Understanding the J-1 Landscape for OB GYN Residents
For international medical graduates (IMGs) in Obstetrics & Gynecology, the J-1 visa is the most common pathway to train in a U.S. residency or fellowship. However, the J-1 comes with a major condition: the two-year home residence requirement under INA §212(e). After finishing your OB GYN residency (and fellowship, if applicable), you are generally required to return to your home country for a cumulative two years before you can:
- Change to H-1B status in the U.S.
- Obtain an immigrant visa (green card)
- Adjust status to permanent residence
- Receive many other nonimmigrant visas such as L-1 or K
To remain in the U.S. and move directly into practice, you will typically need a J-1 waiver. For most graduating OB GYN residents, this means securing a position in an underserved area waiver job, usually under the Conrad 30 program or a similar federal program.
This guide breaks down J-1 waiver strategies specifically for Obstetrics & Gynecology, with a focus on:
- How OB GYN as a specialty fits into the J-1 waiver world
- Detailed pathways: Conrad 30, HHS and other federal waivers, hardship and persecution options
- Practical job-search and timing strategies during the obstetrics match and beyond
- Contract and immigration considerations unique to OB GYN
While this article is informational and strategy-focused, it is not legal advice. Work closely with an experienced immigration attorney throughout the process.
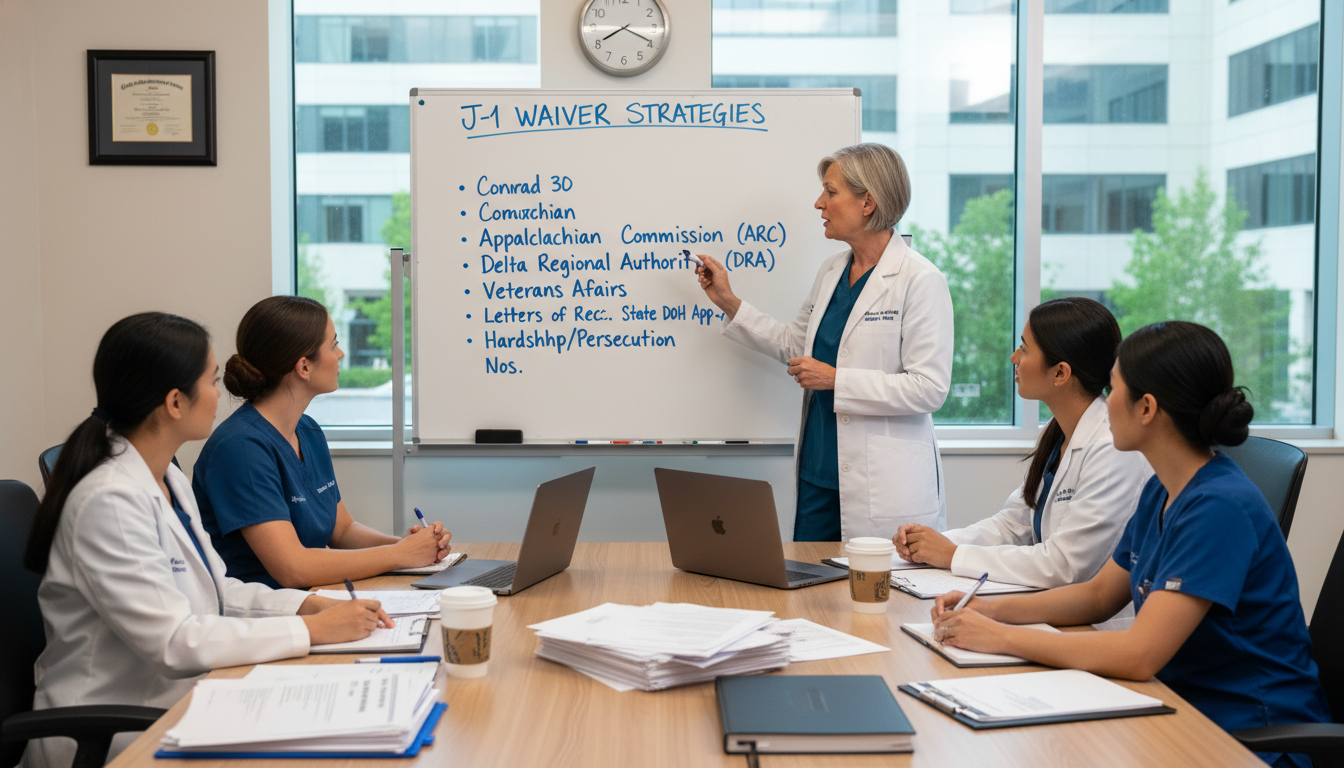
Core J-1 Waiver Options for OB GYN Graduates
Several waiver options are theoretically available, but only a subset are widely practical for someone completing an OB GYN residency in the U.S.
1. Conrad 30 State Program
The Conrad 30 program is the most common J-1 waiver pathway for OB GYN physicians. Each U.S. state (plus certain territories) can sponsor up to 30 J-1 physicians per fiscal year to work in underserved communities.
Key features:
- Employment type: Full-time clinical practice, typically 40 hours/week
- Duration: Minimum 3-year service commitment
- Visa status: H-1B (not cap-exempt in all cases, but most Conrad positions are cap-exempt through affiliated entities or non-profit hospitals)
- Practice setting: Must primarily serve patients in designated shortage areas or through “flex” slots
Why OB GYN fits well in Conrad 30:
- High demand: OB GYN specialists are consistently in shortage, especially in rural and inner-city areas
- Many states explicitly list OB GYN as a priority specialty
- Maternity care deserts and hospital L&D closures make OB GYN recruitment a political and public health priority
Typical eligible sites:
- Federally Qualified Health Centers (FQHCs)
- Rural hospitals with labor & delivery units
- Community health centers
- Safety-net hospitals in inner-city areas
- Private group practices with significant Medicaid/uninsured volume in shortage areas
Employment model:
- Employed directly by a hospital or health system
- Employed by a private group with a hospital affiliation
- Rarely, independent contractor arrangements—many states strongly prefer or require direct employment
Key takeaway: For most OB GYN J-1 physicians, Conrad 30 is the primary and most realistic strategy for remaining in the U.S. after residency.
2. Federal Agency Waivers (Beyond Conrad 30)
A few federal agencies can sponsor J-1 waivers directly, independent of state Conrad 30 caps. For OB GYN, these are less common but important to understand:
a. Department of Health and Human Services (HHS)
Historically, HHS had primary emphasis on primary care (FM, IM, pediatrics, psychiatry). For specialists like OB GYN, eligibility can be more limited and criteria may be adjusted over time.
HHS-contracted facilities must often:
- Be in areas of extreme shortage
- Participate in certain federal programs (e.g., National Health Service Corps-like models)
Some HHS waiver programs periodically open to specialists in maternal health priority areas. OB GYNs may qualify if:
- The facility serves a high volume of Medicaid/uninsured patients
- The position is in a maternity care desert or high maternal mortality region
- The position supports public health priorities (e.g., maternal mortality reduction, high-risk pregnancy care)
Because HHS rules are periodically updated, check current regulations and consult your attorney before assuming eligibility.
b. VA, ARC, and Other Agencies
- Veterans Affairs (VA): Rare for OB GYN, as VA hospitals have limited inpatient obstetrics volumes and generally do not employ large numbers of OB GYNs in L&D roles.
- Appalachian Regional Commission (ARC) and Delta Regional Authority (DRA): Cover certain geographic regions (Appalachia, Mississippi Delta). They may occasionally support specialist waivers, including OB GYN, if serving severely underserved communities.
In practice, for OB GYN, most federal agency waivers are niche. They may be valuable if your target state’s Conrad 30 slots are full or not favorable to specialists.
3. Hardship and Persecution Waivers
These are not tied to specific jobs but are case-based waivers:
a. Exceptional Hardship Waiver
Based on the claim that your 2-year home return would cause exceptional hardship to a U.S. citizen or permanent resident spouse or child.
Common OB GYN–related scenarios:
- Spouse has a medical condition requiring specialized care not readily available in your home country
- Child receives critical therapy or special education services unavailable or unreliable abroad
- Documented risk related to pregnancy or reproductive health if spouse must relocate overseas
Requirements:
- Strong documentary evidence of hardship beyond normal family separation
- Legal argumentation by an immigration attorney
- No need to work in a shortage area, but waiver is discretionary
b. Persecution Waiver
Granted if you can demonstrate a well-founded fear of persecution in your home country based on:
- Race, religion, nationality, membership in a particular social group, or political opinion
For an OB GYN doctor, this might intersect with:
- Practicing obstetrics and gynecology in settings where gender-based persecution or professional persecution is a credible threat
- Advocacy for women’s reproductive rights in countries where that is politically dangerous
Both hardship and persecution waivers are legally complex, take longer, and outcomes can be unpredictable. They are realistic for some physicians but are not the default route for most OB GYN graduates.
4. Alternative Non-Waiver Pathways (Limited Use)
In rare cases, an OB GYN may:
- Complete the 2-year home residence requirement, then return to the U.S. in H-1B or immigrant status, or
- Work partially abroad while engaging in long-distance steps toward U.S. re-entry
However, for most IMG OB GYN residents deeply invested in U.S. practice, direct J-1 waiver strategies (especially Conrad 30) remain the centerpiece.

Timing Your Strategy: From Obstetrics Match to PGY-4 and Beyond
Effective use of J-1 waiver options in OB GYN hinges on early planning and precise timing.
PGY-1 to PGY-2: Laying the Groundwork
In your first two years of OB GYN residency:
- Understand your J-1 obligations: Read your DS-2019 and know your program end date.
- Clarify your long-term goals:
- Do you want to stay in the U.S. long-term?
- Are you considering fellowship (MFM, REI, Gyn Onc, FPMRS, MIGS)?
- Talk to your GME office and program leadership:
- Confirm that your residency is on a J-1 (not H-1B)
- Ask what prior graduates have done for waivers
- Attend immigration info sessions offered by your institution or ECFMG/EVSP.
No formal waiver steps are taken yet, but this is when to educate yourself and track your timeline.
PGY-3: Strategic Decisions and Early Job Exploration
During PGY-3:
Decide on fellowship vs. job directly after residency
- If pursuing fellowship on J-1, you will add extra years before needing a waiver but will still face the same 2-year rule.
- Some states and employers are more enthusiastic to sponsor subspecialists (e.g., MFM in rural areas), while others prioritize general OB GYN.
Start researching Conrad 30 rules by state
- Look up each state’s Conrad 30 program:
- Application timelines (some open October 1, others later; some are rolling)
- Priority specialties (many specifically favor OB GYN due to maternal care shortages)
- Required documents (contracts, recruitment evidence, site designation)
- Identify 3–8 target states where:
- You would realistically be willing to live for at least 3 years
- OB GYN is explicitly welcomed or prioritized
- Historical use of slots is not 100% for internal medicine/primary care
- Look up each state’s Conrad 30 program:
Attend career fairs and speak with recruiters
- Ask pointed questions:
- “Do you sponsor J-1 waivers?”
- “Have you sponsored Conrad 30 waivers for OB GYNs before?”
- “Is this practice located in a HPSA/MUA or using flex slots?”
- Keep a log of interested employers and their locations.
- Ask pointed questions:
PGY-4: The Crucial J-1 Waiver Job Search Year
Your final year is when everything must come together.
Ideal timeline (for residency completing June 30):
- Jan–June of PGY-3 to early PGY-4:
Begin targeted job search for J-1–friendly OB GYN positions. - July–October PGY-4:
- Interview and sign contract for a job that meets waiver criteria.
- Ensure contract aligns with specific state Conrad 30 requirements.
- Fall/Winter PGY-4:
- Employer’s attorney prepares and submits the state Conrad 30 application.
- Winter/Spring PGY-4:
- If state approves, application goes to the U.S. Department of State (DOS), then USCIS for H-1B processing.
- Before residency completion (ideally by May/June):
- Aim to obtain your H-1B approval notice to start the waiver job promptly on or after July 1.
Risk management:
- Some states fill OB GYN-friendly slots quickly. Applying late (e.g., after January) can be risky.
- Consider backup states and maintain contact with multiple employers until you have a secure approved slot.
- If a state has historically not filled all 30 slots, late applications may still be feasible, but don’t rely on it.
Choosing the Right Underserved Area Waiver Job as an OB GYN
The quality and fit of your waiver job can shape your life and career trajectory.
1. Understanding “Underserved Area” for OB GYN
Most Conrad 30 positions are tied to:
- Health Professional Shortage Area (HPSA)
- Medically Underserved Area (MUA)
- Medically Underserved Population (MUP)
- Or use flex slots, where the site is not in a shortage area but serves patients from shortage areas
For OB GYN, this often translates into:
- Rural counties with a single small hospital and no recent OB coverage
- Suburban fringe communities adjacent to big cities with a high Medicaid/uninsured population
- Urban core safety-net hospitals and FQHCs providing women’s health services
Assess:
- Distance to the nearest tertiary care center for high-risk obstetrics
- Availability of anesthesia, NICU, and emergency surgical support
- Call schedule and backup arrangements
2. Practice Model Considerations Specific to OB GYN
Key factors to evaluate:
- Obstetrical volume:
- Too low: Skills may atrophy; OB service may be at risk of closure.
- Too high: Unsafe workload, burnout risk, inadequate support.
- Gynecologic surgery resources:
- Access to OR time, laparoscopy, hysteroscopy equipment
- Availability of support services: anesthesia, blood bank, post-op ICU if needed
- Call structure:
- 1:3 or better is generally desirable; avoid being the only OB GYN on call for large catchment areas without backup.
- Support staff:
- Midwives, family medicine with OB, women’s health NPs/PAs
- Access to MFM consultation (in-person or telemedicine)
3. Contract and Legal Terms to Watch
Your employment contract must satisfy immigration requirements and still be sustainable for you.
Key elements:
- Term: Minimum 3 years, usually full-time 40 hrs/week
- Location: Clearly defined practice sites; beware of vague language allowing relocation far away from the designated underserved area
- Scope of practice: Confirm mix of obstetrics, gynecology, surgery, and clinic.
- Non-compete clauses:
- In many waiver jobs, non-competes can severely limit your options after the 3-year obligation.
- Some states restrict or ban physician non-competes; know your state’s law.
- Compensation structure:
- Base salary vs. RVU or productivity bonuses.
- Ensure salary is aligned with regional OB GYN benchmarks and not exploitatively low due to waiver dependency.
- Call pay:
- Clarify if call is included in base salary or compensated separately.
- Tail coverage:
- Who pays for malpractice tail if you leave after 3 years? This can be a significant cost.
Always have an independent attorney review the contract—not just the employer’s immigration counsel.

J-1 Waiver Strategies Tailored to OB GYN Subspecialties
Many OB GYN trainees pursue fellowships. Each subspecialty intersects with J-1 waiver options slightly differently.
1. Maternal-Fetal Medicine (MFM)
Pros for J-1 waiver:
- Acute national shortage of MFMs
- Rural and community hospitals often need tele-MFM or part-time coverage
- Some states highly value MFM services in maternal mortality reduction strategies
Challenges:
- Many rural hospitals cannot support a full-time MFM service
- You may need a hybrid model: part-time local plus telehealth across a system
Strategy:
- Target regional health systems that have multiple hospitals and a commitment to perinatal quality improvement.
- Be open to flexible arrangements, such as strong telemedicine MFM plus periodic on-site clinics.
2. Gynecologic Oncology
Pros:
- Highly specialized, high-need field; few gynecologic oncologists relative to demand
- Cancer centers and tertiary hospitals in non-major metros may qualify for Conrad or federal waivers.
Challenges:
- Many gynecologic oncology positions are in academic medical centers in metropolitan areas that may not qualify as shortage areas.
Strategy:
- Look for cancer centers and tertiary hospitals in secondary cities or multi-state systems with documented patient catchment from underserved regions.
- Explore flex-slot Conrad positions or regional waiver programs (ARC, DRA) if geographically relevant.
3. Reproductive Endocrinology & Infertility (REI)
Reality check:
- Many REI practices are private, high-resource, and located in affluent urban/suburban areas.
- Few are in HPSAs/MUAs or structured as safety-net providers.
Consequence:
- J-1 waiver options for REI are limited. Many REI-bound physicians either:
- Return home for 2 years post-fellowship, then re-enter the U.S., or
- Pursue hardship/persecution waivers if applicable.
Strategy:
- If staying in the U.S. is a priority, consider:
- Completing a general OB GYN or another subspecialty waiver first, then later transitioning to or adding REI practice once your immigration status is more secure.
4. Female Pelvic Medicine & Reconstructive Surgery (FPMRS) and MIGS
- Both are often hospital-based specialties, needed in community hospitals across wide regions.
- They can qualify for Conrad 30 if your employer can document service to underserved populations.
Strategy:
- Target health systems with:
- Regional referral patterns from rural or underserved counties
- Documented shortages in urogynecology or complex benign gynecology
Long-Term Planning After the Waiver: From Conrad 30 to Permanent Residence
J-1 waiver strategies should be integrated into your long-term immigration and career planning.
1. Moving From H-1B Waiver Job to Green Card
During or after your 3-year Conrad or other underserved area waiver service, most OB GYNs:
- Pursue employment-based permanent residency, usually under:
- EB-2 (often with PERM labor certification)
- Occasionally EB-1 for those with strong academic or research profiles
Key steps:
- Employer sponsorship:
- Many hospitals and health systems are willing to file PERM and I-140 petitions.
- National Interest Waiver (NIW) options:
- As an OB GYN serving severely underserved areas or working in maternal mortality reduction, you may have arguments for a physician NIW or standard NIW.
- These require demonstrating that your work is of substantial intrinsic merit and in the national interest (especially plausible in maternal health deserts).
2. Flexibility After the 3-Year Obligation
After completing your 3-year waiver:
- Your H-1B is no longer tied to underserved-area work.
- You may:
- Move to a practice in a non-shortage area
- Join an academic department in a larger city
- Shift to a subspecialty or lifestyle-focused practice
However:
- Watch non-compete clauses and geographic restrictions in your waiver job contract.
- Time career moves to align with your green card process stage and H-1B status validity.
Frequently Asked Questions (FAQ)
1. Can I pursue an OB GYN residency on J-1 and then get an H-1B directly for my first job without a waiver?
No. If you are subject to the J-1 two-year home residence requirement, you cannot change to H-1B status in the U.S. or obtain an H-1B visa abroad until you either:
- Complete the 2-year home residence requirement, or
- Obtain a J-1 waiver (e.g., Conrad 30, hardship, persecution, or federal agency waiver)
For almost all IMG OB GYN residents who wish to stay in the U.S. after training, a J-1 waiver is essential.
2. Are all OB GYN positions in rural areas automatically eligible for Conrad 30?
No. While many rural positions qualify, eligibility depends on:
- Whether the practice site is in a designated HPSA/MUA/MUP, or
- The state’s flex slot rules and whether the employer can use flex slots
- Compliance with each state’s specific Conrad 30 criteria (recruitment requirements, service hours, etc.)
Always verify:
- The exact designation status of the clinic/hospital address
- The state program’s current rules and slot availability
3. What happens if I leave my J-1 waiver job before completing the 3 years?
Leaving early can be serious:
- You may lose the benefits of the J-1 waiver, and the two-year home requirement can be considered reinstated.
- Limited exceptions exist (e.g., severe breach by employer, facility closure), but you would need immediate alternative arrangements and legal guidance.
Before changing or leaving a waiver job:
- Speak with an immigration attorney
- Review your contract and state waiver program rules
- Explore whether a transfer to another qualifying underserved employer is possible
4. Does doing a fellowship on J-1 before seeking a waiver make it harder or easier?
It depends on your subspecialty and goals:
- Easier if:
- Your subspecialty (e.g., MFM, Gyn Onc) is also in shortage in underserved areas
- You target systems that value highly specialized OB GYN services in rural or safety-net contexts
- Harder if:
- Your subspecialty (e.g., REI) is concentrated in affluent, non-shortage areas
- There are fewer Conrad 30-eligible employers hiring subspecialty-only positions
Many OB GYNs choose:
- To complete general OB GYN waiver service first, then pursue subspecialty work once immigration status is more secure; or
- To apply strategically for fellowships with strong ties to underserved maternal health programs that may support waiver pathways later.
Planning your J-1 waiver strategy as an OB GYN requires early awareness, informed decision-making, and proactive job search efforts. By understanding Conrad 30, underserved area waiver options, and the nuances of OB GYN practice needs across the U.S., you can align your training, specialty interests, and immigration pathway toward a sustainable, rewarding career in women’s health.





















