
Understanding the Landscape: Emergency Medicine, J‑1 Visas, and the 49th & 50th States
Emergency medicine residency in the United States is uniquely appealing to many international medical graduates (IMGs). The specialty’s broad scope, high acuity, and procedural intensity make it a powerful career path, and programs in geographically distinct states like Alaska and Hawaii add lifestyle and mission-driven appeal.
However, for IMGs training in the U.S. on a J‑1 visa, long-term practice planning requires early attention to immigration options—especially the J‑1 waiver. For those drawn to an emergency medicine residency in Alaska or Hawaii, the interplay between the EM match, state-level Conrad 30 programs, and underserved area waiver options can be both promising and complex.
This guide walks through:
- How J‑1 sponsorship intersects with emergency medicine residency
- The basics of the J‑1 home-residency requirement and waiver options
- The specific J‑1 waiver structures in Alaska and Hawaii
- Practical strategies to position yourself for an EM career in these states
- Actionable timelines and tips for the EM match and post‑residency planning
Throughout, the focus is on J‑1 waiver strategies tailored to emergency physicians who want to train or practice in Alaska and Hawaii.
J‑1 Visa Fundamentals for Emergency Medicine Residents
Most IMGs entering an ACGME-accredited emergency medicine residency in the U.S. are sponsored by the Educational Commission for Foreign Medical Graduates (ECFMG) on a J‑1 exchange visitor visa (clinical trainee category).
How the J‑1 Works in EM Residency
Key points relevant to emergency medicine residency:
- Sponsorship: ECFMG is the typical visa sponsor for IMGs in EM; some programs may support H‑1B, but many—especially in smaller or safety-net hospitals—prefer or require J‑1.
- Duration: The J‑1 is granted for the length of the training program (e.g., 3–4 years for emergency medicine), with the possibility of extension for fellowships.
- Return-home requirement: After completing J‑1 clinical training, you are subject to a two-year home-country physical presence requirement (INA 212(e)):
- You must spend a cumulative two years in your country of last legal permanent residence, or
- You must get a J‑1 waiver before you can transition to H‑1B, L‑1, or immigrant (green card) status in the U.S.
Why J‑1 Waivers Matter So Much in Emergency Medicine
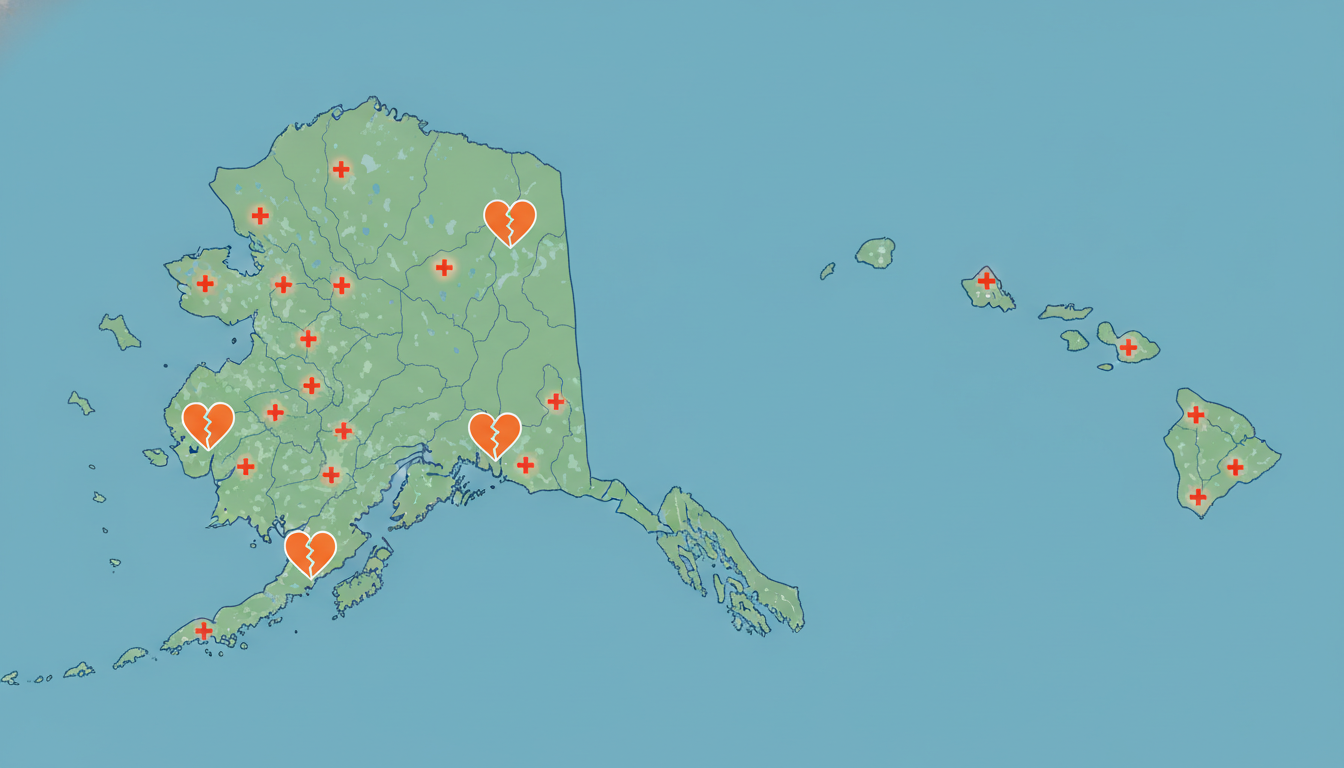
Emergency medicine is almost always practiced in a hospital or urgent care setting. Many emergency departments that rely on J‑1 physicians are in:
- Rural hospitals
- Small island or frontier communities
- Urban safety‑net hospitals
These are often designated as medically underserved areas (MUA) or health professional shortage areas (HPSA)—key concepts because many J‑1 waivers, including the Conrad 30 program, are tied to service in such locations.
For an IMG interested in practicing emergency medicine in Alaska or Hawaii after residency, a well-planned J‑1 waiver strategy can allow you to:
- Waive the two-year home residency requirement
- Work in an underserved community where EM physicians are badly needed
- Start a longer-term path to permanent residence (if desired)
Core J‑1 Waiver Options: What EM Physicians Need to Know
Multiple pathways exist to waive the J‑1 home-residency requirement. For emergency physicians targeting Alaska residency or Hawaii residency programs, the following are the most relevant.
1. Conrad 30 Program (State-Based Underserved Area Waiver)
The Conrad 30 J‑1 waiver program is usually the centerpiece of strategies for J‑1 physicians finishing residency. Every U.S. state and certain territories can sponsor up to 30 J‑1 waivers per fiscal year for physicians who commit to work in designated shortage areas.
Key features:
- Requirement: Minimum 3-year, full-time employment (usually 40 hours/week) in a qualifying site.
- Location: Typically in a HPSA, MUA, or serving a Medically Underserved Population (MUP).
- Flexibility: Some states use “flex” slots to allow placements at sites outside formal shortage-designated areas if the population served is underserved.
Why this matters for emergency medicine:
- Many rural EDs and safety‑net hospitals in Alaska and Hawaii qualify for Conrad 30.
- Some state programs are especially open to hospital-based specialties, including EM, because of severe workforce shortages.
2. Federal Government Agency Waivers (VA, DoE, etc.)
Several federal agencies can also sponsor J‑1 waivers, such as:
- Veterans Health Administration (VA)
- Department of Health and Human Services (HHS)
- Department of Defense (DoD)
Pros:
- Not limited by the state’s “30 slot” cap.
- Some may support hospital-based positions.
Cons:
- Criteria can be narrow and may not always align with emergency medicine openings in Alaska or Hawaii at the time you finish training.
- Application processes can be lengthy and sometimes less predictable.
3. Hardship and Persecution Waivers
These are more individualized:
- Exceptional Hardship Waiver: If leaving the U.S. or being forced to return home will cause exceptional hardship to a U.S. citizen or permanent resident spouse or child.
- Fear of Persecution Waiver: If you would face persecution in your home country based on race, religion, or political opinion.
They do not rely on working in an underserved area and can, in theory, be combined with any job offer. However:
- The evidentiary burden is high.
- Processing times can be long.
- Often pursued with the help of specialized immigration counsel.
For most emergency medicine IMGs looking specifically at Alaska and Hawaii, the main practical option is still the Conrad 30 underserved area waiver route.
Alaska & Hawaii: EM Programs, Waiver Ecology, and System Realities
Emergency Medicine Residency and Practice in Alaska
As of the current landscape, Alaska typically has:
- Limited or no in-state, fully-accredited stand-alone emergency medicine residency programs compared to the continental U.S.
- Strong reliance on visiting EM physicians, locums, and telehealth support.
- A healthcare system with:
- Large geographic distances
- Severe weather constraints
- Many critical access hospitals and small EDs
- Significant Alaska Native and rural populations
For IMGs, this means:
- You will likely complete emergency medicine residency outside Alaska, then seek a J‑1 waiver job in Alaska after training.
- The state’s workforce shortages can make Alaska an especially receptive environment for Conrad 30 and other underserved area waiver placements.
Emergency Medicine Residency and Practice in Hawaii
Hawaii has:
- A smaller number of residency programs overall, often centered in Honolulu.
- A mix of:
- Academic medical centers with high-acuity EDs
- Community hospitals on outer islands
- A need for emergency physicians in both urban safety‑net and rural island contexts.
In terms of the EM match:
- Most IMGs matching into emergency medicine in Hawaii do so through mainland or local programs willing to sponsor J‑1 visas.
- After EM residency, Hawaii’s geography (many isolated islands) and tourism-based economy create sustained demand for EM physicians, especially in underserved or smaller island hospitals.
For J‑1 waiver strategy, Hawaii’s Conrad 30 spots can be appealing if:
- You enjoy cross‑cultural care and complex emergency presentations.
- You’re willing to live outside the main urban centers, or
- You’re interested in joining safety‑net hospitals and trauma-capable centers serving diverse and underserved populations.

State-Specific J‑1 Waiver Strategies: Alaska vs. Hawaii
While both states participate in the Conrad 30 program, their size, needs, and administrative cultures differ. The details change periodically, so always verify with each state’s current guidelines, but the general strategic principles are stable.
1. Alaska J‑1 Waiver Strategy for Emergency Physicians
A. Demand Signal
Alaska faces chronic shortages in:
- Emergency medicine
- Primary care
- Psychiatry
- Other frontline specialties in small hospitals
Many communities are reachable only by air, boat, or seasonal roads. This makes recruitment and retention of EM physicians challenging and increases receptiveness to J‑1 waiver placements.
B. Typical Alaska Conrad 30 Priorities
While the priority list can shift, Alaska tends to favor:
- Physicians willing to work in rural or frontier settings
- Service to Native Alaska and other underserved communities
- Physicians with strong commitment to long-term practice in the state
Emergency medicine is often viewed favorably because practically every hospital must maintain ED services to ensure community viability.
C. Strategic Moves for Alaska-Oriented IMGs
During EM Residency (PGY-1 to PGY-2)
- Seek rural or resource-limited EM rotations (e.g., away rotations or electives in frontier-style ED settings).
- Build a procedural and systems-based care profile that suits low-resource contexts (airway management with minimal backup, trauma stabilization, telehealth, etc.).
- Attend virtual or in-person conferences where Alaska hospital recruiters and medical directors participate.
Mid-Residency (PGY-2 to early PGY-3)
- Start investigating Alaska hospital systems known to sponsor J‑1 waivers.
- Network with EM attendings who have done locums or permanent work in Alaska.
- Clarify with potential employers:
- Whether they have previously used Conrad 30 or other waivers.
- Their comfort with sponsoring a position in an underserved area waiver context.
Late Residency (PGY-3 and beyond)
- Align your job search timeline to meet Alaska’s Conrad 30 application period. Some states:
- Open applications at the start of the federal fiscal year (October 1).
- Use a first-come, first-served model or prioritize shortage specialties.
- Confirm that:
- The ED site is in a qualified HPSA/MUA, or can be justified under a flex slot.
- The employer has the infrastructure to support the 3-year contract requirement (full-time, usually 3–4 shifts/week depending on contract terms).
- Align your job search timeline to meet Alaska’s Conrad 30 application period. Some states:
Document Your Commitment
- Letters of intent, statements in your application, and employer attestations that highlight your long-term commitment to Alaska’s frontier health system are often viewed positively by state health departments.
2. Hawaii J‑1 Waiver Strategy for Emergency Physicians
A. Demand Signal
Hawaii’s needs include:
- EM physicians for rural island hospitals (e.g., on Maui, Kauai, Hawaii Island, and other outer islands)
- EM coverage for safety‑net hospitals and busy urban EDs
- Physicians comfortable with:
- Multi-ethnic, multilingual patient populations
- Tourists and transient visitors with limited follow-up
B. Typical Hawaii Conrad 30 Priorities
Hawaii may prioritize:
- Placement in rural or surgeon/EM-scarce communities
- Service to Native Hawaiian and Pacific Islander populations
- Hospital-based specialties that can maintain 24/7 emergency services
C. Strategic Moves for Hawaii-Oriented IMGs
During EM Residency
- Emphasize cultural competence and language skills (e.g., Asian, Pacific, or other languages common among Hawaii residents and visitors).
- Seek exposure to:
- Island or coastal EDs (if available)
- Trauma and marine-related emergencies
- Participate in or research global/international EM or cross-cultural care topics; this can align with Hawaii’s multicultural environment.
Connecting Early With Hawaii Employers
- Identify hospital systems on outer islands (and in Honolulu) that historically sponsor J‑1 waiver positions.
- Reach out to:
- Medical directors of EDs
- Physician recruiters
- Faculty in Hawaii-based EM or combined programs
- Ask directly:
- “Have you sponsored J‑1 waivers (Conrad 30) for emergency medicine before?”
- “Are your ED sites within HPSAs/MUAs or eligible flex slots?”
Timing and Application Strategy
- Monitor Hawaii’s public health department website for:
- Opening dates of the Conrad 30 application cycle
- Specialty preference lists
- Document requirements (contracts, letters, site designations)
- Ensure your job offer:
- Is clearly full-time, 3-year minimum.
- Specifies your ED duties and role across satellite sites, if any.
- Meets any state-specific minimum hours or on-call coverage standards.
- Monitor Hawaii’s public health department website for:
Positioning EM as an Underserved Asset
- In supporting letters, emphasize how your emergency medicine skillset:
- Stabilizes critically ill patients in low-resource island hospitals.
- Reduces the need for costly medevac transfers by handling more cases locally.
- Improves 24/7 coverage for underserved populations who rely on EDs as their primary care access.
- In supporting letters, emphasize how your emergency medicine skillset:
EM Match, Visa Choices, and Long-Term Planning
During the EM Match: Choosing Programs With J‑1 Flexibility
When selecting emergency medicine residency programs—whether in continental U.S., Alaska (if available), or Hawaii—it’s crucial for IMGs to:
Confirm Visa Policies
- Does the program accept IMGs on J‑1?
- Are they open to H‑1B sponsorship (if you want to avoid J‑1 waivers entirely)?
- Ask program coordinators or GME offices directly.
Assess Graduate Outcomes
- How many prior residents were IMGs on J‑1 visas?
- Where did they go after graduation?
- How many obtained J‑1 waivers (Conrad 30, VA, etc.)—and in which states?
Consider Geographic Ties
- If your long-term goal is an Alaska residency equivalent experience (practice after mainland residency) or to join Hawaii residency programs and stay locally, develop ties early:
- Electives or rotations in Alaska/Hawaii if possible
- Research or quality improvement projects linked to these regions
- Mentorship from faculty with ties to the Pacific Northwest, Pacific Islands, or Arctic/frontier care
- If your long-term goal is an Alaska residency equivalent experience (practice after mainland residency) or to join Hawaii residency programs and stay locally, develop ties early:
J‑1 vs H‑1B for EM Residents Targeting Alaska & Hawaii
If you have an option between a J‑1 and an H‑1B:
J‑1:
- Pros: Simpler for many programs; widely used; predictable ECFMG framework.
- Cons: Mandatory home-country 2-year requirement unless a waiver is obtained; requires careful J‑1 waiver planning for Alaska and Hawaii.
H‑1B:
- Pros: No 2-year home residency requirement; can transition directly into practice or further training.
- Cons: Some EM programs do not support H‑1Bs; subject to numerical caps except in cap-exempt institutions; more legal and cost burden on the employer.
For many IMGs, particularly those strongly attracted to rural or underserved ED work, the J‑1 plus Conrad 30 waiver route is not just manageable but can be a planned path into meaningful service in Alaska or Hawaii.
Timeline Overview: From EM Residency to J‑1 Waiver Job
A common sequence for an IMG in emergency medicine:
PGY-1–2
- Focus on core EM skills.
- Confirm program’s J‑1 sponsorship.
- Start exploring Alaska and Hawaii workforce needs.
PGY-2–early PGY-3
- Begin targeted networking with potential Alaska/Hawaii employers.
- Learn each state’s Conrad 30 rules and deadlines.
- Seek letters and mentors who understand your long-term goals.
Mid–late PGY-3 (or final year)
- Secure a job offer at a qualifying ED site.
- Ensure the employer is prepared to:
- File the Conrad 30 application with the state.
- Support the USCIS J‑1 waiver petition.
- Track timelines carefully so waiver approval is obtained before J‑1 end date.
Post-Residency, Years 1–3
- Complete your 3-year full-time service in the underserved area (Alaska or Hawaii ED).
- Maintain licensure, board certification, and strong performance documentation.
- If desired, explore immigrant visa options (e.g., EB-2 NIW, employer-sponsored PERM) in parallel with service.
Practical Tips and Common Pitfalls for EM IMGs
Practical Tips
- Keep Records Organized: Training certificates, evaluations, procedure logs, and proof of work in underserved settings will support both your waiver and future immigration steps.
- Engage With State Health Departments: For Alaska and Hawaii, state-level Conrad 30 coordinators are usually open to questions from physicians and employers; early communication can prevent missteps.
- Align Your CV With Underserved Care:
- Highlight any rural EM experience.
- Include community service, telemedicine, or public health projects.
- Frame your interest in underserved area waiver service as a mission, not just a visa solution.
- Use Professional Immigration Counsel: Particularly when:
- Combining Conrad 30 with other immigration strategies (e.g., green card planning).
- Navigating complex family or previous visa histories.
Common Pitfalls
- Waiting Too Long to Seek a Job: In both Alaska and Hawaii, matching to a great EM residency doesn’t guarantee an easy waiver job later. Start networking and searching during residency, not after.
- Assuming Any Hospital Qualifies: Not all EDs are in HPSAs/MUAs, and flex slots are limited. Verify your prospective site’s designation status early.
- Ignoring Contract Details:
- The waiver contract must usually be full-time, for at least 3 years.
- Changes in employer or site may jeopardize the waiver if not handled correctly.
- Underestimating Cultural and Geographic Realities:
- Alaska’s remote settings can be socially and professionally isolating.
- Hawaii’s cost of living (especially housing) is high. Plan financially.
FAQ: J‑1 Waivers for Emergency Medicine in Alaska & Hawaii
1. Can I do my entire emergency medicine residency in Alaska or Hawaii on a J‑1 visa?
It depends on program availability and sponsorship policies at the time you apply. Historically, IMGs have more commonly completed emergency medicine residency in mainland programs and then moved to Alaska or Hawaii for a J‑1 waiver job. If an EM residency program in Alaska or Hawaii accepts IMGs and is ECFMG-approved for J‑1 sponsorship, you can complete your training there. Always confirm directly with each program.
2. Are Conrad 30 waivers guaranteed for emergency physicians in Alaska and Hawaii?
No. While emergency medicine is often a high-need specialty in both states, Conrad 30 slots are limited and subject to state priorities and timing. Your chances improve if:
- You secure a job at a clearly underserved ED site.
- You apply early in the state’s application cycle.
- Your employer has experience with J‑1 waivers.
3. Can I switch employers during my 3-year J‑1 waiver service in Alaska or Hawaii?
Potentially, but it’s complicated. Changing employers or sites typically requires:
- State health department approval.
- Filing amended petitions with USCIS.
Unauthorized changes can put your waiver and immigration status at risk. Always consult an immigration attorney and the state Conrad 30 coordinator before making changes.
4. What if I want to stay in Alaska or Hawaii permanently after completing my J‑1 waiver service?
Many physicians use their 3-year J‑1 waiver period to start a longer-term immigration pathway, such as:
- Employer-sponsored immigrant visas (e.g., EB-2 with PERM labor certification).
- Self-petitioned routes like EB-2 National Interest Waiver (NIW), if eligible.
If you plan to remain long-term, begin discussing green card strategy with your employer and immigration counsel early in your waiver service, not at the end.
By understanding how the J‑1 waiver, Conrad 30, and underserved area waiver systems operate in Alaska and Hawaii, emergency medicine IMGs can turn visa constraints into a structured path toward meaningful practice in some of the most unique and underserved regions in the United States. Thoughtful planning—beginning in residency and extending through your first years in practice—will position you for both immigration stability and a deeply rewarding EM career in the 49th or 50th state.





















