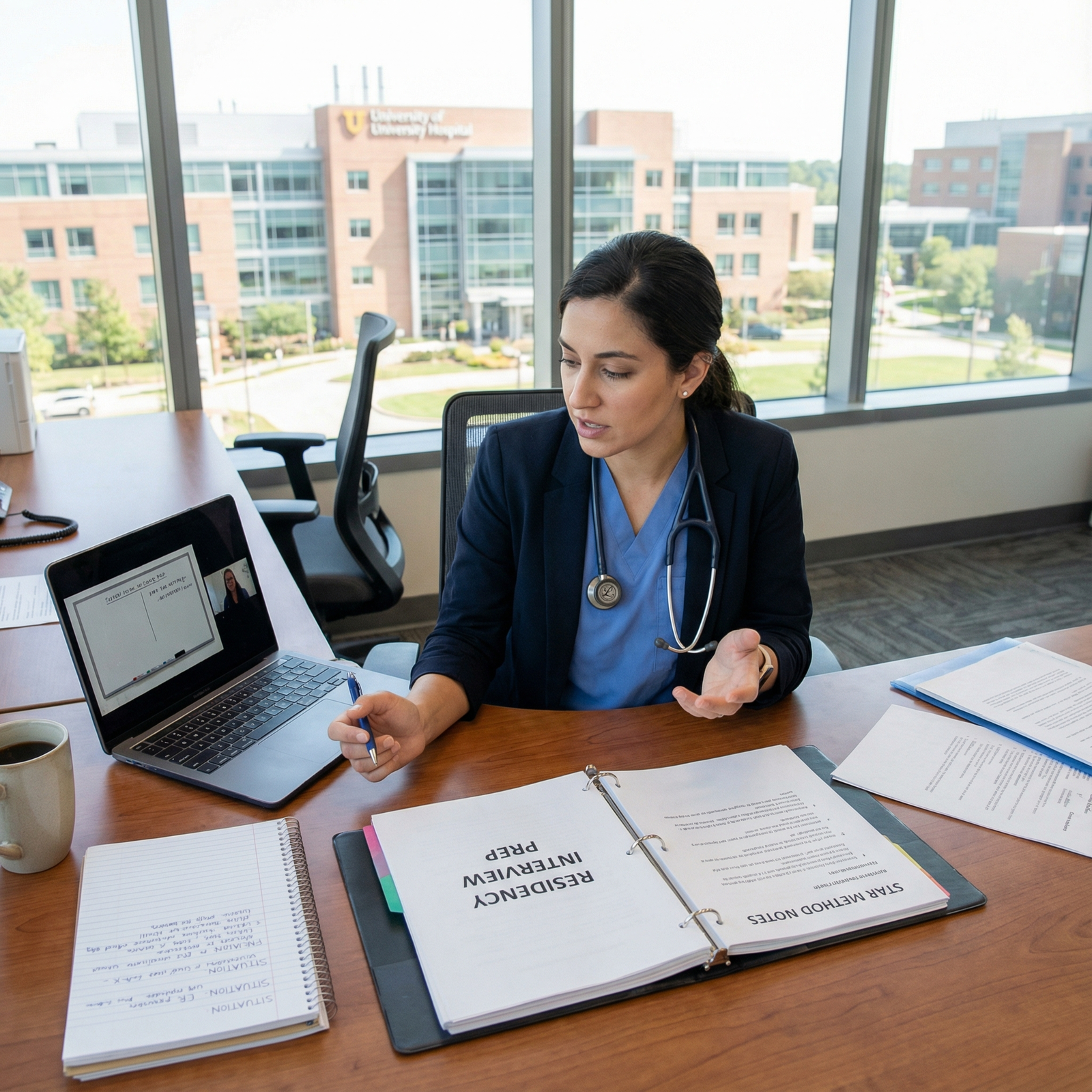
You’re in a Zoom interview, PGY-2 in surgery turned PGY-1 in anesthesia, and the program director leans in a little and asks: “So… walk me through why you left your previous specialty.” You feel your throat tighten. Because you know this isn’t just curiosity. They’re asking: Are you going to bail on us too?
If you switched specialties late in training, every behavioral question becomes a double audition. You’re not just proving you’re competent. You’re proving you’re stable, self-aware, and not a ticking time bomb.
Let’s fix how you frame your stories so you come across as deliberate and mature, not flaky or running away.
What Programs Are Really Worried About
I’m going to be blunt. When a PD sees “prior residency” or a midstream specialty switch, a few alarms go off:
- Will this person quit again when it gets hard?
- Are there professionalism or performance issues hiding behind this “career change”?
- Is this someone who blames systems and other people instead of owning their decisions?
- Are they chasing prestige, lifestyle, or rumors instead of a grounded fit?
If your behavioral stories sound like:
- “The culture was toxic.”
- “I just realized late that it wasn’t for me.”
- “I wanted better lifestyle.”
- “I was unhappy, so I left.”
…you’re feeding those fears.
You need to reframe around:
- Deliberate decision-making, not impulse.
- Growth and self-knowledge, not crisis.
- Transferable skills from the first specialty.
- Evidence that you commit and follow through.
The 3 Non-Negotiable Storylines You Must Master
There are three behavioral “arcs” you absolutely must have clean, repeatable stories for if you switched late:
- Why you chose the first specialty (and why that wasn’t a stupid decision).
- Why you decided to switch (and what changed).
- How you handled the switch (and what you learned + how you grew).
You’ll use these arcs across dozens of behavioral questions: “Tell me about a challenge”, “Describe a conflict”, “Give an example of a difficult decision”, etc.
Let’s break each down and then layer on specific behavioral stories.
1. Framing Why You Chose Your First Specialty
You cannot throw your old specialty under the bus. That makes you look impulsive or bitter. You need to sound like a thoughtful person who made a reasonable decision with the information you had.
Bad version:
- “I went into surgery because that’s what everyone did at my med school.”
- “I picked OB because I loved the idea but had no idea what it was really like.”
- “I just thought EM would be cool.”
Better structure:
- A traceable, rational reason you chose it.
- Specific experiences that support that choice.
- A bridge that sets up your later realization.
Example for someone moving from IM to Radiology:
“Going into residency, I chose internal medicine because I liked complex problem solving and longitudinal relationships. On my third-year rotations, I loved working through differential diagnoses and managing multi-morbidity in the ICU. It made sense at the time—broad training, lots of exposure, and I truly valued patient interaction. That foundation in clinical reasoning has been incredibly useful, even though I ultimately realized I was most energized by the diagnostic side of medicine rather than long-term management.”
Notice what that does:
- Validates the original choice.
- Shows you weren’t clueless.
- Sets up a pivot from “I liked X” to “But I later learned I’m best at Y.”
Now plug in your own version. Ask yourself:
- What did I genuinely like about the old specialty before I soured on it?
- What concrete experiences at the time made that choice reasonable?
- What parts of that specialty still help me today?
Write that out in 3–5 sentences. You’ll reuse it constantly.
2. Framing Why You Switched Late (Without Sounding Unstable)
This is the landmine.
You must avoid two extremes:
- “It was hell, so I left.” -> impulsive, avoidant
- “Everything was fine, I just switched.” -> shallow, confusing
You need a narrative that shows:
- Progressive realization, not overnight drama.
- You did serious self-reflection.
- You attempted to adapt and improve the situation before leaving.
- The new specialty is clearly aligned with your skills and values.
Use a timeline-based structure. Something like:
- Initial fit seemed okay.
- Over time, specific mismatch patterns kept repeating.
- You sought feedback/mentorship and tried to make it work.
- You did targeted exposure to the new specialty.
- You made a structured, planned transition.
Here’s a polished version for someone who switched from Surgery to Anesthesia late PGY-2:
“During my first year in general surgery, I enjoyed the OR and the acuity but I noticed that the parts of my day that energized me most were the intraoperative physiology discussions with anesthesia and the immediate hemodynamic management. Over my second year, that pattern became more obvious: I found myself more engaged in the anesthetic planning than in the postoperative clinic or ward management. I spoke with my program director and a few mentors about this, and they encouraged me to explore it in a structured way. I arranged elective time with anesthesia, did additional reading in pharmacology and physiology, and realized that my strengths—situational awareness, calm under pressure, and interest in physiology—aligned much more with anesthesiology. At that point, I made a deliberate decision to switch, with support from my prior program, rather than continue on a path that wasn’t the best long-term fit for me or for my patients.”
That hits every checkbox:
- Not impulsive.
- Not slamming the old program.
- Shows introspection.
- Shows action steps and mentorship.
- Ties concrete traits to the new specialty.
Write your own version. If possible, include:
- Names of roles (not necessarily people): PD, advisor, mentor.
- Specific exposure: rotations, electives, shadowing, research.
- A clear “inflection point” when you decided.
3. How You Handled the Switch (This Is Your Character Test)
Programs will test this from every angle with behavioral questions:
- “Tell me about a time you made a difficult decision.”
- “Describe a time you faced a setback.”
- “Give an example of a time you had to have a hard conversation.”
Your answer should quietly demonstrate how you managed your transition.
Use the STAR or CAR structure, but don’t sound robotic. Think:
- Situation / Context
- Task (your responsibility)
- Action (what you did)
- Result (what happened + what you learned)
Let’s build one core story and then I’ll show you how to repurpose it.
Core story: The decision conversation with your PD
Situation: Late in PGY-2, realization of mismatch, preparing to speak with PD.
Action details to highlight:
- You prepared (reflected, listed pros/cons, consulted mentors).
- You owned your decision (no blaming).
- You focused on patient care and program impact, not just your feelings.
- You communicated early and honestly.
Example:
“By the middle of my second year, it was clear to me that although I was performing well in my surgical rotations, my long-term fit was elsewhere. I felt a responsibility to address it early rather than drift along. I scheduled a dedicated meeting with my program director, came in with specific examples of what I’d enjoyed and where I felt misaligned, and shared that I’d done elective time in anesthesia and spoken with several mentors. I made it clear that this wasn’t about call schedules or personalities but about where I could contribute best over a 30-year career. Together, we mapped out a plan that allowed me to complete the year responsibly while beginning the application process for anesthesia. That conversation was difficult, but it reinforced for me the value of transparent communication and making thoughtful decisions even when they’re uncomfortable.”
You can now morph that same story into multiple behavioral answers:
- Difficult decision? -> Emphasize pros/cons and timeline.
- Handling conflict? -> Emphasize the tough conversation with PD and being honest.
- Leadership/professionalism? -> Emphasize finishing your responsibilities and safe transition.

| Step | Description |
|---|---|
| Step 1 | Identify Switch Reason |
| Step 2 | Map Timeline of Realization |
| Step 3 | List Key Conversations |
| Step 4 | Extract 3-4 Core Stories |
| Step 5 | Match Stories to Common Questions |
| Step 6 | Practice Concise Versions |
Turning Behavioral Questions to Your Advantage
You’re going to be asked the “Why did you switch?” question directly. Fine. Prepare for it.
But the real win is when you proactively weave your switch into answers to standard behavioral questions so there are no “mystery gaps” in your story.
Here’s how to reframe common question types.
1. “Tell me about a time you made a difficult decision.”
You use the specialty switch itself. That’s the obvious one. Keep it under 2 minutes.
Key beats:
- Noticing the misalignment.
- Gathering data, seeking mentorship.
- Considering the impact on colleagues, patients, and your career.
- Making a clear decision and communicating it.
Avoid:
- Over-explaining the drama with your old program.
- Over-emphasizing lifestyle or location unless it’s clearly secondary.
2. “Tell me about a time you failed or things didn’t go as planned.”
Perfect place to talk about realizing your first specialty choice wasn’t the best long-term match.
Frame it as:
“The ‘failure’ was not that surgery/IM/OB is bad, but that my initial self-assessment was incomplete. Here’s how I corrected course responsibly.”
Example skeleton:
“I’d consider my initial specialty choice a kind of failure in self-assessment. Not dramatic—my evaluations were solid and I learned a lot—but I realized I hadn’t fully understood where I did my best work. Rather than ignoring that discomfort, I treated it like any other clinical problem: gather data, get second opinions, and adjust the plan. I arranged X, spoke with Y, and ultimately made the decision to switch to Z. It taught me to be more honest earlier with myself and to view course correction as a professional responsibility, not a personal defeat.”
Again, you’re not confessing catastrophe. You’re showing maturity.
3. “Describe a time you handled conflict or disagreement.”
Use either:
- A tough conversation with a mentor/PD about your decision.
- Or a scenario where colleagues didn’t understand or initially support your switch.
The point: you stayed professional, listened, and held your ground without burning bridges.
4. “Tell me about your biggest professional challenge.”
Use the period of doubt and transition. The challenge isn’t switching; it’s functioning at a high level while you’re in limbo.
Example angle:
“My biggest professional challenge was staying fully engaged and present for my patients while I was working through the decision to change specialties. I set specific commitments—finishing my year strong, volunteering for teaching duties, and maintaining my clinical performance—so that my internal uncertainty didn’t affect patient care or my team.”
That shows programs what they care about: you don’t check out when things are hard.

Cleaning Up the Red Flags in Your Stories
There are specific phrases that make PDs nervous. Cut them or reframe them.
Here’s a quick reference.
| Risky Phrase | Strong Alternative |
|---|---|
| The culture was toxic | The fit between my working style and the environment wasn’t ideal |
| I hated the lifestyle | I realized I’m at my best in [outpatient/OR/ICU/clinic] settings |
| I just knew it wasn’t right | Over time, a clear pattern emerged about where I was most engaged |
| My program didn’t support me | I had open conversations with my leadership about my evolving goals |
| I was burned out | I recognized early signs of burnout and sought mentorship and structural changes |
Programs don’t want victims. They want adults who can talk about problems without sounding like they’re relitigating grievances.
Be especially careful about words like:
- “Toxic”
- “Abusive”
- “Horrible”
- “Unbearable”
If there were truly serious issues (harassment, discrimination), you can allude to them without turning your interview into a deposition. For instance:
“There were elements of the environment that weren’t sustainable for me long term, even after I tried to address them through the appropriate channels. That was one factor, but the larger driver was recognizing that my clinical interests and strengths aligned better with [new specialty].”
Short, controlled, then move on.
Show, Don’t Just Say: Bring Evidence of Stability
Your words are one thing. Evidence is another. When you’ve switched specialties late, they want proof that you’re not a repeat flight risk.
Here’s what to subtly highlight in your stories:
- You completed commitments you’d already made (finished the year, finished projects).
- You kept good relationships with your prior faculty (letters from them help).
- You’ve had sustained exposure to the new specialty, not a 1-month fling.
- You’ve done something extra to demonstrate commitment: research, QI, teaching, electives.
You can slide this into answers:
“When I decided to apply to psychiatry, I stayed on in my internal medicine program through the end of the academic year, completed my continuity clinic responsibilities, and helped onboard the incoming interns. During that time, I also worked with the consult-liaison team on a small QI project looking at [X]. That experience confirmed the switch was the right direction and that I could contribute meaningfully to the new field.”
Notice: stability, follow-through, relationships, proactivity.

| Category | Value |
|---|---|
| Stability | 90 |
| Insight | 85 |
| Professionalism | 80 |
| Transferable Skills | 75 |
| Commitment to New Field | 88 |
Practice: One Switch, Four Behavioral Stories
Let’s make this brutally concrete. Say you switched from Pediatrics to Psychiatry after PGY-2.
You should be able to answer, in 90–120 seconds each:
- “Why did you leave pediatrics?”
- “Tell me about a time you made a difficult decision.”
- “Describe a time you had to deliver difficult news or have a hard conversation.”
- “Tell me about a time you adapted to a new environment.”
All four can be variations on the same core events, with slightly different angles.
Skeletons:
Why you left:
- Rational original choice, specific realization it wasn’t ideal, exploration of psych, structured decision.
Difficult decision:
- Choosing to switch despite sunk costs, conversations with mentor/PD, long-term thinking.
Hard conversation:
- Meeting with PD, explaining decision, planning transition that didn’t hurt patients or colleagues.
Adapting to new environment:
- Starting psych rotations/residency with pediatric background, leveraging rapport skills, catching up on new knowledge base.
If you can’t do that yet, you’re not ready. Sit down and script them. Out loud. Record yourself.

One More Trap: Over-Apologizing for Your Path
Some applicants show up to interviews acting like they committed a crime by changing paths. They over-explain. They apologize repeatedly. They try to convince every interviewer that they’re not flaky.
That insecurity leaks out and makes people nervous.
Your frame should be:
- “I made a thoughtful decision then.”
- “I gained valuable skills there.”
- “I recognized a better long-term fit.”
- “I handled the transition professionally.”
- “I’m here now because this is where I can contribute best.”
You are not asking for forgiveness. You’re explaining a mature career decision.

Your Next Step (Do This Today)
Open a blank document and write three headings:
- “Why I chose my first specialty”
- “Why I switched and how I did it”
- “What I bring now because of that path”
Under each, write a 5–7 sentence story in plain language, like you’re talking to a smart friend. Then trim each to under 2 minutes when spoken.
Tomorrow, record yourself answering:
- “Why did you leave [old specialty]?”
- “Tell me about a difficult decision you made.”
- “Tell me about a time you had to face a setback.”
If your answers to all three don’t sound like three angles on the same clear, coherent story, rework them until they do. That coherence is what makes programs trust you after a late specialty switch.




















