
Understanding the Landscape: Family Medicine, Appalachia, and J-1 Waivers
Family medicine residency in Appalachia sits at the intersection of three powerful forces: a high-need region, a primary care–oriented specialty, and immigration rules that shape how international medical graduates (IMGs) can remain in the United States after training.
For IMGs on a J-1 visa, the J-1 waiver is often the most realistic pathway to remain in the U.S. and practice clinically after residency. Because Appalachian communities are heavily designated as underserved, the region offers particularly rich opportunities for family medicine residency graduates seeking positions that qualify for Conrad 30 and other underserved area waiver options.
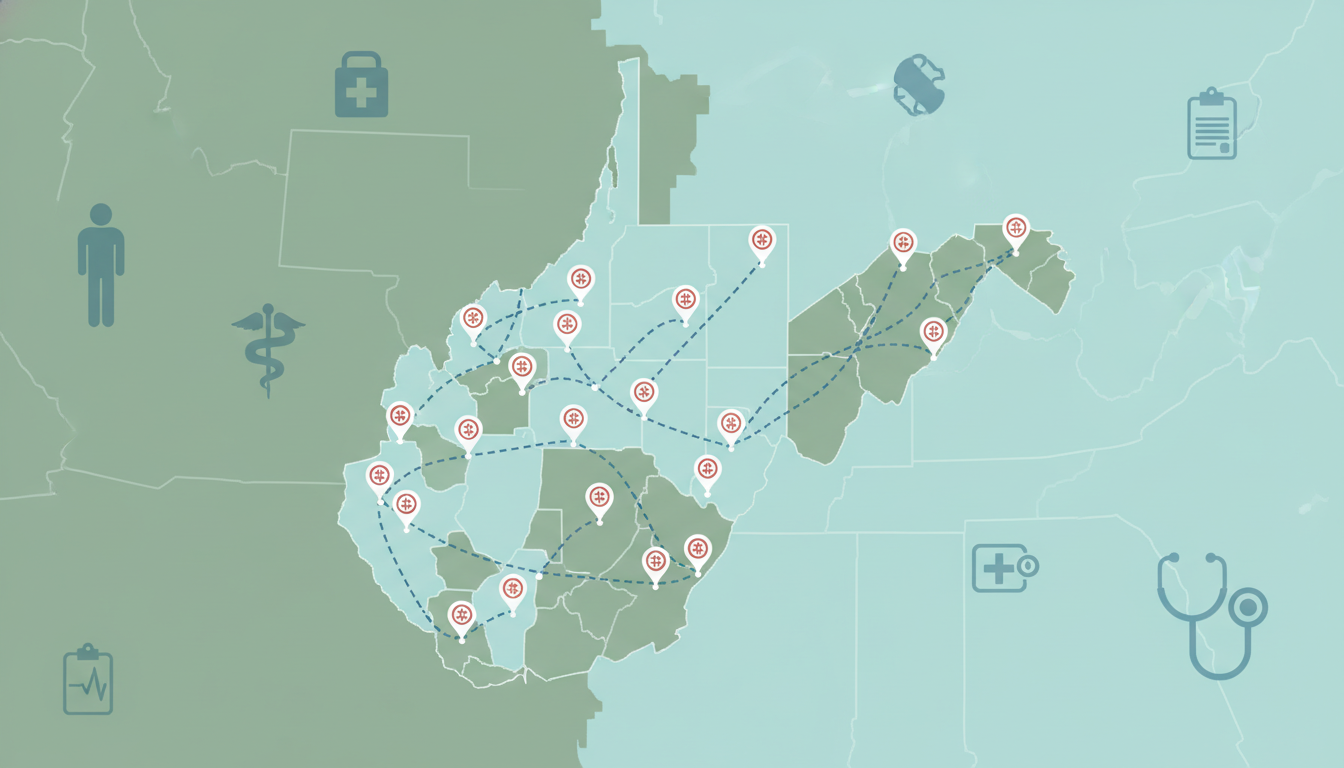
This guide focuses on J-1 waiver strategies for family medicine programs in Appalachia, with emphasis on West Virginia and Kentucky (but concepts apply broadly to the Appalachian region, including parts of Ohio, Virginia, Tennessee, North Carolina, and Pennsylvania).
You’ll learn:
- How the J-1 visa and waiver system works for family medicine residents
- Why Appalachian programs (including West Virginia and Kentucky residencies) are strategically attractive for FM IMGs
- How to plan your J-1 waiver strategy before, during, and after residency
- Specific steps to secure Appalachian waiver positions, including Conrad 30 and alternatives
- Common pitfalls and practical, time-sensitive tips
Throughout, the focus stays on family medicine residency, the FM match, and the unique opportunities associated with rural and community-based training in Appalachia.
J-1 Basics for Family Medicine Residents in Appalachia
Before designing a strategy, it’s essential to understand the framework you’re working within.
What is a J-1 Visa for IMGs?
Most IMGs who enter U.S. residency programs are sponsored on a J-1 exchange visitor visa through the Educational Commission for Foreign Medical Graduates (ECFMG, now part of Intealth). Key points:
- You are allowed to train in an ACGME-accredited residency and perhaps fellowship.
- After finishing training, you are subject to a two-year home-country physical presence requirement unless you obtain a J-1 waiver.
- Without a waiver, you must typically return to your home country for an aggregate of two years before being eligible for certain U.S. visas (e.g., H-1B, L-1, immigrant visas).
For family medicine residents, this usually means:
- 3 years of residency on J-1
- Then a choice: return home for two years, or secure a waiver job that lets you stay and work in the U.S.
What is a J-1 Waiver?
A J-1 waiver removes the two-year home residency requirement, allowing you to:
- Move to a different nonimmigrant status (commonly H-1B)
- Eventually pursue U.S. permanent residence (green card), if desired
For physicians, most waivers are tied to service in an underserved area. This is where Appalachia—and family medicine—become especially important.
Why Family Medicine + Appalachia Is a Strong Combination
Family medicine is uniquely suited to J-1 waiver pathways because:
- Most waiver programs require work in a Health Professional Shortage Area (HPSA) or Medically Underserved Area/Population (MUA/P).
- Appalachian regions are heavily designated as underserved, especially for primary care.
- Family medicine training prepares you to take comprehensive roles in these communities—outpatient primary care, hospitalist work in some smaller systems, obstetrics in select rural settings, and urgent care.
This makes graduates of Appalachian family medicine residencies (especially in West Virginia and Kentucky) particularly attractive to rural and underserved employers using Conrad 30 and related waiver programs.
Core J-1 Waiver Pathways Relevant to Appalachia
There are several J-1 waiver mechanisms; for family medicine residency graduates headed to Appalachia, four stand out.
1. Conrad 30 State Program
The Conrad 30 program is the primary path many IMGs use. Each U.S. state can sponsor up to 30 J-1 waiver physicians per fiscal year, typically prioritizing primary care in underserved areas.
For West Virginia and Kentucky residency graduates, this is often the most realistic and strategically important route.
Key Features:
- Up to 30 waiver slots per state per year
- Most states reserve a portion for primary care (family medicine, internal medicine, pediatrics, OB/GYN, psychiatry)
- Mandatory 3-year full-time service commitment, usually in HPSA/MUA/P sites
- Employer must show recruitment efforts and underserved need
- Requires support from the state health department (or equivalent)
- After approval, you change from J-1 to H-1B status and begin employment
Why it fits Appalachia:
- West Virginia and Kentucky both have chronic primary care shortages, especially outside metro centers.
- Many rural systems, FQHCs, and community health centers have experience sponsoring Conrad 30 waivers.
- Family medicine is often one of the state’s highest priorities due to broad scope and continuity of care.
State-specific rules differ. For example:
- Some states cap how many slots can go to specialists vs primary care.
- Some require the job site to be in a HPSA of a minimum score.
- Some allow “flex” slots—jobs not physically in an underserved area but serving underserved patients.
Action Step:
Before you even start your FM match cycle, download and read the Conrad 30 guidelines for the states you’re most interested in (e.g., West Virginia and Kentucky, plus any neighboring Appalachian states). Note:
- Application windows
- Priority specialties
- Employer requirements
- Any special preferences (e.g., rural vs urban underserved)
2. Federal Agency Waivers (e.g., VA, HHS Programs)
Several federal agencies can sponsor J-1 waivers to address physician shortages:
- U.S. Department of Health and Human Services (HHS) – historically more focused on research, but increasingly involved in clinical shortage waivers in certain programs
- Department of Veterans Affairs (VA) – sometimes considered in the waiver context
- Other federal agencies with clinical or public health responsibilities
In practice, for family medicine physicians targeting Appalachian communities, Conrad 30 and VA-connected roles are more common than HHS clinical waivers, but it’s important to be aware of these options, especially if:
- You are interested in a VA medical center in Appalachia
- You are engaged in significant public health, addiction medicine, or rural health research
3. Appalachian Regional Commission (ARC) Opportunities
The Appalachian Regional Commission does not directly grant J-1 waivers, but:
- It supports regional health initiatives, telehealth expansions, opioid response, and primary care access.
- Employers in ARC-sponsored projects may be particularly tuned into IMGs and waiver options.
For strategy purposes, it’s valuable to:
- Identify employers in ARC-funded or rural health network initiatives.
- Ask residency faculty if their major local systems have past experience with J-1 waivers in ARC-partnered projects.
4. Hardship and Persecution-Based Waivers
These are less common and more legally complex:
- Exceptional hardship waiver – Requires showing that your U.S. citizen or permanent resident spouse/child would suffer exceptional hardship if you must complete the two-year home residency.
- Persecution-based waiver – For significant risk of persecution if you return to your home country.
These routes are highly individualized and require competent immigration counsel. For most family medicine IMGs looking to stay in Appalachia, the Conrad 30 underserved area waiver route remains the primary focus.
Planning Your Strategy Before and During Family Medicine Residency
The best J-1 waiver outcomes start years before you finish residency. Your choice of family medicine residency program in Appalachia can either simplify or complicate your path.
1. Choosing the Right FM Programs in Appalachia
When you are preparing for the FM match, and especially if you are committed to staying in the U.S. after training, consider:
A. Program Location and Community Type
Programs in or near:
- Rural towns
- Smaller cities that act as hubs for the surrounding countryside
- Federally Qualified Health Centers (FQHCs) or rural health clinics
These frequently feed into waiver-eligible employers.
Examples (not exhaustive):
- Community-based programs in West Virginia’s smaller cities or rural counties
- University-affiliated programs in eastern Kentucky with strong rural track components
- Programs with continuity clinics in HPSA-designated areas
B. Program Track Record With IMGs and Waivers
Ask explicitly:
- Do you regularly match IMGs on J-1 visas?
- Where have recent graduates gone for J-1 waiver jobs?
- In the last 5 years, how many J-1 residents successfully obtained waivers, and in which states?
- Are there faculty who have gone through the J-1 waiver process themselves?
Programs with prior J-1 waiver success stories in Appalachian communities can provide:
- Networking connections to waiver employers
- Guidance on timing and paperwork
- Realistic expectations in terms of job search
C. Regional Employer Network
Some family medicine residencies in Appalachia are embedded in health systems that:
- Run multiple clinics across wide rural catchment areas
- Operate critical access hospitals or small community hospitals
- Partner actively with county health departments, FQHCs, and mental health centers
These systems often:
- Understand Conrad 30 and other waivers
- Have a strong interest in retaining residents as staff physicians, including IMGs
2. During Residency: Building a Waiver-Ready Profile
Once you are in a family medicine residency in Appalachia, you can strengthen your waiver prospects in several ways.
A. Lean into Rural and Underserved Rotations
Prioritize rotations and electives in:
- Rural clinics
- FQHCs and community health centers
- Substance use disorder treatment programs
- Community hospitals in underserved counties
This accomplishes:
- Direct experience in environments that seek waiver physicians
- Relationship-building with potential future employers
- A track record of commitment to underserved care, important to both states and employers
B. Develop a Broad Family Medicine Skill Set
Appalachian practice often demands breadth:
- Robust outpatient primary care (all ages)
- Chronic disease management (diabetes, COPD, heart failure)
- Mental health and substance use care (especially opioid and stimulant use disorders)
- Women’s health, including prenatal care and limited OB in some sites
- Minor procedures (joint injections, skin biopsies, IUD insertions, etc.)
Being versatile increases your value to rural employers who need “one-stop” family physicians.
C. Cultivate Faculty Mentors Who Understand J-1 Issues
Identify attendings or program leaders who:
- Have experience with IMGs or are IMGs themselves
- Have relationships with HR/administration at regional systems
- Know which local employers have historically used J-1 waiver recruits
Meet with them early (PGY-1 or early PGY-2) to discuss:
- Your goal to pursue a J-1 waiver job in Appalachia
- Their advice on which rotations and community sites to prioritize
- Potential employers you should get to know

Executing the Waiver Job Search: Timeline and Tactics
Timing is critical. Many J-1 residents underestimate how early they must start.
1. General Timeline for J-1 Waiver Jobs
Assume a standard 3-year family medicine residency with June 30 graduation:
- PGY-1 (early): Learn the basics of J-1 and waivers; identify likely states (e.g., West Virginia, Kentucky, neighboring Appalachian states).
- PGY-1 (late) to PGY-2 (early): Deepen ties with rural/underserved sites; get clear on your preferred practice setting (FQHC vs hospital-employed, etc.).
- PGY-2 (mid to late):
- Actively explore J-1 waiver jobs.
- Attend recruitment fairs (especially those focused on rural/Appalachian practice).
- Start direct outreach to potential employers.
- PGY-3 (early):
- Secure a signed employment contract for a waiver-eligible position.
- Employer prepares and submits Conrad 30 application to the appropriate state.
- PGY-3 (mid to late):
- After state recommends you, U.S. Department of State and USCIS process the waiver.
- Your employer files for your H-1B.
- You transition to H-1B around the time residency ends and waiver job begins.
Because Conrad 30 slots are limited and many states open application windows in the fall/winter before your graduation, being late can cost you a year.
2. Targeting Employers in Appalachia
Focus your search on:
- FQHCs and rural/community health centers in West Virginia, eastern Kentucky, and neighboring Appalachian areas
- System-owned primary care clinics in smaller towns
- Rural hospitals that staff outpatient clinics and hospitalist roles with family physicians
- VA clinics and hospitals in Appalachian catchment areas (if they sponsor waivers)
Practical steps:
- Use state and federal shortage-area tools:
- HRSA HPSA and MUA/P locator
- State health department primary care office websites
- Ask your residency program:
- “Which employers in the region routinely hire J-1 waiver family medicine physicians?”
- Engage recruiters carefully:
- Many health systems use in-house recruiters or contracted firms familiar with Conrad 30.
- Verify that the recruiter and employer truly understand J-1 requirements and have sponsored waivers before.
3. Evaluating Whether a Job is Truly Waiver-Eligible
Key questions to ask every potential employer:
- Are you willing and able to sponsor a J-1 waiver (e.g., Conrad 30) for family medicine?
- Have you successfully sponsored J-1 physicians before? In which state programs?
- Is the clinic/hospital located in a recognized HPSA or MUA/P?
- In which state will the application be filed (especially relevant near state borders in Appalachia)?
- Who will handle the waiver and H-1B paperwork—an in-house legal team or an external immigration attorney?
Ask to speak with:
- Current or former J-1 physicians on staff
- The HR representative or legal counsel who manages immigration matters
If an employer seems uncertain or inexperienced, you may be at higher risk of delays or errors. This doesn’t necessarily mean you should walk away, but you’ll need strong legal guidance and extra vigilance.
4. Negotiating the Employment Contract
In a waiver job, your contract must meet specific requirements:
- 3-year full-time service commitment
- Typically 40 hours/week of patient-care related activity (check state rules)
- Clinic site(s) clearly defined (especially if multiple sites or outreach clinics)
- No overly restrictive non-compete clauses that contradict state waiver rules
Discuss with both:
- An immigration attorney (for waiver and visa compliance)
- A healthcare employment attorney (for contract fairness, salary, benefits, malpractice, call, etc.)
Key practical points to negotiate or clarify:
- Salary and benefits relative to MGMA or other benchmarks (rural areas may offer loan repayment or signing bonuses).
- Expected patient panel size and visit volume.
- Call coverage (especially if the role involves inpatient rounds or OB).
- CME time and funding.
- Support for future permanent residency (green card) after waiver obligations.
State-Specific Considerations: West Virginia and Kentucky
While you must always verify current rules from official sources (and with counsel), some recurring themes apply to West Virginia and Kentucky as Appalachian states.
West Virginia
Key characteristics:
- Large portions of the state are designated as primary care HPSAs.
- Strong need for family medicine physicians in small towns and rural counties.
- Multiple family medicine residencies embedded in health systems that serve broad rural regions.
Strategic points:
- West Virginia’s Conrad 30 program has historically been open to primary care, with a particular emphasis on rural/underserved sites.
- Employers include:
- Hospital systems with network clinics
- FQHCs
- Rural health clinics
- Some positions may involve blended outpatient + limited inpatient responsibilities, which can be attractive to broad-scope FM physicians.
Actionable tip:
- During residency (especially if training in West Virginia), ask your program director:
“Which West Virginia employers have successfully used Conrad 30 to hire our graduates, especially family medicine?”
Kentucky (Especially Eastern Kentucky)
Eastern Kentucky is quintessential Appalachia, with significant rural poverty and health challenges.
Key features:
- High burden of chronic illness (e.g., diabetes, COPD, heart disease).
- Significant impact from the opioid crisis.
- Shortage of primary care clinicians, especially in mountain communities.
Strategic points:
- Kentucky’s Conrad 30 program often values family medicine physicians who can provide comprehensive, longitudinal care in rural clinics.
- There may be opportunities tied to:
- Critical access hospitals
- Outpatient family medicine clinics with telehealth integration
- Integrated behavioral health models (especially addiction treatment)
Actionable tip:
- If you train in or near Kentucky, consider doing electives at rural clinics in eastern counties; these often become entry points to waiver positions.
Beyond the Waiver: Long-Term Career and Immigration Planning
The J-1 waiver is just one stage of your career and immigration journey.
1. After the 3-Year Waiver Commitment
After completing your 3-year underserved area waiver (Conrad 30 or equivalent), options may include:
- Continuing with the same employer (often with expanded responsibilities or leadership roles).
- Moving to another employer, possibly in a more urban/suburban area, now that your J-1 requirement is satisfied.
- Transitioning from H-1B to permanent residence (if not already in process).
If your long-term goal is to stay in the U.S., discuss with your employer early on:
- Will you sponsor my green card?
- Under what category (e.g., EB-2 with PERM labor certification, or possible National Interest Waiver if applicable)?
- When will we start the process (many begin during the first 1–2 years of waiver service)?
2. Balancing Service and Career Development
A position in an Appalachian underserved community can be deeply rewarding:
- Strong continuity relationships with patients
- Meaningful impact on community health
- Opportunities to develop niche skills (addiction medicine, rural obstetrics, telemedicine, leadership in small systems)
To maintain professional growth:
- Attend regional and national FM conferences.
- Stay active in scholarly or quality improvement projects (many rural sites welcome QI initiatives on chronic disease or opioid stewardship).
- Consider leadership roles in clinic administration, medical directorships, or community outreach.
Your early-career years in an Appalachian underserved waiver job can lay the foundation for a long-term career that’s both mission-driven and professionally robust.
Frequently Asked Questions (FAQ)
1. Should I prioritize family medicine residency programs in Appalachia if I already know I want a J-1 waiver job there?
If your long-term plan is to practice in Appalachia, training there is often advantageous:
- You build local connections with employers who regularly sponsor Conrad 30 and other underserved area waivers.
- State health departments and local systems become familiar with you during residency.
- You gain a clear understanding of the region’s clinical realities, making you a more attractive candidate.
However, reputation, training quality, and your overall fit with the program are also critical. A strong FM residency elsewhere that actively supports J-1 IMGs and has connections to Appalachian employers can still work well.
2. Can I do a fellowship after family medicine residency if I’m on a J-1 visa, or must I go straight to a waiver job?
Yes, many J-1 family medicine graduates pursue fellowships (e.g., sports medicine, geriatrics, palliative care, addiction medicine) under continued J-1 sponsorship. But:
- Each additional year prolongs the period before you must address the two-year home requirement or a waiver.
- Some states and employers may prefer you to be newly graduated for Conrad 30 roles; others might value extra skills.
If your top priority is to remain in the U.S. and secure a waiver position in an underserved Appalachian area, weigh the benefits of fellowship against the risk of tighter waiver job markets or shifting state policies in future years. Discuss this in detail with both your program director and an immigration attorney.
3. Are J-1 waiver jobs in Appalachia only outpatient, or can they include inpatient and OB?
Many Appalachian family medicine waiver jobs are primarily outpatient, but there is variety:
- Some roles combine outpatient clinic with inpatient rounding at a small hospital.
- A subset include low- to moderate-volume OB (especially in rural hospitals that rely on family physicians for maternity care).
- Others may integrate urgent care or telehealth.
Your scope will depend on your skills, comfort, and the needs of the community. If you want OB or inpatient responsibilities, choose a residency with robust training in those areas and seek employers who value full-scope FM.
4. What happens if I cannot secure a J-1 waiver job before residency ends?
If you do not obtain a waiver:
- You remain subject to the two-year home-country physical presence requirement.
- Options may include returning to your home country for two years, pursuing a hardship/persecution-based waiver (if applicable), or exploring positions that can accommodate the two-year requirement in creative ways (rare and complex).
This scenario is high-stakes and time-sensitive. If you’re approaching mid-PGY-3 without a solid waiver plan:
- Immediately consult with an experienced immigration attorney.
- Intensify your search, possibly expanding to more states with strong demand for primary care IMGs.
- Engage your program leadership to tap into their wider employer network.
By starting early, choosing your family medicine residency intentionally, and building relationships across the Appalachian health care landscape—especially in West Virginia and Kentucky—you can position yourself for a successful transition from J-1 training to a Conrad 30 or underserved area waiver role. This not only satisfies immigration requirements but also allows you to deliver essential primary care in communities that need it most.





















