
Understanding the Landscape: FM Match, Alaska & Hawaii, and J‑1 Status
Family medicine residency in Alaska and Hawaii offers a unique mix of training in frontier, rural, and island medicine—exactly the kind of settings that often align well with J‑1 waiver opportunities. For international medical graduates (IMGs), these states can be particularly strategic when thinking ahead to the three‑year service required for a J‑1 waiver.
Before diving into Alaska residency and Hawaii residency programs specifically, it helps to clarify the key concepts:
- FM match: Refers to entering a family medicine residency through the NRMP Match. For IMGs, this usually means an ECFMG‑sponsored J‑1 visa.
- J‑1 waiver: A process that allows physicians who trained in the U.S. on a J‑1 visa to waive the 2‑year home residency requirement, usually in exchange for 3 years of full‑time work in an underserved or high‑need area.
- Conrad 30: A major J‑1 waiver pathway where each state can sponsor up to 30 waivers per year for physicians agreeing to work in federally designated shortage areas or in high‑need facilities.
- Underserved area waiver: A more general term (often overlapping with Conrad 30) that describes waivers tied to service in Health Professional Shortage Areas (HPSAs) or Medically Underserved Areas/Populations (MUAs/MUPs).
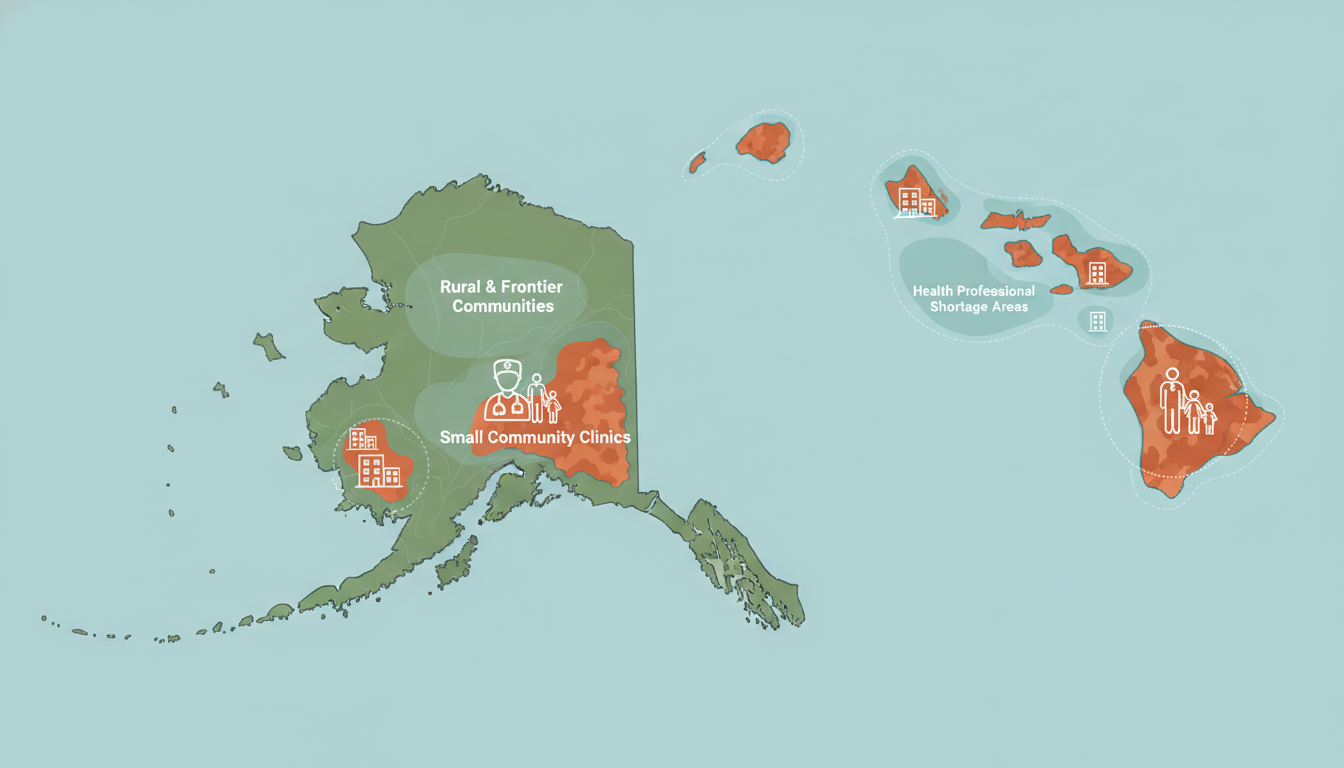
For family medicine, especially in frontier and rural health systems like those in Alaska and Hawaii, the demand for primary care creates relatively favorable conditions for J‑1 waiver jobs. However, the small number of residency programs and limited positions in these states make it important to plan early and understand the regional dynamics.
This guide focuses on J‑1 waiver strategies tailored to family medicine residents and applicants considering training or practice in Alaska and Hawaii.
J‑1 Foundations for Family Medicine Residents
J‑1 Basics for IMGs
Most IMGs in U.S. residency programs train under an ECFMG‑sponsored J‑1 Exchange Visitor visa. Key points:
- Intended purpose: Graduate medical education and training.
- Duration: Typically valid for the length of the residency and fellowship (with annual extensions).
- Two‑year home residency requirement: After completing training, J‑1 physicians must generally return to their home country for at least two years before being eligible for H‑1B or permanent residency—unless this requirement is waived.
For family medicine residents planning to stay in the U.S. after training, securing a J‑1 waiver is crucial.
Main J‑1 Waiver Pathways
The most relevant waiver pathways for family medicine physicians considering Alaska or Hawaii include:
Conrad 30 State Waivers
- Each state can recommend up to 30 waivers per federal fiscal year.
- Usually requires:
- 3‑year full‑time employment contract.
- Employment in a HPSA/MUA/MUP or serving a high‑need population.
- Acceptance of Medicaid/Medicare and sliding fee scales.
- Alaska and Hawaii both participate in the program, but with their own state‑specific priorities and timelines.
Federal Programs (Non‑Conrad)
- Examples include:
- U.S. Department of Health and Human Services (HHS) Clinical Care waivers – limited and specialty‑specific.
- Appalachian Regional Commission (ARC) and Delta Regional Authority (DRA) – not relevant for Alaska or Hawaii geographically.
- For Alaska/Hawaii, federal non‑Conrad paths are usually less common than Conrad 30.
- Examples include:
Hardship and Persecution Waivers
- Based on extreme hardship to a U.S. citizen or permanent resident spouse/child or fear of persecution.
- Complex, heavily case‑specific, and involve immigration attorneys.
- Not typically used as a systematic “career strategy,” and are less tied to geographic location.
For most family medicine graduates aiming to remain in the U.S., Conrad 30 and other underserved area waivers (like certain federal options) are the primary strategic tools.
Alaska: Family Medicine Training & J‑1 Waiver Opportunities
Alaska is one of the most distinctive environments for a family medicine residency. It combines urban training in Anchorage with extensive rural and frontier experiences serving remote communities, Alaska Native populations, and small towns accessible only by plane or boat.
Family Medicine Residency Context in Alaska
Alaska has a limited number of GME programs, including a prominent family medicine residency in Anchorage (aligned with University of Washington/WWAMI). Even if you do not complete your residency in Alaska, it’s possible to pursue your post‑residency J‑1 waiver job there.
Key characteristics of Alaska’s family medicine landscape:
- Heavy emphasis on broad‑scope practice:
- Inpatient and outpatient medicine
- Emergency coverage in smaller communities
- Obstetrics in some locations
- High demand for primary care, particularly in:
- Frontier villages
- Tribal/Native health corporations
- Regional medical centers serving large catchment areas
- Frequent designation as HPSA/MUA, which is favorable for J‑1 waiver placements.
Alaska Conrad 30 Overview
While you should always check the latest guidance on the Alaska Department of Health or state office websites, the following core patterns are typical:
Eligibility:
- Must hold a valid J‑1 status and have completed or be completing residency/fellowship.
- Must have a full, unrestricted Alaska medical license or be license‑eligible.
- Must have an employment offer in a qualifying facility (often FQHCs, tribal health, rural hospitals, or community health centers).
Practice Requirements:
- 3 years of full‑time clinical practice (usually defined as at least 40 hours/week, with a specified portion in direct patient care).
- Serve primarily in HPSA/MUA/MUP or in areas where there is a documented shortage of primary care clinicians.
- Employer must:
- Document recruitment efforts for U.S. citizen/permanent resident physicians.
- Accept Medicaid/Medicare.
- Use a sliding fee scale based on patient income.
Timeline & Application Cycle:
- Alaska, like many states, typically opens applications around the beginning of the federal fiscal year (often October 1), but exact details can change.
- Conrad 30 slots in smaller states like Alaska may not always fill every year, which can be an advantage for family medicine physicians.
J‑1 Waiver Strategy for Alaska: Step‑by‑Step
PGY‑1 to Early PGY‑2: Build the Right Profile
- Focus on excelling in core family medicine rotations, including rural and inpatient experiences.
- If possible, seek electives or away rotations in Alaska or similar frontier settings to:
- Demonstrate interest and adaptability.
- Build connections with Alaska‑based attendings and administrators.
- Get to know the Alaska Native Tribal Health Consortium, regional tribal health organizations, and FQHCs that frequently hire FM doctors.
Mid PGY‑2: Begin Market Research
- Review Alaska’s current Conrad 30 guidelines on the state website.
- Identify health systems that:
- Operate in HPSA or MUA areas.
- Regularly recruit J‑1 physicians (ask program directors, faculty mentors, and alumni).
- Attend virtual job fairs, especially primary care and rural health conferences where Alaska employers recruit.
Late PGY‑2 to Early PGY‑3: Initiate Job Search
- Directly contact physician recruiters at Alaska facilities.
- State clearly that you are J‑1 and seeking a Conrad 30 or underserved area waiver position.
- Ask recruiters:
- “Have you sponsored J‑1 waiver physicians before?”
- “Do you anticipate having a family medicine opening that qualifies for Conrad 30 in my graduation year?”
- Compare:
- Practice scope (OB vs. no OB, ER coverage, inpatient responsibilities).
- Call schedules and compensation.
- Support structures (mid‑level providers, telehealth, specialty backup).
PGY‑3: Secure Contract & Start Conrad 30 Process
- Aim to sign an employment contract at least 6–12 months before graduation.
- Ensure the contract meets Alaska’s Conrad 30 requirements:
- Clearly states 3‑year term.
- Includes full‑time hours and site location(s).
- Doesn’t contain restrictive non‑compete clauses that conflict with state rules.
- Work with:
- Employer’s immigration counsel.
- Possibly your own immigration attorney.
- File the Conrad 30 application as early in the cycle as possible to:
- Avoid delays.
- Have time to pivot if something changes.
Practical Example: A Strategic Path Through Alaska
- Dr. A, an IMG in a mainland U.S. family medicine residency, does a rural Alaska elective in PGY‑2.
- They impress the local preceptors, who later connect them to a regional hospital in western Alaska.
- In early PGY‑3, Dr. A receives an offer: a broad‑scope FM job with inpatient and occasional ER work in a frontier HPSA community.
- The employer has J‑1 waiver experience and supports a Conrad 30 application.
- Dr. A starts work on time, completes the three‑year commitment, and later transitions to H‑1B or permanent residency.
Hawaii: Island Family Medicine Training & Waiver Options
Hawaii residency programs in family medicine offer robust training in urban, suburban, and rural island contexts, serving a multiethnic, multilingual population. For IMGs, Hawaii can be attractive for both residency and long‑term practice—but competition can be tight due to the state’s appeal and relatively small system.
Family Medicine Residency Context in Hawaii
Hawaii has a core family medicine residency program in Honolulu (with ties to the University of Hawaii system) and, in some years, satellite training or rural rotations on neighbor islands.
Typical features of Hawaii’s FM training environment:
- Emphasis on:
- Chronic disease management.
- Culturally competent care for Native Hawaiian, Pacific Islander, and Asian communities.
- Rural/neighbor island rotations with small hospitals and clinics.
- Strong demand for primary care across:
- Neighbor islands (e.g., Hawai‘i Island, Maui, Kaua‘i, Moloka‘i, Lana‘i).
- Underserved urban pockets in Honolulu.
Many communities in Hawaii are designated as HPSAs or MUAs, which aligns well with underserved area waiver strategies.
Hawaii Conrad 30 Overview
Hawaii also participates in the Conrad 30 program, but details can shift over time; always refer to the Hawaii State Department of Health for current rules. Common themes include:
Eligibility & Priorities:
- Must be a J‑1 physician with completed or near‑completed GME training.
- Must hold or be eligible for a Hawaii medical license.
- Preference often given to:
- Primary care specialties like family medicine.
- Placements on neighbor islands or in heavily underserved urban neighborhoods.
Practice and Site Requirements:
- 3 years of full‑time practice (40 hours/week).
- Service in HPSAs/MUAs/MUPs or other defined shortage areas.
- Employers must demonstrate:
- Prior unsuccessful recruitment of U.S. candidates.
- Sliding fee scale and acceptance of public insurance.
- Commitment to care for uninsured and underinsured patients.
Application Process:
- Typically limited slots (max 30/year) and sometimes substantial competition.
- Early submission and a strong statement of need/support from the employer can be important.
J‑1 Waiver Strategy for Hawaii: Step‑by‑Step
PGY‑1: Clarify Your Long‑Term Goals
- If your dream is to work in Hawaii long‑term, recognize:
- The market is smaller and more competitive than many mainland rural areas.
- Family medicine is still in demand, especially outside O‘ahu.
- Start networking early with:
- Faculty who have Hawaii connections.
- Alumni from your program now practicing in Hawaii.
- If your dream is to work in Hawaii long‑term, recognize:
PGY‑2: Targeted Exposure and Relationship‑Building
- Seek electives in Hawaii, preferably on neighbor islands if available.
- Learn about the specific healthcare challenges:
- Travel barriers for patients.
- Limited specialty access.
- High cost of living and its impact on healthcare utilization.
- Meet clinic directors and potential future employers; express your interest in Conrad 30 or underserved area waiver work and ask:
- “Have you sponsored J‑1 physicians before?”
- “Are you located in a HPSA/MUA, and do you expect to have a FM opening in the year I graduate?”
Late PGY‑2 to Early PGY‑3: Formal Job Search
- Focus on:
- Federally Qualified Health Centers (FQHCs).
- Rural hospitals on neighbor islands.
- Community health clinics serving low‑income or Native Hawaiian populations.
- Clarify with each employer:
- Their history with Conrad 30.
- Whether they have in‑house immigration support.
- Their timeline for hiring relative to the state’s Conrad 30 application cycle.
- Focus on:
PGY‑3: Contract & Waiver Application
- Negotiate a contract that:
- Specifies 3 years of full‑time practice.
- Lists all work locations (especially if you’ll rotate across islands or clinics).
- Coordinate with:
- Employer’s legal/immigration team.
- State office handling Conrad 30 submissions (to confirm any new requirements).
- Submit the application as early as your employer and the state allow.
- Negotiate a contract that:
Practical Example: Neighbor Island Strategy
- Dr. B, an IMG in family medicine residency, does a PGY‑2 elective on the Big Island of Hawaii, working with a rural FQHC and small hospital.
- They learn the clinic previously used Conrad 30 for internal medicine and psychiatry, but is now recruiting family physicians.
- Dr. B stays in touch with the medical director, and in early PGY‑3 is offered a position on the island, providing outpatient FM with some inpatient call.
- The clinic and hospital collaborate on a Conrad 30 application. Dr. B’s prior rotation and cultural familiarity strengthen the case that they are prepared for long‑term service in this underserved area.
- After three years dedicated service, Dr. B transitions to another visa or permanent residency while continuing to practice in Hawaii.

Comparing Alaska & Hawaii: Strategic Considerations for FM IMGs
Both Alaska and Hawaii can be excellent regions for family medicine physicians seeking J‑1 waivers. However, the best choice for you will depend on your personal preferences, training goals, and risk tolerance regarding waiver availability.
Demand and Competition
Alaska:
- High need for primary care in remote and frontier areas.
- Some years, Conrad 30 slots remain unfilled, especially for primary care.
- Broader scope of practice (including ER and OB in many sites) can be appealing for those who enjoy a wide skill set.
Hawaii:
- Strong need in rural and neighbor island communities, but the state’s overall allure makes it more competitive.
- Conrad 30 slots may fill faster, depending on the year.
- Scope of practice often more outpatient‑focused in some settings, though rural sites can still offer broad responsibilities.
Lifestyle and Personal Fit
Alaska:
- Long, dark winters in many regions; limited daylight in winter months.
- Outdoor lifestyle for those who enjoy mountains, snow sports, fishing, and wilderness.
- Remote postings may mean:
- Small communities.
- Limited social/cultural amenities.
- Weather‑dependent transportation.
Hawaii:
- Tropical climate, year‑round outdoor activities, beaches, hiking.
- Higher cost of living, especially housing and groceries.
- Island living can feel isolating for some; travel to mainland can be costly and time‑consuming.
Professional Development and Career Trajectory
Alaska:
- Ideal if you want to stay in rural or frontier family medicine long‑term.
- Experience in remote Alaska carries strong credibility for future roles in rural health leadership, global health, and academic rural medicine.
Hawaii:
- Valuable if you’re interested in:
- Pacific Islander and Native Hawaiian health.
- Community‑based and culturally responsive primary care.
- After the three‑year service, you’ll have strong credentials in underserved, multicultural primary care.
- Valuable if you’re interested in:
Risk Management: Backup Plans
- Apply to multiple regions, not just Alaska or Hawaii. Maintain:
- A primary target (e.g., Hawaii neighbor island).
- One or two secondary regions (e.g., mainland rural Midwest or Southwest).
- Evaluate each potential employer based on:
- Proven track record with J‑1 waivers.
- Clarity and transparency around the waiver process.
- Their willingness to start paperwork early.
- Keep a spreadsheet comparing practice sites, waiver experience, compensation, call schedules, and community factors.
Actionable Tips for Maximizing J‑1 Waiver Success in FM
1. Start Thinking About Waivers in PGY‑1
Even if the J‑1 waiver seems far away, the steps you take early matter:
- Request rural, frontier, or underserved rotations.
- Seek mentors who:
- Have worked in Alaska or Hawaii.
- Are familiar with J‑1 waiver paths (Conrad 30, underserved area waivers).
- Attend webinars or workshops at your program or specialty conferences about visa options for IMGs.
2. Be Upfront with Prospective Employers
When contacting Alaska or Hawaii employers:
- Introduce yourself as:
- “I am a J‑1 IMG in family medicine residency, graduating in [Year]. I am seeking a J‑1 waiver (Conrad 30 or other underserved area waiver) opportunity.”
- Ask early:
- Whether they have sponsored waivers previously.
- What their typical timeline is.
- If they are in a HPSA/MUA/MUP, and if they know their scores/designations.
This transparency helps avoid wasted time on employers who are unfamiliar with or unwilling to sponsor waivers.
3. Understand the Paper Trail
Typical documents and steps for Conrad 30/underserved area waivers in Alaska/Hawaii include:
- Signed employment contract for 3 years.
- Evidence of:
- J‑1 status and training completion.
- Medical license or eligibility.
- Employer’s shortage designation (HPSA/MUA).
- Employer’s recruitment efforts for U.S. physicians.
- Personal statements or CVs showing your commitment to underserved practice.
Knowing what will be needed helps you prepare in advance and avoid last‑minute delays.
4. Work with Immigration Professionals
- Encourage your employer to engage an experienced immigration attorney if they do not have one.
- Consider consulting your own attorney, especially if:
- You are pursuing complex visa transitions.
- You have any past status issues or multiple J‑1 segments.
5. Keep an Eye on Policy Changes
Visa and waiver policies can shift:
- Monitor:
- ECFMG announcements.
- State health department websites (Alaska and Hawaii).
- Professional organizations like the AAFP, AMA, and state medical societies.
- Policy changes might affect:
- Priority specialties.
- Definitions of shortage areas.
- Application cycles or documentation.
Staying informed allows you to adjust your strategy early rather than react at the last minute.
FAQs: Family Medicine J‑1 Waiver Strategies in Alaska & Hawaii
1. Do I have to complete my family medicine residency in Alaska or Hawaii to get a J‑1 waiver job there?
No. You can complete residency anywhere in the U.S. and still take a J‑1 waiver job in Alaska or Hawaii. What matters is:
- Your J‑1 status and completion of training.
- A qualifying job offer in a shortage area.
- Meeting the state’s Conrad 30 or other waiver criteria.
However, rotations or electives in Alaska/Hawaii can make you a stronger candidate and help with networking.
2. Are family medicine physicians prioritized for Conrad 30 waivers in Alaska and Hawaii?
Both Alaska and Hawaii clearly recognize primary care shortages, and family medicine is generally viewed favorably. Many states explicitly prioritize:
- Family medicine
- Internal medicine
- Pediatrics
- Psychiatry
Priority does not guarantee selection, but as an FM physician you are usually in a strong position, especially in frontier or rural communities.
3. Can I switch employers during my 3‑year J‑1 waiver commitment in Alaska or Hawaii?
Possibly, but it is complicated and risky. Switching employers generally requires:
- A new qualifying position in a HPSA/MUA (or otherwise approved site).
- Updated approval from the same or new state office and from USCIS.
Any break in service or mis‑step can jeopardize your waiver and future immigration options. Always consult an immigration attorney before changing jobs.
4. How early should I secure a J‑1 waiver job offer in Alaska or Hawaii?
Aim for at least 6–12 months before residency completion. This allows time for:
- Contract negotiation.
- State Conrad 30 processing.
- USCIS petition filings and processing times.
In more competitive states (and in years when demand is high), earlier is better. In smaller states like Alaska where slots sometimes remain open, you may have a little more flexibility, but it’s still wise to plan early.
By understanding how family medicine residency, FM match, Alaska residency and Hawaii residency programs, and J‑1 waiver pathways intersect, you can design a deliberate, realistic strategy. Whether your path leads to a snowy village clinic in Alaska or a neighbor island community health center in Hawaii, careful planning around Conrad 30 and underserved area waivers can turn your long‑term U.S. practice goals into a secure and rewarding reality.





















