The idea that “SOAP is only for desperate applicants” is not just wrong. It is dangerous, lazy thinking that costs people training spots and derails careers.
Let me be blunt: using the Supplemental Offer and Acceptance Program (SOAP) strategically is what savvy applicants do. The “I’m too good for SOAP” mindset is how people go from “temporarily unmatched” to “no residency, no license, no plan.”
You can dislike SOAP all you want. You cannot ignore what the data shows.
What SOAP Actually Is (And What It Is Not)
SOAP isn’t a sympathy program. It’s a structured, time-compressed match.
During Match Week, if you find out on Monday that you’re unmatched (or partially matched for advanced/prelim combos), SOAP is the mechanism that:
- Tells you which programs have unfilled spots
- Lets you apply via ERAS to a limited number of those programs
- Enables programs to interview and rank you
- Sends out multiple rounds of binding offers
That’s not “begging for a job.” That’s participating in another algorithmically organized, regulated matching process with real programs that simply did not fill.
And those unfilled programs? Many are perfectly solid:
- Solid community IM and FM programs
- New or expanding programs still building reputation
- Programs in less popular locations
- Spots in prelim surgery, transitional year, internal medicine, etc.
Are there some weak or malignant programs in the SOAP list? Of course. There are weak and malignant programs in the main Match too. Pretending SOAP is uniquely toxic is just a way for insecure people to feel better about their own outcome.
The Data: Who Actually Ends Up in SOAP?
Not the caricature you’ve heard.
The stereotype: SOAP is full of “desperate” applicants who failed exams, had red-flag professionalism issues, or “shouldn’t be doctors anyway.”
Reality: SOAP is full of:
- Applicants who aimed too high and under-applied to safety programs
- Strong applicants in overly competitive specialties (derm, ortho, plastics, ENT)
- Dual-apply folks whose backup didn’t pan out because they treated it like an afterthought
- International medical graduates (IMGs) and DOs who were competitive but faced numbers games and biases
- People who had one bad exam, one weird MSPE comment, or simply bad luck in a given year
Is SOAP over-represented with higher-risk profiles (low Step, attempts, gaps)? Yes. But it’s also full of “borderline misses” and even obviously solid candidates who miscalculated.

| Category | Value |
|---|---|
| Over-competitive specialty | 25 |
| Under-applied to safety | 20 |
| Low scores/attempts | 25 |
| IMG/DO with bias issues | 20 |
| Other (personal, timing) | 10 |
Those percentages are illustrative, but they match what I’ve seen looking at cohorts across multiple cycles: SOAP is a mixed bag, not a trash bin.
Myth: “If I SOAP, I’ll Be Labeled Forever”
This is the emotional core of the “SOAP is desperate” myth: that using SOAP brands you as defective, and every future colleague will know you “failed the Match.”
Here’s the truth:
Your NRMP result is not public.
Programs you SOAP into know you SOAPed. Most others do not. Your co-residents only know if you tell them or if they were there that year and paying attention.Board certification and state licensing do not care how you got your residency.
They care that you completed an ACGME-accredited program and passed your boards. No application asks “Did you enter residency through SOAP? Y/N”.Fellowship programs care about performance, not entry mechanism.
I’ve seen SOAPed prelims go on to match into anesthesiology, radiology, even cardiology fellowships. Once you’re in training, your evaluations, letters, research, and board scores carry far more weight than how you got your PGY-1.Most attendings barely remember who SOAPed.
Ask any PD: by October of intern year, the focus is “Who’s actually good?” Not “Who got an offer on Thursday of Match Week instead of Monday of Match Week?”
The “labeled forever” argument is almost always fear talking, not reality. It’s ego masquerading as strategy.
Myth: “SOAP Spots Are Garbage Programs”
Another lazy take: that if a program didn’t fill in the main Match, it must be trash. That’s just not how the numbers work.
Reasons decent programs end up with open spots:
- They’re in less desirable locations (mid-sized towns, rural states, certain regions)
- They just expanded positions and underestimated how many ranks they’d need
- They’re new programs still building a reputation and pipeline
- They’re in specialties where applicants overshoot to “top” programs and abandon mid-tier ones
- Bad year-to-year stochastic noise – yes, sometimes it’s just randomness
Do some programs SOAP every single year because of poor reputation, malignant culture, or terrible leadership? Yes. And you should absolutely be wary of chronic multi-spot SOAP offenders with terrible scuttlebutt.
But painting all SOAP programs with the same “garbage” brush is childish. It also hides a harder truth: many people calling SOAP spots garbage are really just angry those programs weren’t in the list they originally applied to. It’s about status, not quality.

The Real Risk: Not Using SOAP Because of Pride
Here’s the scenario I’ve watched play out more than once:
- Student A doesn’t match categorical IM after chasing mostly big-name academic programs.
- They’re stunned Monday of Match Week.
- Their school says: “We’ll help you SOAP into prelim IM, FM, transitional, etc.”
- Student A: “I’d rather reapply next year than take something I don’t want. SOAP is for desperate people.”
Fast-forward:
- Next year, they’re one year further from clinical training.
- Red flags: gap year, no new LORs from rotations, limited new research.
- Competition is the same or worse.
- They don’t match again because now they’re “older applicant with a gap.”
- Now they’re two years removed from med school. Match odds crater. Visa/IMG issues get worse. States start questioning training currency. Doors close.
Compare that to Student B:
- Same stats, same failure to match.
- They SOAP into a prelim IM spot at a decent community hospital.
- They show up, work hard, get strong letters, crush Step 3.
- They reapply in the fall to categorical IM or another field with those new letters and real US clinical experience.
- They match categorical the following year into a solid program.
Did Student B love SOAPing into prelim IM? Of course not. But they understood the difference between an emotional reaction and an actual strategy.
SOAP is often the least risky option on the table, especially for:
- IMGs
- DOs targeting MD-heavy fields
- Applicants with any Step failures
- Anyone who is not independently wealthy and cannot burn multiple years reapplying
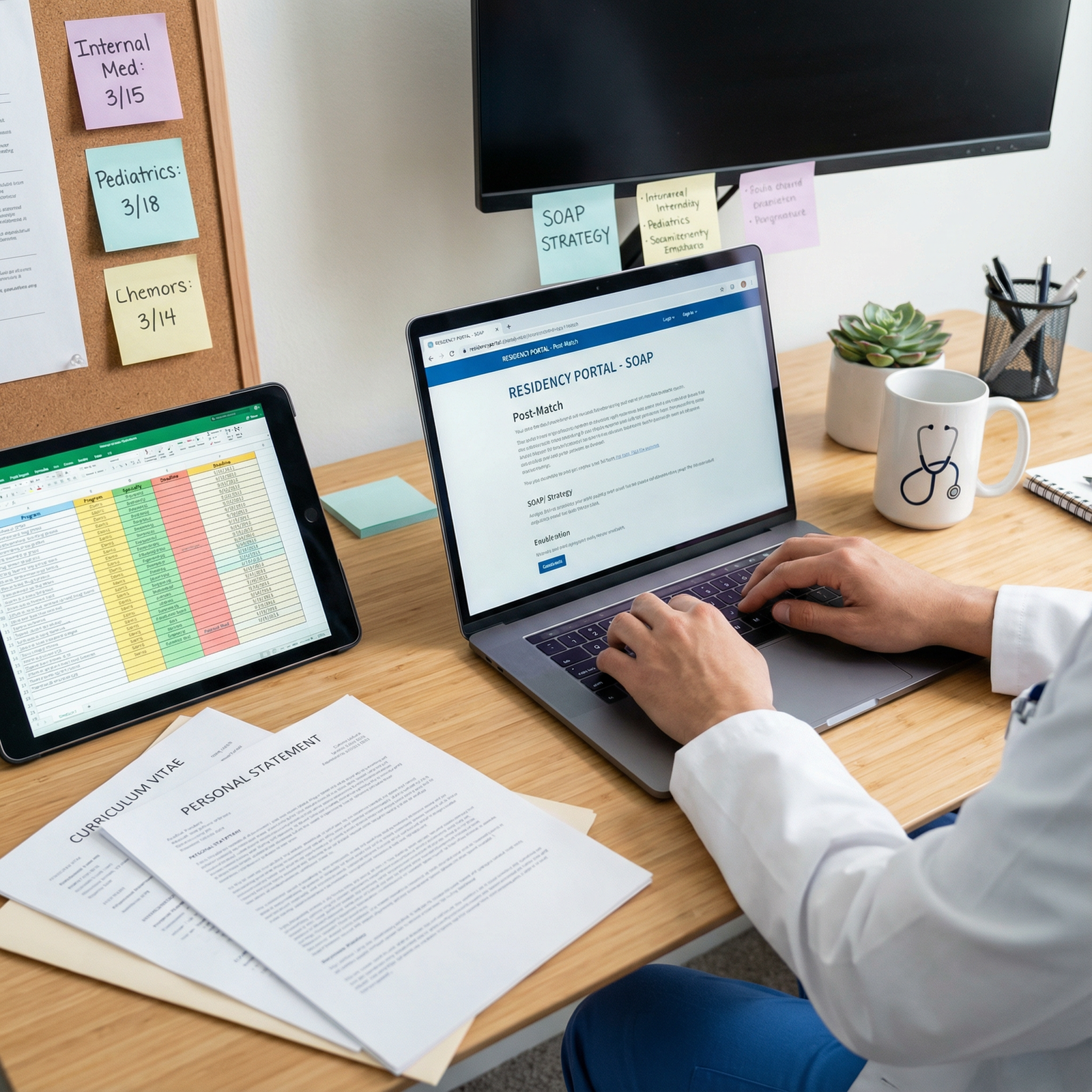
How Smart Applicants Use SOAP Strategically
If you’re serious about not wasting years of your life, you plan for SOAP before you ever need it.
That’s not pessimism. That’s risk management.
1. You mentally rehearse the Monday email
You tell yourself in advance:
“If I get the ‘You are NOT matched’ email, I will give myself 30–60 minutes to be upset, then I will pivot immediately to SOAP. Emotion later, logistics now.”
The people who freeze and waste Monday afternoon are usually the ones who never allowed the possibility in their head.
2. You scout likely SOAP targets ahead of time
You look at:
- Programs that frequently have a small number of SOAP spots (1–3) but aren’t universally hated
- States/regions you’d realistically move to, even if they weren’t your top choices
- Prelim and transitional year programs that could be a launchpad
You do not need a 50-program spreadsheet. But having a sense of realistic options beats staring at the vacancy list for the first time while your dean is calling you.
3. You drop the prestige obsession
You stop asking, “Will people judge me for going there?” and start asking, “Can I get solid training here, avoid abuse, and build a career?”
Red flags to consider: chronic unfilled large numbers of spots, toxic Glassdoor/SDN chatter that’s consistent over years, ACGME citations, 100% attrition of residents from certain classes. Those matter.
Name-brand snobbery doesn’t.
What Actually Happens After You SOAP In
This is where the myth really collapses.
Here’s what your life looks like if you SOAP into a halfway decent program:
- July: You show up for orientation. Nobody introduces you as “the SOAP resident.” They introduce you as “Dr. X, one of our new interns.”
- First 3 months: You’re overwhelmed, just like everyone else. You’re learning workflows, trying not to miss sepsis, and figuring out how to staff new admits at 2 a.m. Nobody cares about your Match status. They care if you answer your pager.
- 6–12 months: Your identity at the program is now based on how you work, whether nurses trust you, whether seniors want you on their team, whether attendings write, “Hard-working, clinically sound, pleasant to work with” or “Frequently late, disorganized, defensive.”
- PGY-2/3: If you want to switch specialties, apply for fellowships, or move programs, what matters most is your performance during residency plus your board exams.
The SOAP label fades shockingly fast in real life. The “desperate applicant” label survives mostly in Reddit comments and applicant gossip, not in actual hospitals.

| Step | Description |
|---|---|
| Step 1 | Unmatched on Monday |
| Step 2 | Enter SOAP |
| Step 3 | Accept prelim/categorical spot |
| Step 4 | Intern year performance |
| Step 5 | Reapply to new specialty |
| Step 6 | Continue in same program |
| Step 7 | Apply to fellowship |
| Step 8 | Matched into new program |
| Step 9 | Graduate, board certified |
| Step 10 | Fellowship training, career |
| Step 11 | Next step? |
When SOAP Might Not Be the Best Move
Let’s be fair: SOAP isn’t always the right call.
Situations where passing on SOAP can be reasonable:
- You only qualify for programs that are clearly malignant (documented abuse, mass resignations, serious probations)
- You’re an exceptionally strong applicant who swung at an ultra-competitive specialty and you’re willing and able to pivot completely (e.g., take a solid research year in that field with a credible mentor and concrete reapplication plan)
- Visa or personal constraints make specific SOAP programs practically impossible
- You have an ironclad plan with departmental backing for a structured gap year that genuinely improves your application, not just “I’ll do some research and hope”
But that’s not most people. That’s the top 5–10% of unmatched applicants with unusually strong institutional backing.
For the majority, “I’ll just sit out and come back stronger” is a story they tell themselves without any realistic plan or numbers to back it up.
The Real Myth: That You’re “Above” SOAP
Let me reframe this:
SOAP is not for “desperate” applicants.
SOAP is for applicants who are honest enough to admit they want to be doctors more than they want to protect their ego for one bad week in March.
Every year, solid residents, future fellows, and future attendings enter medicine through SOAP. Their patients don’t care. Their colleagues barely remember. Their careers move on.
Every year, other unmatched applicants—often just as capable—decide they’re too proud for SOAP. A few recover. Many don’t.
You get to choose which group you want to be in.
| Factor | Use SOAP Now | Skip SOAP / Reapply Later |
|---|---|---|
| Start training | July this year | 1+ year delay |
| Financial impact | Salary + benefits sooner | Extra year(s) loans, no income |
| Risk of never matching | Lower, if you get any spot | Higher with each gap year |
| Ego comfort this week | Lower | Higher (short-term only) |
| Long-term career | Mostly unaffected if you perform | Can be damaged by gaps/age |
FAQ (4 Questions)
1. If I SOAP into a prelim year, am I stuck without a categorical spot forever?
No. Plenty of people SOAP into prelim IM or surgery, then use that year to strengthen their application: strong letters from U.S. attendings, better clinical narrative, Step 3 passed, tangible performance data. They then reapply to categorical positions—either in the same specialty or switching—often with much better odds than if they’d sat out entirely. It’s not guaranteed, but it’s a far stronger position than “unmatched with a gap.”
2. Do programs look down on applicants who went through SOAP?
Good programs mostly care about whether you’re competent, reliable, and not a nightmare to work with. Some old-school PDs have biases, but they usually don’t know or don’t dwell on SOAP history if your training record and letters are strong. If a place fixates on how you got your PGY-1 instead of what you did with it, that’s probably not a place you want to build a career anyway.
3. Should I avoid SOAPing into a specialty I’m not sure I want long-term?
You need to be honest about your tolerance for pivoting. SOAPing into FM or IM when you truly hate primary care is a bad idea. But SOAPing into IM when you’re open to hospitalist work, heme/onc, cards, pulm/crit, etc., is often a smarter play than sitting out. Same with prelim surgery if you’re realistically open to other procedural fields. The key question: “Would I rather do this training than risk never practicing at all?”
4. How do I prepare for SOAP without being pessimistic?
You treat it like insurance. You don’t buy car insurance because you expect to crash; you buy it because you’re not arrogant enough to assume you’re immune to randomness. Same logic here: have an updated CV, a generic but solid personal statement variant for a backup field, and a short list of regions/program types you’d accept. If you never need it, great. If you do, you’re not trying to rebuild your life in a 48-hour panic.
Key takeaways:
- SOAP is not a mark of desperation; it’s a structured second chance that many solid physicians quietly use.
- The real career risk isn’t entering SOAP—it’s refusing to use it out of pride and then compounding that with gap years and worsening odds.
- If your goal is to actually become a practicing physician, treating SOAP as a serious option—not a shameful last resort—is simply rational.






















