I Noticed Residents Looked Exhausted: Am I Overreacting or Right?
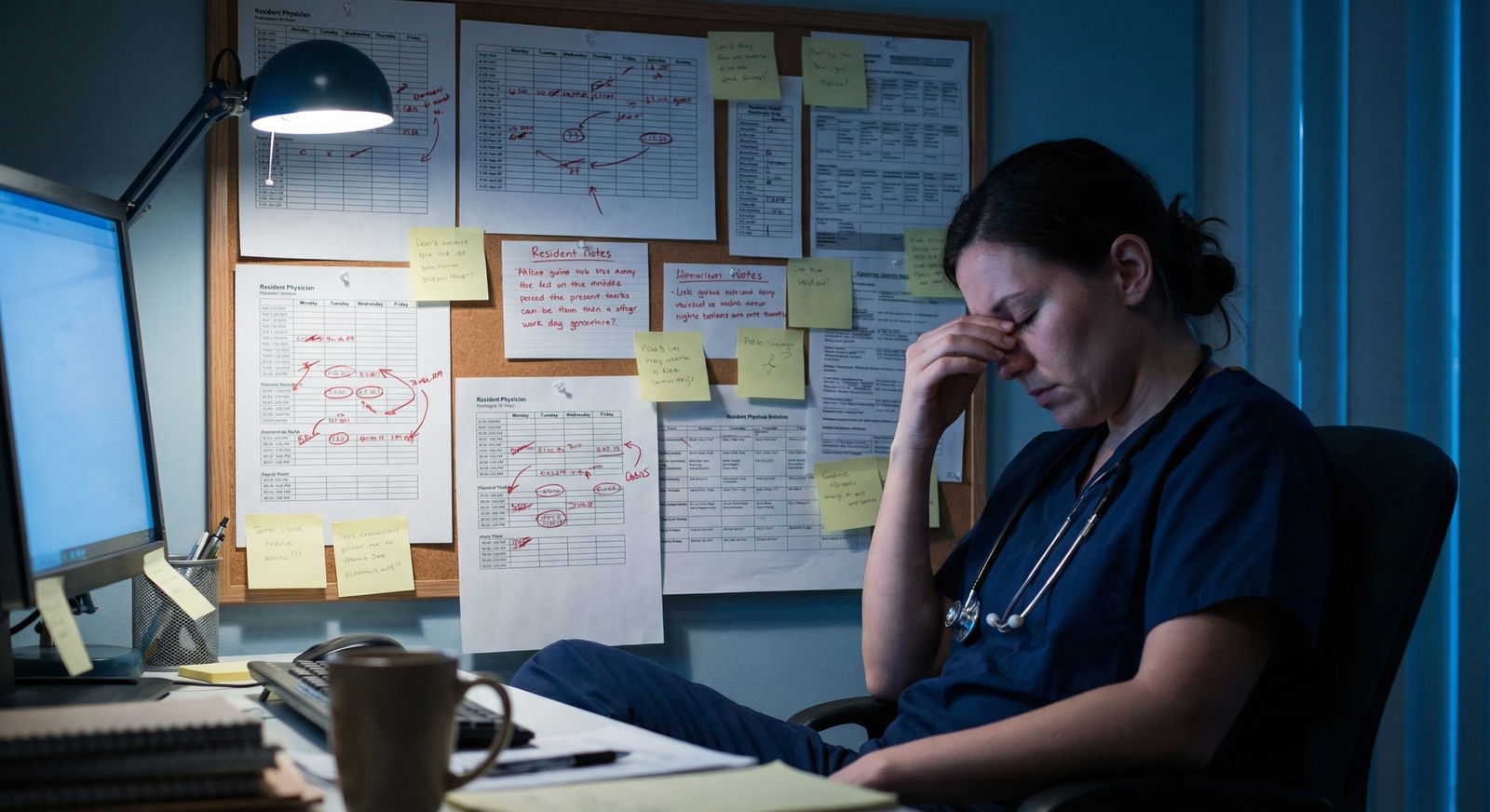
It’s 4:45 a.m. You’re on your third day of a sub‑I. You’re standing at the workroom door watching a senior resident chug cold coffee, sigh, rub their eyes, and then shuffle back to the computer like a zombie. Another resident just muttered “I haven’t peed since yesterday” and everyone laughed like that’s…normal.
And you’re thinking:
“Is this just how residency is?”
And under that:
“Am I signing up for a life I’m going to regret?”
You’re probably also doing the mental gymnastics:
“Maybe it was just a rough night.”
“Maybe I’m being dramatic.”
“Every program is like this…right?”
“Am I overreacting, or is this actually a red flag?”
Let me be blunt: you are not crazy for noticing. And you’re not wrong to be scared.
The hard part is separating “this is residency” tired from “this place is quietly destroying people” tired.
Let’s talk about that.
What Exhaustion Actually Tells You (And What It Doesn’t)
Every resident in the country is tired. That part is not a red flag. Training is intense, the work is heavy, and 3 a.m. pages do not care about your REM cycles.
But there are flavors of tired.
There’s the “I’m wiped but I still vaguely like my life” tired. And there’s the “I’m hanging on by a thread and nobody cares” tired.
Your gut is picking up on that distinction, which is why you’re here reading this.
Here’s the ugly truth: one exhausted resident means nothing. An entire vibe of exhaustion across multiple days, multiple rotations, and multiple residents? That’s data.

| Category | Value |
|---|---|
| Hours | 40 |
| Workload | 30 |
| Toxic Culture | 15 |
| Poor Staffing | 10 |
| Commute | 5 |
Notice what’s on that chart: the “unavoidable” stuff (hours, workload) and the “this is a systems failure” stuff (toxic culture, poor staffing). You’re trying to figure out what’s driving what you’re seeing.
You’re not going to get a label on their forehead that says “chill, it’s just nights.” So you watch. You listen. You ask.
Exhausted vs. Broken: The Difference You Need to See
You’re standing in the team room. It’s day five. Everyone looks tired. How do you tell if this is just standard-issue residency or a program-level problem?
Here’s the difference I pay attention to.
1. How they talk about being tired
Normal‑residency tired sounds like:
- “I’m wiped, but our attending actually helped with notes yesterday, so that saved us.”
- “I’m exhausted, but I learned a ton on this call.”
Broken‑program tired sounds like:
- “It doesn’t matter what we do, it’s never enough.”
- “They don’t care as long as the notes are done.”
- “We’re just bodies to fill the schedule.”
Those sentences matter. That’s not just fatigue. That’s demoralization.
2. What happens after a bad call night
One brutal call? Fine. It happens.
If you watch the team after a bad call and:
- They’re dragging, but they’re joking with each other.
- Someone says, “They sometimes bring us breakfast after nights.”
- Seniors check in: “Go lie down for 20 if I can cover your pager.”
That’s a tired but functional culture.
If instead:
- Everyone’s silently suffering.
- People get snapped at for being a little slow on rounds.
- No one even pretends wellness is a thing.
That’s a problem.
3. How many days in a row this looks the same
If it’s:
- Monday: everyone looks dead, but they perk up by noon.
- Tuesday: better.
- Wednesday: call night hangover.
- Thursday: still some smiles, people talk about days off.
That’s what I’d call a “baseline tired but alive” program.
If it’s:
- Every single day, every time you’re there, people have flat affect, hollow jokes, and that “stare at the wall for 10 seconds before answering a simple question” vibe…
I start to assume this is baked into the system, not just a couple of rough shifts.
Red Flag or Reality Check? A Brutally Honest Breakdown
You’re terrified of two extremes:
- Overreacting and crossing off a good program because you saw a bad week.
- Underreacting and ranking highly a place that will chew you up for three years.
Both are real risks. So let’s put some structure to it.
| What You Notice | More Likely Normal | More Likely Red Flag |
|---|---|---|
| Tired faces | Post‑call day, busy month | Constant, every day, every rotation |
| How they talk | “It’s rough but we’re supported” | “Nobody cares what happens to us” |
| Leadership vibe | PD/attendings visible and approachable | No one knows who PD is / residents afraid of them |
| Schedule | Occasionally stretched, but explained | Chronic violation of hours, brushed off |
| Resident mood | Sarcastic but still joking | Hopeless, bitter, checked‑out |
You’re not looking for perfection. You’re looking for patterns plus how the program responds.
A program that says, “Yeah, July on this service is brutal; we’re hiring another NP for day coverage” is very different from a program that shrugs and says, “Welcome to surgery.”
One is aware and trying. The other is hiding behind the “this is just residency” excuse as cover for laziness or abuse.
Questions You’re Afraid to Ask (But Should)
You’re not crazy for wanting to ask blunt questions. You’re just scared they’ll think you’re “not resilient” or “not a team player.”
I’ve heard PDs say exactly that about certain applicants. So yeah, your fear isn’t imaginary.
But there’s a way to ask about exhaustion without painting a target on your back.
Instead of:
“Everyone here looks miserable. Are you burning them out?”
Try things like:
- “How does your program respond when a service is consistently over hours?”
- “What changes have you made in the last 1–2 years based on resident feedback?”
- “Can you talk about any recent efforts to improve workload or patient caps?”
- “How easy is it for a resident to say, ‘this is too much,’ without retaliation?”
And my favorite, because it forces specifics:
- “Can you give an example of a time residents brought up a concern and something actually changed?”
If they can’t come up with one concrete example? That’s a red flag.

| Step | Description |
|---|---|
| Step 1 | Notice exhausted residents |
| Step 2 | Ask about rotation demands |
| Step 3 | Talk with multiple residents |
| Step 4 | Consider major red flag |
| Step 5 | May be service specific |
| Step 6 | Lower on rank list |
| Step 7 | Weigh with other factors |
| Step 8 | One time or pattern? |
| Step 9 | Same story from most people? |
The Gaslighting Problem: “You’re Just Sensitive”
Here’s the part that messes with your head.
Medicine has a long history of dismissing legitimate concerns as weakness. You say, “People look exhausted,” and someone hits you with, “This is what you signed up for,” or “We all survived it.”
That doesn’t mean you’re wrong. It just means the culture is defensive.
You’re not weak because you noticed the senior almost fell asleep sitting at the workstation.
You’re not soft because you think routinely working 28 hours with no real break might be…not great for patient safety.
You are literally the only one in that room who isn’t already normalized to this system. Your fresh eyes are actually valuable. You’re seeing what they’ve learned to accept.
If anything, the danger isn’t that you’re overreacting now. It’s that in 2–3 years, you won’t react at all when you absolutely should.
The Future of Medicine vs. What You Just Saw
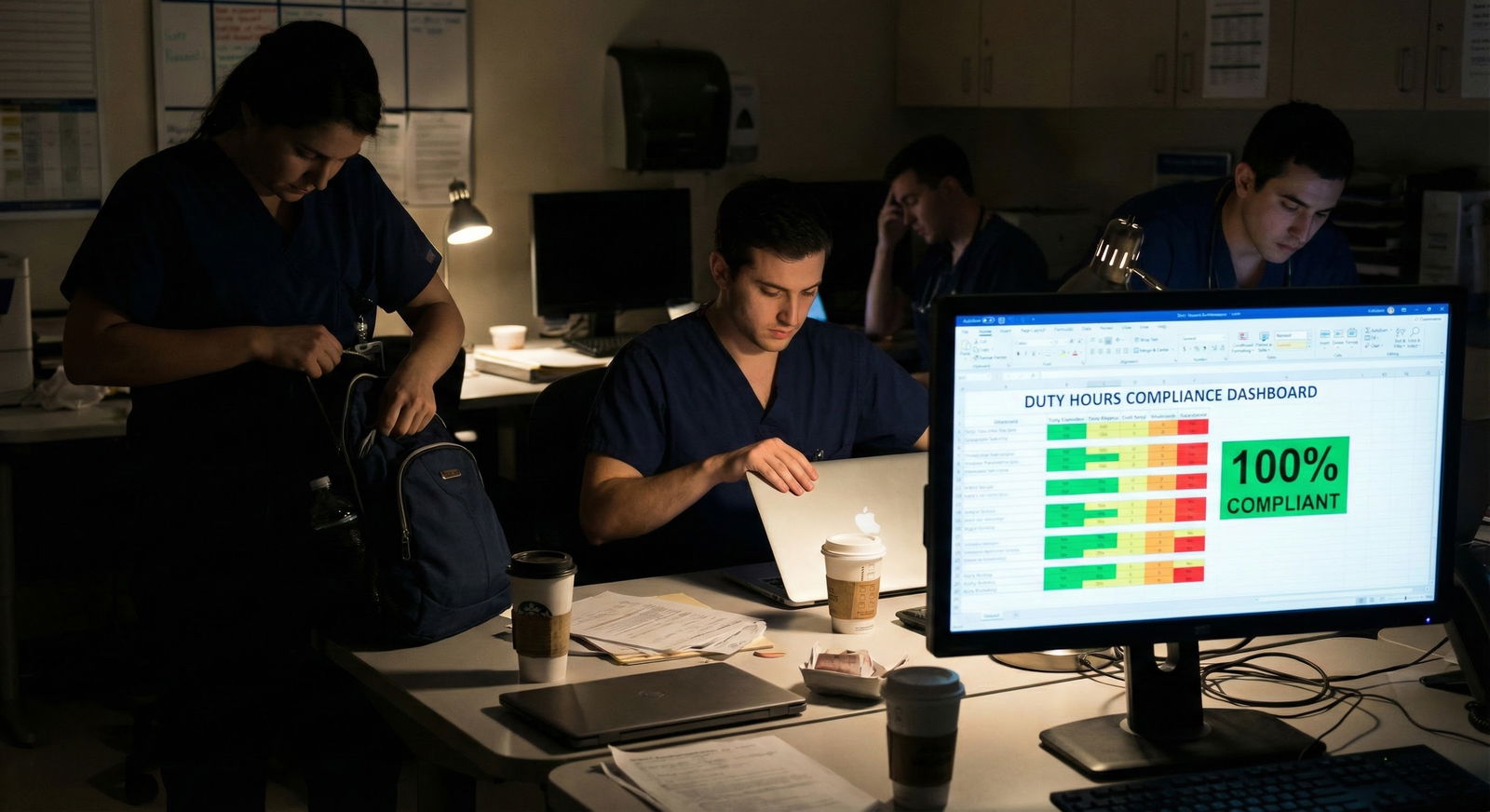
You keep reading about “resident wellness,” “protected time,” and “culture change,” and then you rotate at a place where the senior quietly tells you, “Don’t log all your hours or we’ll get in trouble.”
Two different worlds.
The reality is: some programs are genuinely trying to move into the future. Some have barely left 1995.
You can often tell which is which by looking at how they talk about change.
Future‑leaning programs:
- Admit flaws openly: “We used to be brutal. We’re not perfect, but here’s what we’ve changed.”
- Have recent adjustments: schedule restructures, cap changes, night float implementation, new support staff.
- Let residents speak freely in closed rooms without faculty glaring in the corner.
Stuck‑in‑the‑past programs:
- Act insulted when you ask about workload.
- Say, “We follow ACGME hours,” like that’s the pinnacle of wellness.
- Give vague answers like, “Our residents are very resilient.”
Resilience is not a wellness strategy. It’s a coping mechanism.
How Much Exhaustion Is “Acceptable” Before You Should Run?
You’re never going to find a program where everyone looks fully rested and spiritually fulfilled at 5 a.m. on a call month. That’s fantasy.
So what’s an actual line in the sand?
Here’s my personal one:
I get worried—not mildly, but truly worried—when all of these are true:
- Multiple residents, across different years, look drained every day you see them.
- When you ask “How’s the program?” they pause, look away, and say something like “It’s…fine,” with that flat tone.
- No one can name specific, recent positive changes.
- There’s a weird tension when faculty are around, like everyone is on guard.
- Jokes are bitter, not light. “We’re all dead inside haha” said 20 times a day isn’t actually funny.
If I see that pattern, I don’t care how shiny the fellowship match list is. I’d rank that place low. Because yes, you might match into something prestigious, but at what cost?
This isn’t undergrad. You don’t get a do‑over.
You’re Not Overreacting. You’re Finally Paying Attention.
You’re not wrong to be unsettled by what you saw. You’re just early in the process of realizing that not all residency programs are created equal, and “being tired” can mean a lot of different things.
So here’s where I land:
- Noticing exhausted residents is normal.
- Worrying that it might be a red flag is smart.
- The key is to look for patterns, listen to how people talk about their experience, and see how leadership responds to reality.
If you walk away from a place and can’t shake the sense that something was deeply off? Trust that. You don’t owe any program the benefit of the doubt at the expense of three to seven years of your life.

FAQ: Six Anxiety‑Soaked Questions You’re Probably Asking
1. If I see exhausted residents on one rotation, should I immediately cross the program off?
No. One rotation is a snapshot, not a documentary. Certain months (ICU, wards, trauma) are notoriously brutal almost everywhere. Instead of crossing it off immediately, talk to residents from other services, ask about elective months, ask if what you saw was typical or a known rough patch. If residents elsewhere in the program seem okay and acknowledge, “Yeah, that month sucks, but it’s limited,” I’d pause before throwing the whole program out.
2. What if residents say “we’re tired but it’s worth it”—can I trust that?
Usually, yes. That’s what good struggle looks like. They’re telling you there’s meaning, support, and growth behind the exhaustion. Listen for how they say it. If it sounds genuine and they can tell specific stories about good teaching, supportive chiefs, fair responses when things get unsafe—that’s different from a hollow “it’s worth it” with dead eyes. Same words, totally different reality.
3. I’m scared to ask about hours because I don’t want to be labeled weak. What do I do?
Reframe the question around patient care and education. Instead of “How many hours do you really work?” try, “How does your schedule balance service with education?” or “What does a tough week look like here?” or “How often are you at or over 80 hours, and how does the program respond when that happens?” You’re asking as a thoughtful future colleague, not a complainer. Programs that get defensive at that? Big nope.
4. Residents told me, ‘Don’t tell anyone we talked about this.’ Is that a huge red flag?
Yes. That screams fear of retaliation and a toxic culture. Normal programs don’t need their residents to whisper about conditions like they’re plotting a prison break. If multiple people, independently, are warning you not to repeat things they’ve said—that’s enough for me to drop that program significantly on my list, no matter what else is good on paper.
5. What if every program I see has exhausted residents? Is this just what I signed up for?
Every program has some level of fatigue. But they should vary in tone. Some will feel heavy and brittle. Others will feel busy but strangely alive. Pay attention to your internal ranking of “I could tolerate this” vs “I feel sick imagining being on this schedule.” If literally every place feels like the latter, talk to mentors you trust and be brutally honest with yourself about specialty, environment, and your limits. That’s not weakness. That’s self‑preservation.
6. I can’t stop replaying what I saw at one program. How do I know if it’s intuition or anxiety?
Ask yourself: what exactly is replaying? A single overworked intern? Or a persistent theme—same dead‑eyed look, same bitter comments, same lack of support across multiple people? Anxiety is vague and fuzzy; intuition usually has receipts. Write down specifically what you saw and heard. If, on paper, it reads like a pattern of disrespect, chronic overwork, and resignation…believe yourself.
Today, do one concrete thing:
Open a note on your phone or laptop and write down, in brutal detail, what you actually saw and heard at that program that made you uneasy. No censoring, no “maybe I’m overreacting.” Just facts and quotes.
Then look at that list tomorrow with fresh eyes. Ask yourself: “If a friend showed me this about their potential program, what would I tell them?”






















