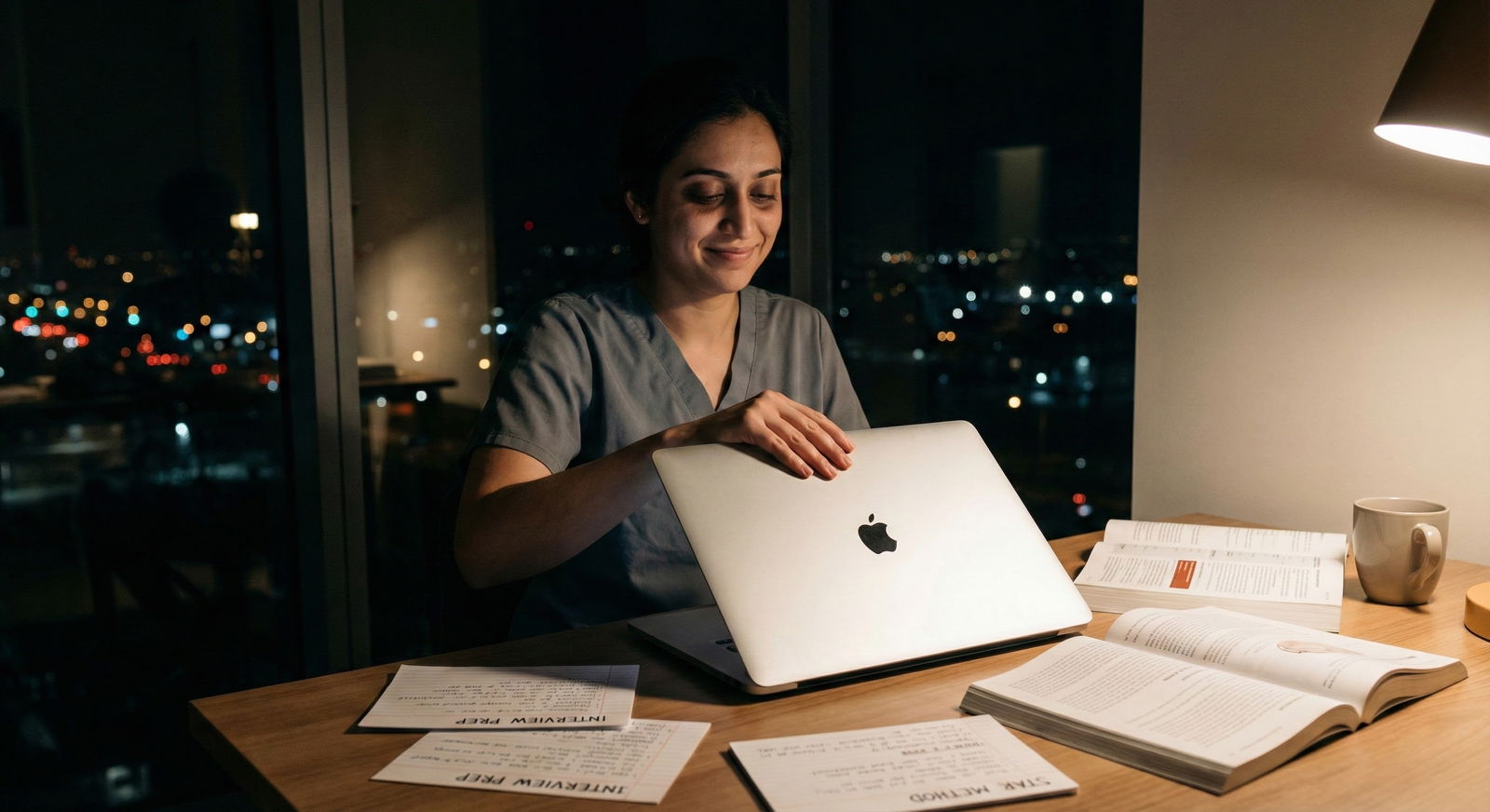
It’s 10:47 pm the week before your first residency interview.
You’re staring at a list of behavioral questions:
- “Tell me about a time you failed.”
- “Describe a conflict with a team member.”
- “Tell me about a time you showed leadership.”
And your brain is doing that awful thing where it tells you:
“I got… nothing. I’ve never saved a crashing patient alone. I’ve never led a disaster response. I’ve never had some movie-level ethical dilemma. I’m screwed.”
Let me say this clearly: you are absolutely not screwed. But I know exactly why it feels like you are.
The Big Fear: “My Life Isn’t Dramatic Enough”
Here’s the anxious loop a lot of us get stuck in:
You watch those “how to answer behavioral questions” videos or read Reddit threads where people talk about:
- De-escalating a violent patient
- Discovering a major medical error and saving the day
- Leading a massive QI project that transformed the hospital
And you think:
“Cool. Meanwhile the worst thing that’s happened to me is my attending yelling at me on rounds and that one time I forgot to order a lab. Who’s going to rank me highly with that?”
Here’s the quiet truth programs won’t put on their website but you need to hear:
Most residents they rank highly do not have dramatic, cinematic stories. They have normal, slightly messy, very human stories—and they tell them clearly.
You don’t need drama. You need clarity. And honesty. And some structure.
That’s it.
What Behavioral Questions Are Actually Testing
Behavioral questions are not a contest for “most traumatic anecdote.”
They’re testing a few very specific things:
- How you think under pressure
- Whether you can reflect on your own behavior
- If you take responsibility or blame others
- Whether you learn from your mistakes
- If you’re going to be unbearable at 3 am on nights
Notice what’s missing from that list:
“Has this person almost died / saved a life / had a TV-worthy moment?”
Programs already know your clinical exposure is limited. You’re a student. Not a fellowship-trained trauma surgeon. They’re not expecting you to have flown a helicopter into a hurricane to rescue a NICU.
What they care about is: can you handle everyday medicine without falling apart or making everyone around you miserable?
So yes, that low-key story about miscommunicating with a nurse and fixing it? That’s fair game. That time you got harsh feedback, felt crushed, and then changed your approach? Absolutely usable.
Why “Small” Stories Usually Work Better Anyway
Counterintuitive thing I’ve seen over and over: the “huge” stories often go badly in interviews.
Here’s why:
Big, dramatic stories are risky because:
- They can sound braggy or performative
- They often lack nuance (you become “the hero”)
- They tempt you to focus on the event instead of your thought process
- They make interviewers silently think: “Is this… actually true?”
Smaller stories are often stronger because:
- They feel real and believable
- They show day-to-day functioning, which is what residency is
- They’re easier to walk through step-by-step
- You can clearly highlight growth, reflection, and insight
I’d take this answer any day:
“I miscommunicated sign-out on a patient, the team got confused, I owned the mistake, clarified the plan, and then changed how I structure my sign-out going forward”
over:
“I single-handedly resuscitated a crashing patient when the whole team froze.”
Programs want someone safe, teachable, and self-aware. Not someone trying to impress them with hero folklore.
You Probably Have More Stories Than You Think
Right now your brain is saying: “No I don’t. I seriously don’t.”
So let’s prove it wrong.
Here are areas where you almost certainly have usable stories, even if they feel “boring” to you:
- Third-year clerkships drama (plenty of interpersonal conflict there)
- Times you messed something up: orders, notes, communication
- Group projects: research, QI, student orgs
- Non-clinical jobs: barista, tutor, scribe, EMT, CNA, tech
- Pre-med stuff: volunteering, leadership positions
- Life outside medicine: family issues, sports, music, caregiving
You don’t need one story per question. You need maybe 6–8 versatile stories that can be repurposed.
Build Your “Story Bank”
Take 30–45 minutes and list experiences under these buckets:
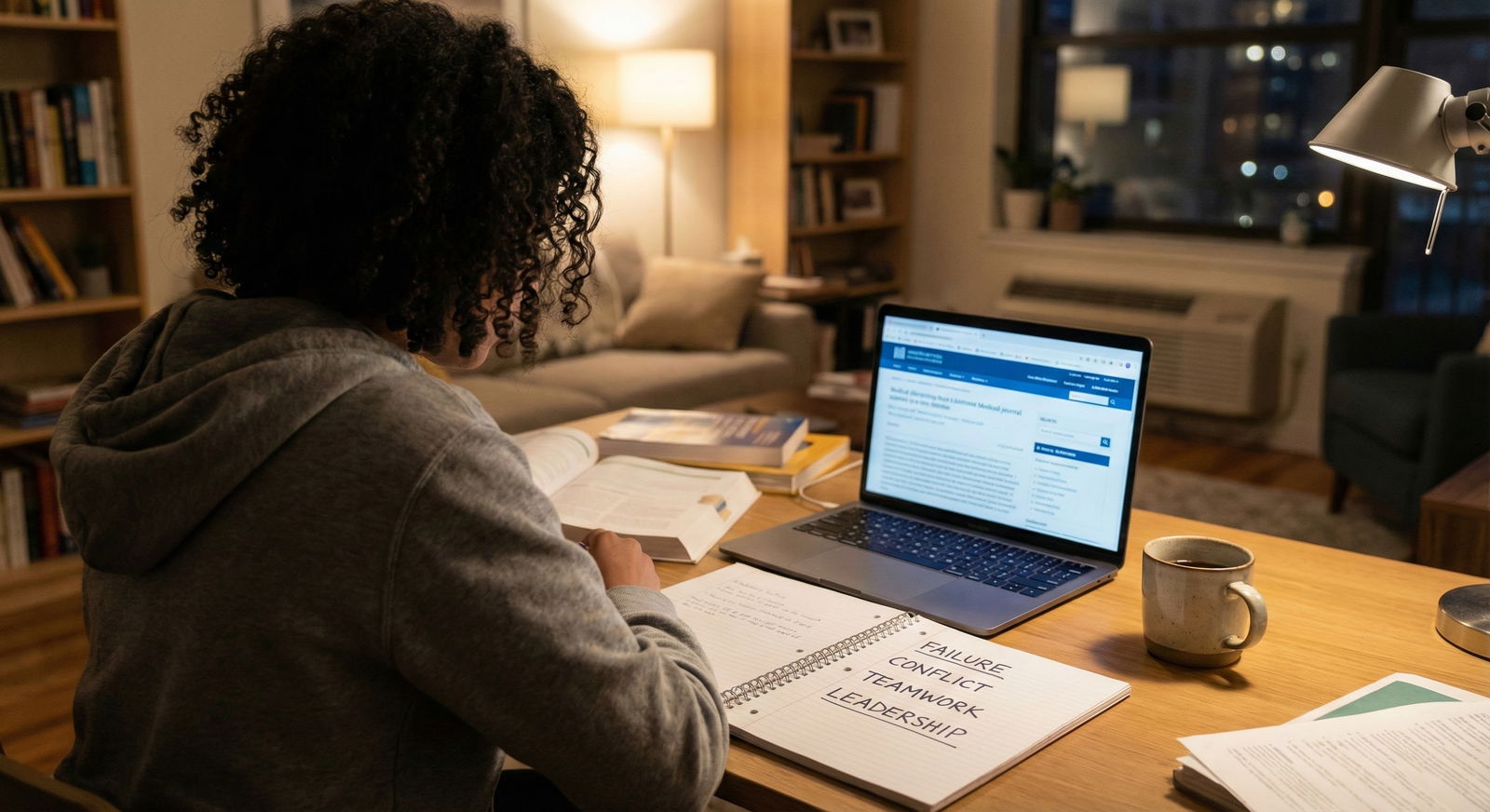
- A time you failed / made a mistake
- A conflict with a peer, nurse, resident, or attending
- A time you had to advocate for a patient
- A time you got tough feedback
- A time you led something (even small)
- A time you had to manage stress / burnout
- A time you adapted quickly to a change or crisis
- A time you worked with a difficult personality
You can reuse the same story across categories with different emphasis. That’s normal.
For example, one story about a miscommunication with a nurse could become:
- “Tell me about a conflict.”
- “Tell me about a mistake.”
- “Tell me about a time you learned something from a colleague.”
- “Tell me about a time you had to rebuild trust.”
It’s not cheating. It’s being prepared.
How To Turn A “Boring” Story Into A Strong Answer
The structure saves you. Not the drama.
Use a simple format: STAR or CAR. I don’t care what you call it as long as it’s structured.
Let’s use STAR (Situation, Task, Action, Result), but keep it human:
- Situation – brief context
- Task – what you were responsible for
- Action – what you did (your thought process)
- Result – what happened + what you learned
Example. Take a very average story: forgot to follow up a lab.
Here’s the anxious inner monologue: “That’s too small. They’ll think I’m incompetent.”
Here’s how you’d actually frame it:
Question: “Tell me about a time you made a mistake.”
Answer (condensed):
“On my medicine rotation, I was following a patient with suspected GI bleed. I was responsible for tracking their hemoglobin trend and updating the team each morning.
One day, the morning labs were delayed, and when they finally came in, I saw the hemoglobin had dropped more than expected. I got distracted helping with another admission and didn’t immediately notify the resident. During rounds, the attending asked about that patient, and it became clear I hadn’t flagged the change quickly.
I owned that I’d seen the lab and hadn’t prioritized communicating it. After rounds, I apologized to the resident, and we discussed how we could systematize lab checks. I set up a personal checklist for pre-rounding where critical labs were highlighted, and if anything crossed a threshold, my next step was to page the resident before doing anything else.
Since then, I’ve been more deliberate about pausing and asking, ‘Is there anything here that changes management right now?’ before moving on. It was a relatively small delay with no harm to the patient, but it was a good wake-up call about how small lapses in communication can add up.”
No drama. No crashing patient. No hero moment.
But:
- You showed ownership
- You didn’t blame “the system” or “the resident”
- You demonstrated adaptation and learning
- You showed you understand safety culture
That’s exactly what they want.
What Interviewers Care About But Won’t Say Out Loud
Most interviewers are thinking three things in behavioral questions:
- Will this person be safe with patients?
- Will this person be tolerable to work with?
- Does this person have a functioning guilt–insight–growth circuit?
They’re less interested in:
- Whether your story sounds impressive
- Whether it’s the “most intense” thing they’ve heard that day
They’re watching for red flags:
- You never take responsibility. It’s always someone else’s fault.
- You throw other people under the bus. Constantly.
- You tell some ultra-dramatic story and clearly haven’t reflected on it.
- You seem proud of something ethically questionable.
- You sound rehearsed to the point of fake.
That last one? Huge. Over-polished, “perfect” answers make people uneasy.
A slightly awkward, honest story about a very normal mistake is far safer.
What If You Actually Haven’t Had Much Clinical Conflict Or Failure?
Another fear:
“I got along with everyone. I never had a major conflict. I never majorly screwed anything up. Now what?”
Conflict doesn’t have to mean screaming matches. It can be:
- Disagreement with a teammate about a plan
- Different communication styles that caused friction
- You feeling dismissed or overlooked
- A subtle tension you had to address
Failure doesn’t have to mean catastrophic. It can be:
- Shelf exam that didn’t go well
- Research project that stalled
- Leadership position where you under-delivered
- Time management meltdown on a rotation
You’re not being “dramatic” by calling those things failure or conflict. You’re being honest that they were challenges for you at the time.
If you truly had a low-conflict environment (lucky you), pull from:
- Preclinical group projects
- Volunteer roles
- Non-medical jobs
- Even family dynamics, if you can present them professionally and briefly
You’re showing patterns of behavior. That’s what interviewers are mapping. Not just “on the wards.”
Practicing Without Sounding Like A Robot
Here’s where anxiety usually spikes:
“If I practice these, I’ll sound fake.”
You’ll sound fake if you memorize full paragraphs.
You’ll sound prepared if you:
- Jot down bullet-point skeletons for each story: situation, 1–2 key actions, 1–2 takeaways
- Practice out loud, but let the exact words change each time
- Focus on the beats of the story, not exact phrasing

| Category | Value |
|---|---|
| Story selection | 25 |
| Structuring answers | 25 |
| Out-loud practice | 30 |
| Mock interviews | 20 |
The goal: your answers feel like a story you’ve told before, not like a script you’re reading in your head.
Do a couple low-stakes mock runs:
- With a friend who’s not in medicine (they’re great for “does this make sense?” checks)
- With a classmate who’s also interviewing
- Even just recording yourself on your phone and listening back once
You’ll hear where you ramble, where you undersell yourself, and where you sound wooden.
How To Handle The Panic Moment In The Actual Interview
You will get at least one question that throws you off. Guaranteed.
The fear is: “If I pause, they’ll think I’m clueless.”
No. A 3–5 second pause with:
“Let me think for a second—that’s a good question.”
makes you look thoughtful, not clueless.
If your brain blanks, mentally scan your short list: failure, conflict, leadership, stress, feedback. Ask yourself: “Which of my 6–8 stories is even loosely related to this?” Then adapt one.

| Step | Description |
|---|---|
| Step 1 | Hear Question |
| Step 2 | Pick Closest Story |
| Step 3 | Pause 3-5 sec |
| Step 4 | Identify If Its Failure/Conflict/Leadership/Teamwork |
| Step 5 | Use STAR Structure |
| Step 6 | End With Takeaway/Learning |
| Step 7 | Recognize Type? |
You will feel like the pause is 10 years long. It’s actually 2 seconds. Interviewers are used to it.
What does look bad is blurting the first half-baked thing that pops into your head and then cornering yourself.
Short pause > panicked ramble. Every time.
Quick Reality Check: You vs. Everyone Else
You’re imagining everyone else showing up with these polished trauma stories and you sitting there like, “Once I ran out of printer paper before clinic.”
Let’s be blunt. Most applicants:
- Are recycling the same 4–5 stories
- Are also scared their stories aren’t good enough
- Are also shaky on structure
- Also feel like impostors
You’re not behind because you lack dramatic content. You’d be behind if you:
- Blame others in every story
- Can’t identify what you learned
- Or insist “I’ve never failed” (big red flag answer, by the way)
If you can:
- Admit imperfection
- Show growth
- Talk like a real person and not a PR statement
—you’re already ahead of more applicants than you think.

| Category | Value |
|---|---|
| Blaming others | 30 |
| No reflection | 25 |
| Overly vague | 20 |
| Over-rehearsed | 15 |
| No clear action taken | 10 |
Example “Normal” Stories You Can Adapt
Just to calm that “I have nothing” voice, here are some very ordinary things that can make excellent answers:
- You struggled with time management on surgery, constantly running behind on pre-rounding, then built a checklist/system and sought advice from a senior.
- You had a miscommunication with a nurse who felt you were dismissive; you reflected, apologized, and changed how you present yourself.
- You studied the wrong way for your first shelf, did poorly, then completely restructured your approach and improved on subsequent exams.
- You were in a research team where two members weren’t pulling their weight; you initiated a meeting, clarified expectations, and redistributed tasks.
- You felt burned out, started dreading clinical days, and actually did something about it: talked to a mentor, set boundaries, adjusted your coping strategies.
None of that is Netflix-drama-level content. All of that is residency-relevant.
| Story Type | Competencies Shown |
|---|---|
| Miscommunication with nurse | Teamwork, humility, communication |
| Poor performance on shelf | Resilience, growth mindset |
| Time management issues on wards | Organization, accountability |
| Low-effort group member in project | Leadership, conflict resolution |
| Burnout and seeking help | Insight, self-care, professionalism |

FAQs
1. What if all my “failure” stories make me look incompetent?
Then you’re telling them wrong.
The failure itself usually isn’t the problem unless it’s something wild (huge professionalism violation, repeated safety issues). It’s how you frame it.
If your story sounds like: “I failed this thing, it was sad, anyway next question,” that’s bad.
If it sounds like: “Here’s what I did wrong, what I realized, and what I changed that still affects how I work now,” that’s exactly what they want. Focus 30% on the failure, 70% on the response and long-term change.
2. Can I reuse the same story for multiple behavioral questions?
Yes. Quietly, everyone does.
You just shift the angle. Same basic event, different emphasis. For “conflict,” your focus is the interpersonal dynamic. For “leadership,” your focus is how you organized others. For “failure,” your focus is your mistake and growth.
Recycling the same 6–8 solid stories is smarter than forcing 20 weak ones.
3. Is it bad if my stories are mostly from before clinical rotations?
Not ideal, but not fatal.
Programs prefer clinical stories because they’re closer to what you’ll be doing as a resident, but if your best examples are from research, previous work, or pre-clinical time, use them—just tie them back to how they affect you clinically now.
If you can, at least have 2–3 stories from third- or fourth-year rotations. Even if they’re small.
4. Should I avoid talking about mental health, burnout, or personal struggles?
You don’t have to completely avoid them, but be careful with framing.
If your whole story is “I was non-functional and did nothing until I failed out,” that’s concerning. If your story is, “I was struggling, I recognized it, I reached out, and here’s how I function better now,” that shows insight and maturity.
Keep personal mental health details at a professional level of disclosure, but don’t pretend you’re a robot who’s never struggled.
5. What if I blank completely and can’t think of any story in the moment?
Happens.
Take a breath. Say: “I’m just going to take a second to think of a good example.” Give yourself 5–10 seconds. If nothing comes, you can say:
“I’m having trouble pulling up a perfect example under pressure right now, but a smaller situation that comes to mind is…”
And pick something modest. Interviewers know nerves scramble memory. They care more about how you handle the stumble than whether your story is incredible.
If you remember nothing else, remember this:
- You are not being judged on how dramatic your life is.
- Ordinary, honest stories told clearly and thoughtfully beat flashy, shallow ones every time.
- A small set of well-prepared, flexible stories is enough to carry you through behavioral questions.
Your life doesn’t have to be a movie. It just has to be real—and you have to be willing to talk about it.