The default way people try to build physician-to-physician platforms is wrong. They think “LinkedIn for doctors” or “Uber for locums” and ship yet another generic directory with messaging. Then they wonder why engagement flatlines and CAC explodes.
Physician-to-physician marketplaces have their own architecture, their own gravity. If you ignore the underlying design patterns, you will burn 2–3 years and several million dollars just rediscovering them the hard way.
Let me walk through the patterns that actually work.
1. The Three Archetypes of Physician-to-Physician Platforms
You are not building “a platform.” You are building one of three archetypes, whether you admit it or not. Each has different economics, trust dynamics, and failure modes.
1. Expert Networks vs Labor Marketplaces vs Infrastructure Networks
Most physician-to-physician products fall into one of these:
Knowledge / expert networks
- Examples: MDCalc’s clinical decision ecosystem, specialty-specific expert consult networks, asynchronous lesion review platforms.
- Core transaction: clinical insight, second opinions, case review, or micro-consults between physicians.
- Value driver: access to very specific brains, not generic “social”.
Labor / coverage marketplaces
- Examples: locums platforms, physician-to-physician cross-coverage networks, telehealth “backup call” pools.
- Core transaction: time and presence (clinic hours, call shifts, tele-consults).
- Value driver: predictable, trustworthy coverage with low administrative friction.
Infrastructure / shared services networks
- Examples: physician groups sharing credentialing staff, QA reviewers, billing/coding experts, peer-review boards, niche procedural collaboratives.
- Core transaction: shared capacity and capabilities (review, credentialing, QA, protocols).
- Value driver: scale and standardization among independent physicians.
You can blend them, but only one should dominate your early product. If you are trying to be all three in the first 24 months, you are already dead.
2. Core Marketplace Design Patterns That Actually Matter
Let’s get concrete. The following patterns show up in almost every physician-to-physician marketplace that survives beyond the vanity-metrics stage.
2.1 Identity and Credentialing as a First-Class Primitive
For a physician-to-physician marketplace, “user = NPI-backed identity.” Not an email. Not a phone number. A verifiable clinical identity.
This is not a “nice to have.” It shapes everything:
- Onboarding flows
- Reputation systems
- Matching rules
- Legal and malpractice framework
- Even the UI copy (you are not dealing with “users,” you are dealing with licensed clinicians who can lose their livelihoods)
Pattern: Credentialed Account Object
Every physician account needs a structured credential spine that lives at the center of your data model:
| Field Group | Examples |
|---|---|
| License | State(s), number, status |
| NPI | Individual NPI, taxonomy |
| Board Status | Board(s), expiration dates |
| Privileges | Facility list, privilege type |
| Specialty Depth | Primary, subspecialty, focus |
Do not let this live as a blob of “profile text.” Make it structured, versioned, and updatable with audit history.
Design choices that are usually wrong:
- Letting physicians self-assert board status without verification.
- Not explicitly modeling what they are privileged to do (procedures, modalities, settings).
- Treating “cardiologist” as a flat label instead of a node with subspecialties (EP, interventional, HF, imaging).
You are building the substrate for automated trust. That means the credential spine must exist and be central.
2.2 Reputation: Structured, Not Star Ratings
Star ratings work for restaurants. They are garbage for physician-to-physician platforms.
You need reputation dimensions, not one-dimensional “4.6/5, great doc” nonsense. Colleagues care about:
- Reliability (show up on time, answer pages, close charts)
- Clinical caliber in a specific micro-domain (e.g., complex revision spine, NICU ventilation, difficult GI cases)
- Communication (handoff quality, clarity, willingness to discuss)
- Documentation and compliance (notes, coding basics, following site protocols)
Pattern: Multidimensional Reputation Matrix
You can approximate it with structured feedback after transactions. For example, on a cross-coverage marketplace:
- Attending A hands off 10 inpatients to Hospitalist B overnight.
- Next morning, A gets a brief, structured rating flow:
- Coverage quality: 1–5
- Communication/handoff back: 1–5
- Documentation completeness: 1–5
- Would you request B again? Yes/No
This feeds a reputation matrix keyed by:
- Specialty
- Setting (ICU vs floor vs tele)
- Time of coverage (days vs nights)
You then rank and match not by “best overall,” but by “best in this setting + gap + time frame.”
Does this add friction? Yes. Does it create defensible matching quality and trust? Also yes. And that is the only reason your marketplace survives after the novelty wears off.
2.3 Supply Liquidity: Panel-Based, Not Free-Form
Most physician platforms drown in a simple trap: too much unstructured supply side noise.
You do not want “any cardiologist.” You want:
- EP coverage at Hospital X, credentialed, at 2–4 PM Thursdays, for device checks.
- An MSK radiologist for MRI reads, licensed in CA, willing to read 15–20 studies/day.
- A breast surgeon willing to be remote second-opinion for N>Y volume with response in 48 hours.
Pattern: Panel-Based Supply
Think “panels” instead of “users”:
- A panel is a defined, structured slice of supply:
- “Interventional radiology procedures at Hospital A”
- “Nocturnist coverage for Community Hospital B”
- “Pathology reviews for Dermatology Group C, 2nd reads only”
Supply signs up into panels instead of unrestricted free listings.
Why this works:
- Forces standardization of expectations, pricing, and response times.
- Makes matching deterministic.
- Lets you report to hospitals or groups with clear SLAs: “This is our nocturnist panel for your facility.”
From a data model standpoint:
- Panels are objects that tie:
- Facility or virtual site
- Modality/service type
- Hours or time windows
- Compensation framework
- Minimum credential profile
Physicians opt into panels, not just “the platform.” This is a big shift in how you design your onboarding and marketplace logic.
2.4 Asynchronous First, Synchronous Second
Synchronous consults (real-time telehealth, live cover, phone calls) are sexy. They also blow up your logistics, legal risk, and scheduling complexity.
Most successful physician-to-physician networks start with asynchronous transactions:
- Chart reviews
- Imaging over-reads
- Second-opinion letters
- Guideline-based case Q&A (“Would you start DOAC in this AF with CKD 4?”)
- Documentation and coding review of batches
Pattern: Asynchronous Core, Synchronous Escalation
Architect your system so the default flow is:
- Asynchronous case submission, with structured clinical data and attachments.
- Asynchronous expert response with clear SLAs (e.g., 24–72 hours).
- Optional escalation to synchronous (video, phone, secure chat) if:
- Case complexity crosses a threshold
- Requesting physician upgrades the case
- Expert requests real-time clarifications
This has three very practical advantages:
- Keeps physician calendars sane.
- Helps you avoid being classified as a direct-to-patient telehealth provider in some regulatory frameworks.
- Makes cross-time-zone collaboration trivial.
If you start with synchronous as the main event, you will hit a wall on scheduling density, no-show risk, and operational overhead by Year 2.
3. Trust, Risk, and Regulatory Patterns (Where Most Startups Faceplant)
You cannot “growth hack” your way around regulatory architecture. The design pattern either respects the clinical risk landscape or it collapses under lawyers and insurers.
3.1 Clarify Who Owns the Patient Relationship
The foundational question: in a physician-to-physician interaction on your platform, who is the treating physician?
You have 3 broad patterns:
Primary treats, expert advises
- The local/treating physician retains full responsibility.
- The marketplace expert is explicitly “consultative,” like a curbside.
- Often no direct patient contact.
- Very strong pattern for second-opinion networks and case review platforms.
Shared care with clear role delineation
- Example: remote radiologists who “own” the interpretation but not the patient’s overall care.
- Local physician uses reports to treat.
- Responsibility is split by domain.
Consultant is a treating physician for a narrow scope
- Example: tele-ICU intensivist with direct orders and documentation.
- Expert is part of the active care team.
You must bake this into:
- Your terms of use
- Clinical documentation templates
- UI copy and handoff flows
- What data is shown to whom
Pattern: Role-Explicit Case Objects
Every case object should carry:
- Requesting physician role
- Responding physician role
- Legal classification: advisory vs consult vs direct care
- Jurisdictional context (state, facility, telehealth designation)
Your platform logic must enforce constraints. For example:
- Advisory-only interactions cannot auto-generate patient-level orders or prescriptions.
- Direct-care consults may require additional consent and documentation workflows.
If you fudge this, you are playing malpractice roulette.
3.2 Liability Containment: Network vs Group Practice
If you build a physician-to-physician marketplace and accidentally look like an integrated group practice, congratulations: you just took on liability exposure and compliance burdens that will crush your unit economics.
Pattern: Network Architecture with Clear Separation
You want:
- Independent physicians (or groups) connected by your platform.
- The platform is a facilitator, not the billing entity or employer (at least initially).
- Contracts and flows that make it clear you are not practicing medicine.
Do not:
- Force standardized medical decision pathways that remove individual physician judgment.
- Blend clinical documentation in a way that makes “the platform” look like a co-actor.
- Control day-to-day scheduling and protocols so tightly that regulators see it as de facto employment.
You can eventually move up the stack to MSO structures, business associates, or even risk-bearing entities. But in the post-residency / early job-market phase, you want to stay light: network, not monolith.
3.3 Payment Architecture: Who Pays, For What
Physician-to-physician marketplaces have messy payer flows. You need to lock down the model early:
Four common archetypes:
B2B Facility/Group Pays (best starting point)
- Hospital pays for remote cross-coverage pool.
- Group pays for external second-opinion network or QA reviewers.
- Clean, predictable, no patient billing.
Physician Pays (rarely works unless ROI is immediate)
- A solo doc pays for second reads or complex case consults.
- Works only when a) reimbursement is higher with help, or b) potential downside of error is huge.
Patient Pays, but you route to physicians
- Second-opinion platforms where patients pay, but your core network is physicians.
- You still must be very clear about treating vs advisory roles.
Payer/plan pays
- Health plans sponsor narrow-network expert panels for specific conditions.
- Complex but very defensible if outcomes data are strong.
Pattern: Decouple Marketplace Matching from Payment Rails
At the architecture level:
- Matching and communication live in one subsystem.
- Payment, invoicing, and reconciliation live in another.
That gives you flexibility to:
- Start with facility-paid pilots (easier sale).
- Later layer in per-case payment, bundles, or subscription access.
- Handle scenarios where the requesting doc never directly pays you.
Do not hard-wire “the doctor pays at checkout like DoorDash.” That is not how clinical budgets work.
4. Supply-Side Design: Making It Work for Real Physicians
If you are building post-residency and job-market tools, let me be blunt: physicians have been burned by garbage platforms. They assume your product will waste time and pay poorly.
Your design patterns need to signal the opposite.
4.1 Time Respect: Batchable, Predictable Work Units
The design principle: physicians think in blocks—clinic sessions, OR blocks, call nights. They do not think in random 7-minute micro-tasks.
Pattern: Block-Structured Work Units
Even for remote or async work:
- Batch imaging reads into predictable blocks (e.g., 90 minutes, 20–30 studies).
- Bundle case reviews into “10 chart review” packets instead of random trickle.
- For cross-coverage, allow physicians to commit to full “micro-shifts” (e.g., 7p–11p tele-cover).
Architect your marketplace around “blocks”:
- A block has:
- Start/end time (or start + typical duration).
- Volume expectation (N cases).
- Compensation and penalties if blocks are abandoned.
This aligns nicely with job-market realities. A physician picking up extra work on your marketplace wants something that fits around their existing clinical load. Not an endless stream of tiny tasks.
4.2 Communication Surfaces: Tight and Contextual
You must kill random messaging. Physicians do not want an inbox. They want case-contextual communication.
Pattern: Case-Scoped Conversations
Design:
- Every message thread is attached to a specific case, panel, or block.
- No free-floating DMs without a clinical or business object anchor.
- Handoffs and escalations are structured flows, not ad hoc chats.
For example:
- Covering hospitalist B ends shift.
- Handoff to day hospitalist A is a structured checklist:
- “Patients needing immediate follow-up”
- “Pending studies”
- “Unresolved issues”
- Messaging adds nuance, but the structure is enforced.
This lowers cognitive load and massively simplifies medico-legal discovery if anything goes wrong.
4.3 Onboarding Pattern: Seed High-Intent Micro-Communities
The worst onboarding pattern: “Any doctor can join from anywhere, here’s your profile, good luck.”
You will get a ghost town with scattered users and no liquidity.
Pattern: Micro-Community Seeding
Approach:
- Pick a narrow specialty + use case + geography or virtual setting combination.
- Example: “Academic and high-volume community GI groups in 3 states for advanced polypectomy second opinions.”
- Seed:
- 10–20 high-caliber experts
- 20–50 high-intent referrers
- Give them workflows that solve a painful, daily problem.
- Only after this micro-community stabilizes, expand adjacently:
- Same specialty, new geography
- Related specialty, same facilities
- New but related use case, same network
This aligns with classical marketplace “bowling pin” strategy, but the underlying reason in medicine is more specific: physicians adopt what their close peers are visibly using successfully. Adoption is tribal.
5. Demand-Side Design: Who You Actually Serve
You say “physician-to-physician” but your economic buyer is often not the individual doctor.
Three demand patterns show up over and over.
5.1 Facility-Centric Demand: Hospital and ASC Use Cases
Hospitals and ASCs do not care about your “community” pitch. They care about:
- Coverage gaps (nights, weekends, holidays, rare subspecialty).
- Throughput (faster reads, quicker consults, shorter LOS).
- Compliance and quality metrics (stroke door-to-needle, cath lab appropriateness, readmissions).
Pattern: Coverage & Throughput Use Cases
Design cases like:
- “Guaranteed 24/7 teleneurology coverage for stroke.”
- “Remote ICU panel to backstop community hospital nights.”
- “24–48 hour turnaround for tertiary-level pathology review.”
You then market your physician-to-physician network as:
- A reliability layer.
- A quality amplification layer.
- A risk reduction tool.
The platform patterns we talked about—credential spine, panel-based supply, structured reputation—are what make those claims credible.
5.2 Group-Centric Demand: Independent Practices and Mega-Groups
Independent physician groups have different pain:
- Burnout from call schedules.
- Recruiting headaches for subspecialties.
- Need for quality review and clinically credible second opinions to defend their work.
Pattern: Peer Extension Network
You design:
- Shared call pools across friendly groups with agreed protocols.
- External QA review panels for complex imaging or procedures.
- Subspecialty “borrowed expertise” networks (“we are a general ortho group, we tap your foot/ankle expert for X% of cases”).
The platform logic is identical to before—panels, case-scoped messaging, block-structured work—but the economic pitch is “keep your independence, extend your capability, reduce burnout.”
5.3 Individual Physician Demand: Career and Income Architecture
Post-residency physicians are in a cynical, practical headspace:
- They have seen EMRs break their workflow.
- They have watched locums platforms screw them on pay transparency.
- They have zero interest in another passive profile they must “maintain.”
So the design pattern is simple:
Pattern: Alternate Income and Career Flexibility Layer
Your platform must:
- Offer clear earning pathways: “2 weekend nights/month = $X K/year.”
- Offer control: “You set your availability blocks; no random texts at 10 p.m.”
- Offer CV value: “Being part of this expert network means something—board reviewers, QA leadership, named expert panels.”
You are competing not just with other apps, but with the default: picking up an extra employed shift, moonlighting, or doing nothing and preserving sanity. Your UX, reputation system, and block design must reflect that reality.
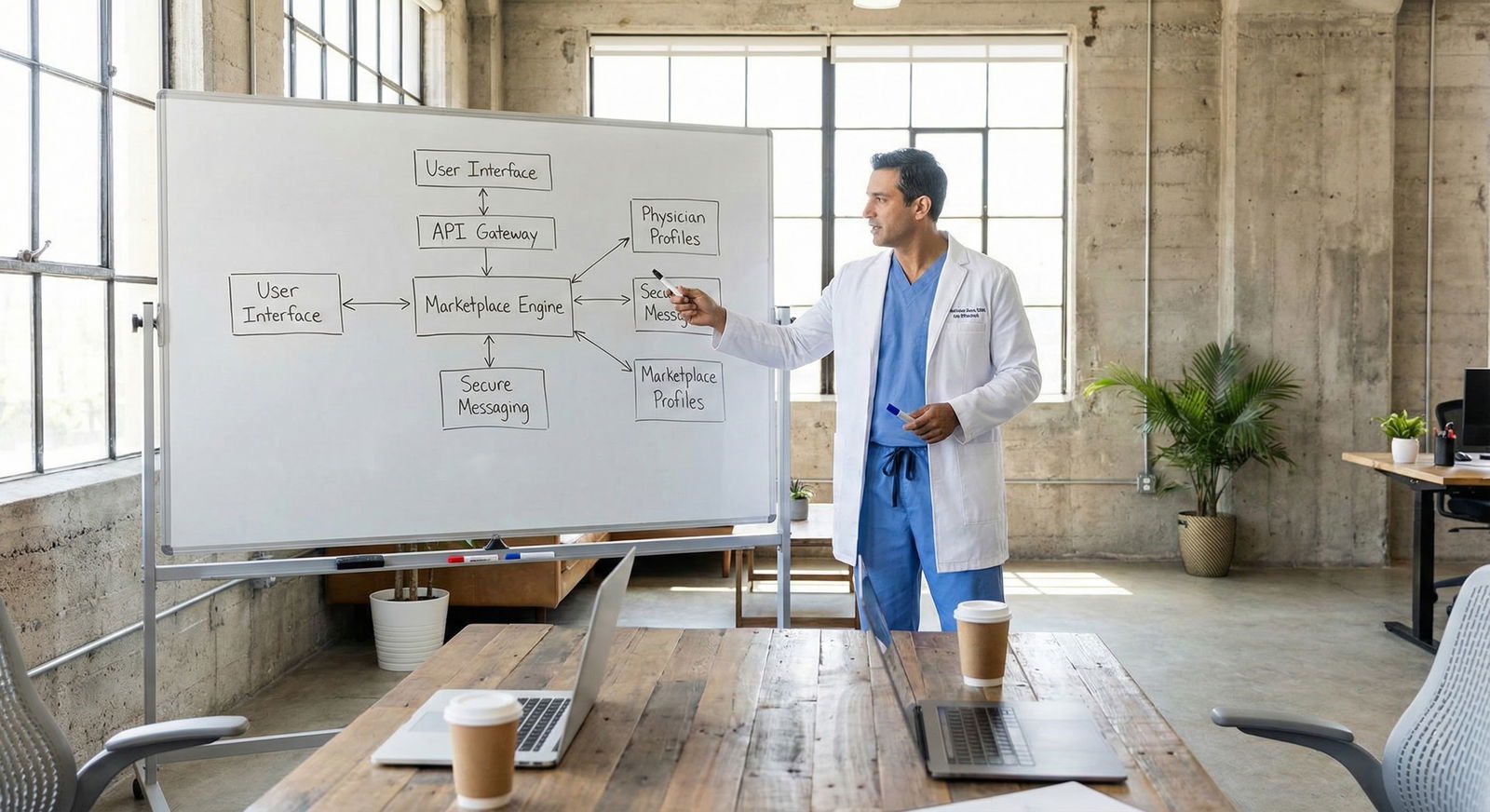
6. Technical and Product Design Patterns Under the Hood
This is where platform choices directly impact regulatory and product realities.
6.1 Event-Driven Case Lifecycle
Physician-to-physician interactions are not linear. Cases get escalated, handed off, re-reviewed months later in QA.
Pattern: Event-Sourced Case Engine
Instead of storing just “case state,” store a full event stream:
- CaseCreated
- DataAttached (labs, imaging, notes)
- ExpertAssigned
- OpinionSubmitted
- HandoffInitiated
- HandoffCompleted
- EscalatedToSynchronous
- QAReviewAttached
- CaseClosed
Benefits:
- Perfect audit trail.
- Easy reconstruction in discovery or internal reviews.
- Fine-grained metrics for throughput, delays, failure points.
Combine this with strongly typed roles (requesting vs responding physician roles) and you now have a compliant, debuggable clinical engine, not a chat app with PDFs stapled on.
6.2 Structured Clinical Data First, Free Text Second
If you allow “upload PDF and type note” as your primary interaction, your analytics and quality efforts will be crippled.
Pattern: Template-Driven Case Intake
For each panel/use case, define:
- Minimum structured fields (age, key comorbidities, relevant labs, prior interventions).
- Standard attachments (DICOM, op notes, pathology reports).
- Clear question from requesting physician (“decision point”).
Yes, you allow free text. But every free text field is anchored to a context, not a blank canvas.
Your future product wins come from this:
- Suggest similar historical cases.
- Surface guidelines or order sets in-line.
- Flag incomplete data before assignment to expert.
This also prevents a very real social dynamic: experts refusing to engage because “the referral is garbage and missing everything I need.” You can design around that.
6.3 Interoperability Patterns: Minimum Viable Integration
You will be tempted to promise full EMR integration early. Resist that.
Pattern: Lightweight Integration First
Focus on:
- Secure data ingress/egress via FHIR or SFTP for studies and documents.
- Simple EHR launch links (SMART on FHIR where possible) to open your app with context.
- PDF or structured note export back into EMR.
Think “sidecar,” not “replacement.” Your physician users live in Epic/Cerner/etc. Your platform should slide along the side, not try to be the main interface.
Longer term, you can:
- Automate patient roster pulling for coverage.
- Auto-push case notes back into EMR as discrete data.
- Build guardrails that sit inside EHR (e.g., soft-interrupt suggestions).
But for a post-residency/early job-market startup, chasing full EHR integration as a precondition is a classic way to die before PMF.
7. Concrete Design Example: Cross-Coverage Marketplace
Let me stitch this together with a specific pattern: a physician-to-physician cross-coverage platform.
Goal: Allow Group A to offload some night/weekend call to external physicians in a safe, reliable way.
Design using the patterns above:
Credential Spine
- Verify license, NPI, board, privileges for all covering physicians.
- Model which hospitals they are already credentialed at vs tele-only coverage.
Panels
- Create discrete panels:
- “Hospitalist nights at Community Hospital 1 (tele + phone, no in-person).”
- “Cardiology phone backup for Hospital 2.”
- Standardize expectations per panel (N patients, call volume, typical issues).
- Create discrete panels:
Block Work Units
- 7p–7a blocks with clear pay.
- Offered to vetted physicians with prior reputation above threshold.
Case-Scoped Interactions
- Every patient contact generates a case:
- Handoff from local to covering physician.
- Event stream of interventions overnight.
- Morning handoff back with structured checklist.
- Every patient contact generates a case:
Role-Explicit Cases
- Local physician is primary.
- Covering physician is clearly designated as cross-covering under group protocols.
- Documentation template reflects this.
Reputation Matrix
- Post-block feedback:
- Reliability, communication, documentation.
- Panel-specific reputation (night hospitalist, not generic “internist”).
- Post-block feedback:
Payment
- Hospital or group pays platform; platform pays physicians.
- Individual physicians never pull out a credit card.
You now have a repeatable pattern you can clone into other specialties and sites. That is how you scale.
8. Metrics That Actually Indicate Product–Market Fit
You can ignore most vanity metrics. For physician-to-physician platforms, these are the telling ones:

| Category | Repeat Requesting Physicians | Average Cases per Active Expert |
|---|---|---|
| Month 1 | 5 | 1 |
| Month 2 | 12 | 3 |
| Month 3 | 18 | 5 |
| Month 4 | 25 | 7 |
| Month 5 | 33 | 9 |
| Month 6 | 40 | 11 |
Metrics that matter:
- Ratio of repeat to first-time requesting physicians. If it is not climbing, your core experience is weak.
- Cases per active expert per month, by panel. Too low = no liquidity, too high = burnout risk and quality drops.
- Time from case creation to expert assignment, and assignment to first response.
- Handoff completion rates and missing-data rates on intake.
- Panel fill rates (how many of your defined panels are consistently staffed).
If your graph looks like:
- High initial signups
- Low repeat usage
- Cases clustering around a handful of experts
…then you are not running a marketplace; you are running a glorified consulting agency.
9. Common Failure Patterns to Avoid
You will see these again and again. Avoid them on day one.
Generic “professional network” UX
- Feeds. Likes. Comments. DMs.
- None of that maps to actual clinical workflows or revenue.
No opinion about specialty granularity
- Treating “cardiology” or “surgery” as monoliths.
- You end up mismatching needs and expertise.
Legal ambiguity on roles
- “This is just educational!” stamped somewhere in the footer while clearly shaping critical decisions.
- Plaintiffs’ lawyers love this.
Over-optimizing for growth over trust early
- Letting anyone sign up and “be available.”
- Not enforcing credentialing rigor to juice numbers.
Trying to own billing too early
- Getting into claims submission and reimbursement optimization before you even have stable use cases.
- You add a second startup’s worth of complexity instantly.
10. Putting It Together: Your Next Moves as a Post-Residency Founder
If you are just out of residency or early in your attending career and thinking about building one of these platforms, your advantage is clinical reality. You know which workflows are broken. Use that.
Start here:

| Step | Description |
|---|---|
| Step 1 | Pick 1 use case |
| Step 2 | Define panel and block structure |
| Step 3 | Design credential spine |
| Step 4 | Implement case event engine |
| Step 5 | Seed 1 micro community |
| Step 6 | Measure repeat use and panel fill |
| Step 7 | Expand adjacent panel |
| Step 8 | Fix workflow and incentives |
| Step 9 | Good retention? |
Couple of specific, tactical suggestions:
- Pick a use case where asynchronous makes sense and risk is bounded. Imaging, pathology, chart QA, and second opinions are good starting points.
- Hard-code structured clinical intake and role-definition from day one. Retrofits are painful.
- Do not be shy about saying no to physicians who want unstructured “consult by text.” That is how you destroy your own defensibility and compliance.
- Talk to hospital CMOs and medical directors early. Listen for phrases like “our cardiologists are drowning in call” or “we send all these cases to Big Academic Center X and wait 3 weeks.” Those are gold.
If you design your physician-to-physician marketplace around these patterns—credential spine, panel-based supply, block work units, role-explicit case flows, structured reputation—you are not just building an app. You are building clinical infrastructure.
With that foundation, you are in a position to tackle harder problems: risk-sharing, outcomes-based contracts, integrated tele-ICU networks, even physician-led virtual specialty hospitals. But that is a different layer of complexity, and a story for another day.

| Category | Value |
|---|---|
| Knowledge/Expert Network | 35 |
| Labor/Coverage Marketplace | 45 |
| Infrastructure/Shared Services | 20 |