
Understanding Physician Salaries: Key Factors Every Trainee Should Know
Physician salaries sit at the intersection of medical specialties, healthcare economics, and individual career choices. For medical students, residents, and fellows carrying substantial educational debt, having a clear, realistic understanding of earning potential is not just interesting—it is essential for long‑term financial planning and career satisfaction.
Physician compensation is shaped by a complex mix of factors: specialty choice, practice setting, geography (including Rural Healthcare opportunities), reimbursement structures, and evolving healthcare policy. Layered on top of that are personal choices about lifestyle, workload, and risk tolerance.
This guide breaks down the major drivers of physician salaries and offers practical, actionable advice to help you align your clinical interests with your financial and personal goals.
1. Medical Specialty: The Primary Driver of Physician Salaries
Among all the variables affecting compensation, medical specialty is consistently the single strongest predictor of income.
1.1 High‑Earning vs Moderate‑Earning Medical Specialties
While specific numbers change year to year and by survey, typical patterns in physician salaries include:
- Higher‑earning specialties often include:
- Orthopedic surgery
- Plastic surgery
- Cardiology (especially interventional)
- Gastroenterology
- Dermatology
- Radiology
- Anesthesiology
- Ophthalmology
These fields often report total compensation (salary + bonuses + incentives) in the $450,000–$700,000+ range, especially for experienced physicians in high‑demand markets.
- Moderate‑earning specialties typically include:
- General internal medicine
- Family medicine
- Pediatrics
- Psychiatry
- Hospital medicine
- Infectious disease
- Endocrinology
- Geriatrics
These specialties often fall in the $220,000–$320,000 range, depending on region, practice model, and call responsibilities.
While primary care tends to earn less per physician, it plays a central role in healthcare delivery and can still be financially rewarding—especially with loan repayment, leadership roles, or ownership in group practices.
1.2 Why Specialty Choice Affects Compensation
Several structural and economic reasons explain the differences in physician salaries across specialties:
Length and intensity of training
- Longer residencies and fellowships (e.g., surgical subspecialties, interventional fields) often correlate with higher pay.
- These specialties incur a greater “opportunity cost” (more years training at lower pay), which the market partially offsets with higher post‑training compensation.
Procedural vs cognitive work
- Procedure‑heavy specialties (orthopedics, interventional cardiology, GI) are reimbursed at higher rates under fee‑for‑service models.
- Cognitive specialties (general internal medicine, rheumatology) rely more on evaluation and management (E/M) codes, historically reimbursed less generously.
Revenue generation per hour
- Procedural work typically generates more billable RVUs (relative value units) per unit of time.
- High‑throughput procedural practices can produce substantial revenue even with fewer patient encounters.
Malpractice risk and overhead
- Specialties with higher malpractice exposure (obstetrics, neurosurgery) often command higher salaries to offset risk and insurance costs.
- Practices that require expensive equipment or infrastructure (cardiac cath labs, endoscopy suites) also factor in those costs when structuring compensation.
1.3 Procedural vs Non‑Procedural Roles
A useful lens for understanding compensation is whether a specialty is primarily procedural or non‑procedural:
Procedural specialties
- Examples: Surgery, anesthesiology, interventional radiology, urology, GI
- Typically higher base pay plus productivity bonuses
- Work involves discrete billable procedures with defined reimbursement schedules
Non‑procedural/cognitive specialties
- Examples: General internal medicine, endocrinology, psychiatry
- Revenue centers on visits, consults, and chronic disease management
- Time‑intensive relationships and complex decision‑making are essential—but not always reimbursed proportionally
Even within a specialty, your practice focus can matter. For example:
- A cardiologist doing a high volume of interventions will usually earn more than a cardiologist focused on non‑invasive imaging only.
- A dermatologist performing cosmetic procedures (often cash‑pay) may out‑earn one focused entirely on medical dermatology.
1.4 Supply and Demand Dynamics by Specialty
Labor market forces significantly shape physician salaries:
High‑demand specialties
- Primary care, psychiatry, hospital medicine, and many surgical subspecialties often face shortages in many regions.
- Employers respond with higher starting bonuses, loan repayment, and more favorable call arrangements.
Oversupplied markets
- Some subspecialties in urban centers may be saturated, leading to lower starting offers, longer job searches, or the need to consider less competitive locations.
Actionable tip:
Before committing to a fellowship, review:
- National workforce reports (AAMC, specialty societies)
- Job boards for your specialty
- Trends in fellowship fill rates and employment projections
This can help you avoid entering an oversupplied niche without a clear plan.
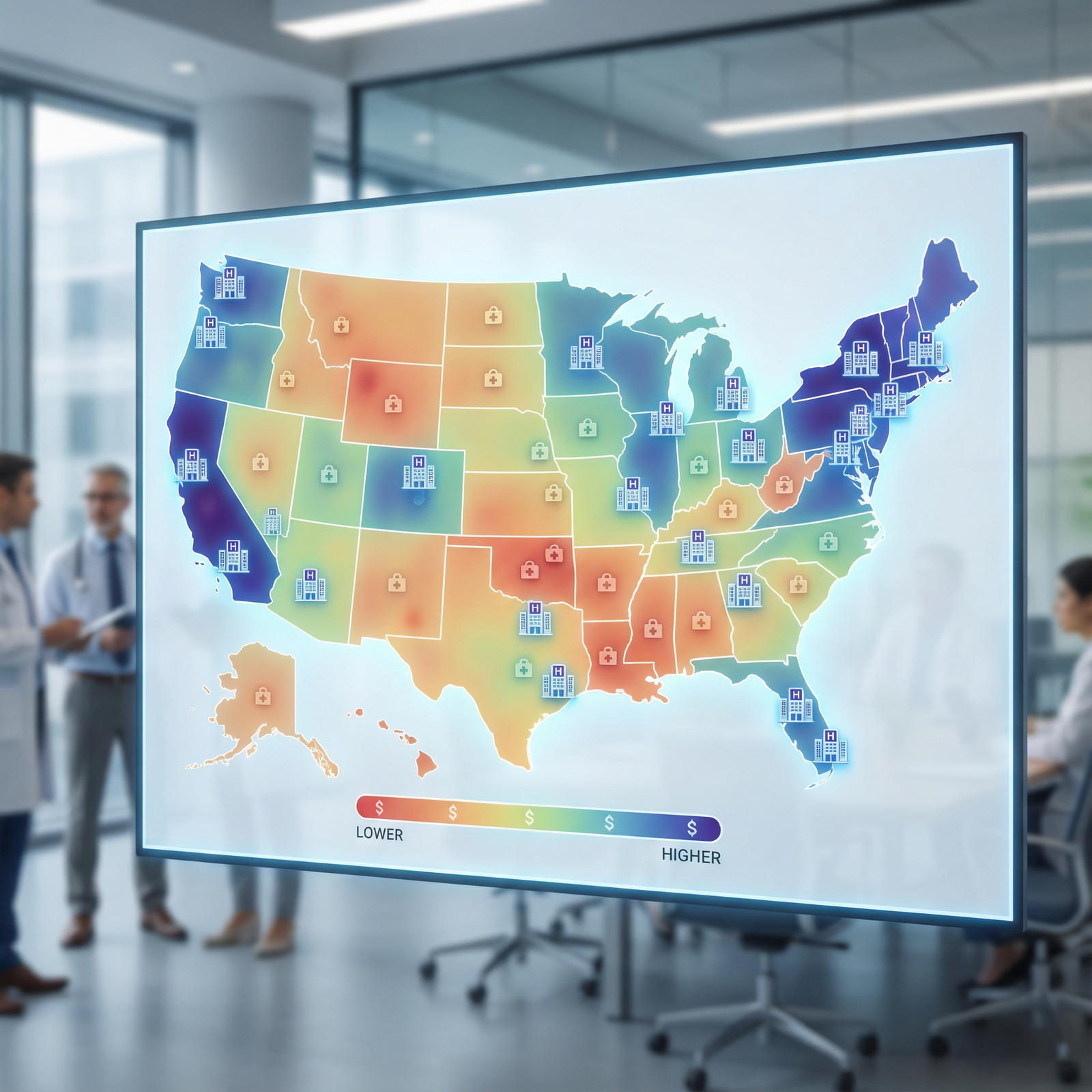
2. Geographic Location: How Where You Practice Affects What You Earn
After specialty, geographic location is often the next most powerful influence on physician salaries. Identical training and skill sets can command dramatically different compensation depending on region, state, and community type.
2.1 Regional Variations and Cost of Living
Compensation surveys consistently show differences between:
High‑paying regions
- Often the Midwest, certain parts of the South, and some non‑coastal states
- Lower cost of living and strong demand can lead to higher income and greater purchasing power
Lower‑paying but high‑cost regions
- Large coastal cities (e.g., San Francisco, New York, Boston) may offer higher nominal salaries but even higher living costs
- After housing, taxes, and childcare, net disposable income may be less than in a lower‑cost region
When evaluating an offer, consider:
- State and local income tax rates
- Housing costs (rent or mortgage per month)
- Student loan repayment strategy (income‑based vs aggressive payoff)
- Commute time and quality of life factors
Actionable tip:
Use cost of living calculators to compare salary offers between regions on an apples‑to‑apples basis. A $260,000 salary in a low‑cost Midwestern city may go farther than $330,000 in a high‑cost coastal metro.
2.2 Rural Healthcare vs Urban Practice
The Rural Healthcare landscape presents unique opportunities and trade‑offs that strongly affect physician salaries:
Rural and underserved areas often offer:
- Higher base salaries and signing bonuses
- Loan repayment programs (federal, state, or employer‑sponsored)
- Stipends for residents/fellows who sign early
- Relocation assistance and housing allowances
- Faster pathways to leadership roles (medical director, department chair)
Professional experiences in rural practice may include:
- Broader scopes of practice and more procedural opportunities, particularly in primary care
- Closer relationships with patients and community members
- Fewer subspecialists on site, requiring more generalist management and telehealth collaborations
Challenges to consider:
- Potential for more call or fewer backup resources
- Limited access to certain amenities or dual‑career opportunities for partners
- Distance from academic hubs, which may impact research or teaching goals
For many physicians, a 3–5 year commitment to rural practice can significantly accelerate debt repayment and savings, putting them in a stronger long‑term financial position—even if they later transition back to urban practice.
2.3 State Policies, Payer Mix, and Healthcare Economics
State‑level factors can substantially influence physician salaries:
Medicaid expansion and reimbursement rates
- States with more generous Medicaid and higher reimbursement can improve overall practice revenue.
- Safety‑net and academic centers in non‑expansion states may face more financial pressure, sometimes translating to lower offers.
Malpractice climate
- States with tort reform and lower malpractice premiums can attract certain specialties and indirectly support more competitive salaries.
- High‑litigation environments can increase overhead and affect specialty distribution.
Payer mix in your community
- Areas with a higher proportion of privately insured patients may generate more revenue per encounter.
- Regions with heavy Medicaid/uninsured populations may rely more on subsidies, grants, or hospital support, sometimes limiting salary growth.
3. System‑Level Forces: Reimbursement, Market Competition, and Value‑Based Care
Physician compensation is tightly linked to broader trends in healthcare economics and payment reform.
3.1 Insurance Reimbursement and RVU‑Based Compensation
Most hospitals and large groups now use RVU‑based (relative value unit) or hybrid compensation models:
How RVU models affect your pay:
- Each service or procedure has an assigned RVU value based on time, complexity, and resources.
- Your compensation often includes a base salary plus a productivity component tied to total RVUs generated.
- If payor reimbursement declines, organizations may adjust RVU conversion factors or base salaries over time.
Impact of payer contracts:
- Negotiations with commercial insurers, Medicare, and Medicaid influence how much revenue your RVUs generate.
- Specialties heavily dependent on certain procedures may be particularly sensitive to changes in coverage or coding rules.
Actionable tip:
When evaluating an offer, ask:
- Is compensation guaranteed or RVU‑based?
- What is the RVU conversion rate (dollars per RVU)?
- What have recent changes in payer contracts or Medicare rules done to RVU values in your specialty?
3.2 Competition and Consolidation in the Healthcare Marketplace
The structure of your local healthcare market affects leverage and Salary Negotiation:
Consolidated markets
- Large health systems may control most hospital beds and outpatient clinics in a region.
- Standardized compensation scales can limit flexibility—but may offer better benefits, loan repayment, or academic opportunities.
Competitive markets with multiple employers
- More options can give physicians greater negotiating power.
- Independent groups may offer partnership tracks, profit‑sharing, or ancillary income (imaging centers, ambulatory surgery centers).
Telemedicine and cross‑state practice
- Virtual care has opened new practice models—especially in psychiatry, primary care, and some subspecialties.
- While telehealth income may not always match procedural fields, it adds flexibility and sometimes side‑gig potential for additional income.
3.3 The Shift Toward Value‑Based Care
Payment reform is gradually shifting from volume‑based to value‑based models:
Value‑based care initiatives may:
- Reward quality metrics (HEDIS measures, readmission rates, patient satisfaction)
- Provide bonuses for cost‑effective care and population health management
- Penalize high complication or readmission rates
How this affects individual physicians:
- Compensation plans increasingly mix:
- Base salary
- RVU/productivity component
- Quality or performance bonuses
- Primary care and hospital medicine may benefit more from value‑based structures given their central role in care coordination.
- Compensation plans increasingly mix:
Actionable tip:
When reviewing a contract, ask for:
- The exact quality metrics tied to your bonus
- Historical payout rates (do people actually earn the quality bonus?)
- Support staff and infrastructure to meet quality targets (care coordinators, social workers, data support)
4. Experience, Training, and Professional Differentiation
Beyond specialty and location, your years of experience and additional qualifications play a central role in your compensation trajectory.
4.1 Career Stage and Salary Growth
Physician salaries typically evolve across stages:
Early career (years 1–3 out of training):
- Often includes guaranteed salary with minimal productivity expectations while you build a panel or referral base.
- Signing bonuses and relocation assistance are common.
- Many contracts include a ramp‑up period and then convert to RVU or productivity‑based models.
Mid‑career (years 4–10+):
- Earnings usually peak as your efficiency increases and patient volume stabilizes.
- Partnership or shareholder status in private groups often occurs in this window, potentially increasing income significantly.
- Leadership roles (service chief, medical director) may add administrative stipends.
Late career:
- Some physicians maintain high productivity; others scale back call, procedures, or clinic time.
- Flexible or part‑time schedules may involve lower overall compensation but higher quality of life.
- Experience can translate into lucrative consulting, medico‑legal work, or leadership in healthcare organizations.
4.2 Additional Training, Fellowships, and Certifications
Extra training can be a powerful lever in boosting physician salaries—but only if aligned with market demand:
Fellowship training
- Can open doors to higher‑paying subspecialties (e.g., interventional cardiology vs general cardiology; pain medicine vs general PM&R).
- Adds 1–3+ years of lower earnings during training, so the long‑term payoff should be evaluated carefully.
Subspecialty certification and niche expertise
- Examples: advanced endoscopy in GI, fetal echocardiography in cardiology, complex spine in orthopedics.
- Unique skills can justify higher compensation or better job offers, especially in markets with unmet need.
Non‑clinical skills that enhance compensation
- MBAs or MHAs for leadership roles
- Health informatics or quality improvement expertise
- Research productivity and grant funding in academic settings
- Speaking, writing, or media engagements that support brand and practice growth
Actionable tip:
Before pursuing extra training, ask:
- What are typical salaries for this subspecialty versus the base specialty?
- How many jobs in my preferred region actually require or reward this advanced expertise?
- Can I speak with recent graduates to understand their real‑world job prospects and compensation?
5. Employment Models and Salary Negotiation Strategies
How you structure your work—your employment model—can be as important as what you do.
5.1 Common Physician Employment Models
Hospital or health system employment
- Pros:
- Stable salary, benefits, and malpractice coverage
- Less administrative burden and no need to manage billing or HR
- Often better for work‑life balance and predictable schedules
- Cons:
- Less control over schedule, support staff, and clinical decisions
- Standardized salary bands with less upside potential
- Vulnerable to system‑wide cost‑cutting, RVU target increases
- Pros:
Private practice (solo or group)
- Pros:
- Greater autonomy over scheduling, staffing, and clinical workflows
- Potential for higher income via ownership, profit‑sharing, and ancillary services
- Ability to build and grow your own brand
- Cons:
- Business risk, overhead responsibility, and need for practice management skills
- Income variability, especially early on
- Responsibility for negotiating payer contracts and managing compliance
- Pros:
Academic medicine
- Pros:
- Opportunities for teaching, research, and subspecialty work
- Collegial environment, intellectual stimulation, and academic titles
- Some protection from pure RVU pressure
- Cons:
- Often lower base salaries compared with private practice/hospital employment
- Promotion and salary tied to academic metrics and institutional budgets
- Administrative and research responsibilities on top of clinical time
- Pros:
Locum tenens and per‑diem work
- Pros:
- High hourly or daily rates
- Flexibility in location and schedule
- Opportunities to “test‑drive” different practice settings
- Cons:
- Typically no long‑term benefits (retirement, health insurance, paid time off)
- Uncertainty of long‑term assignments
- Frequent transitions and credentialing requirements
- Pros:
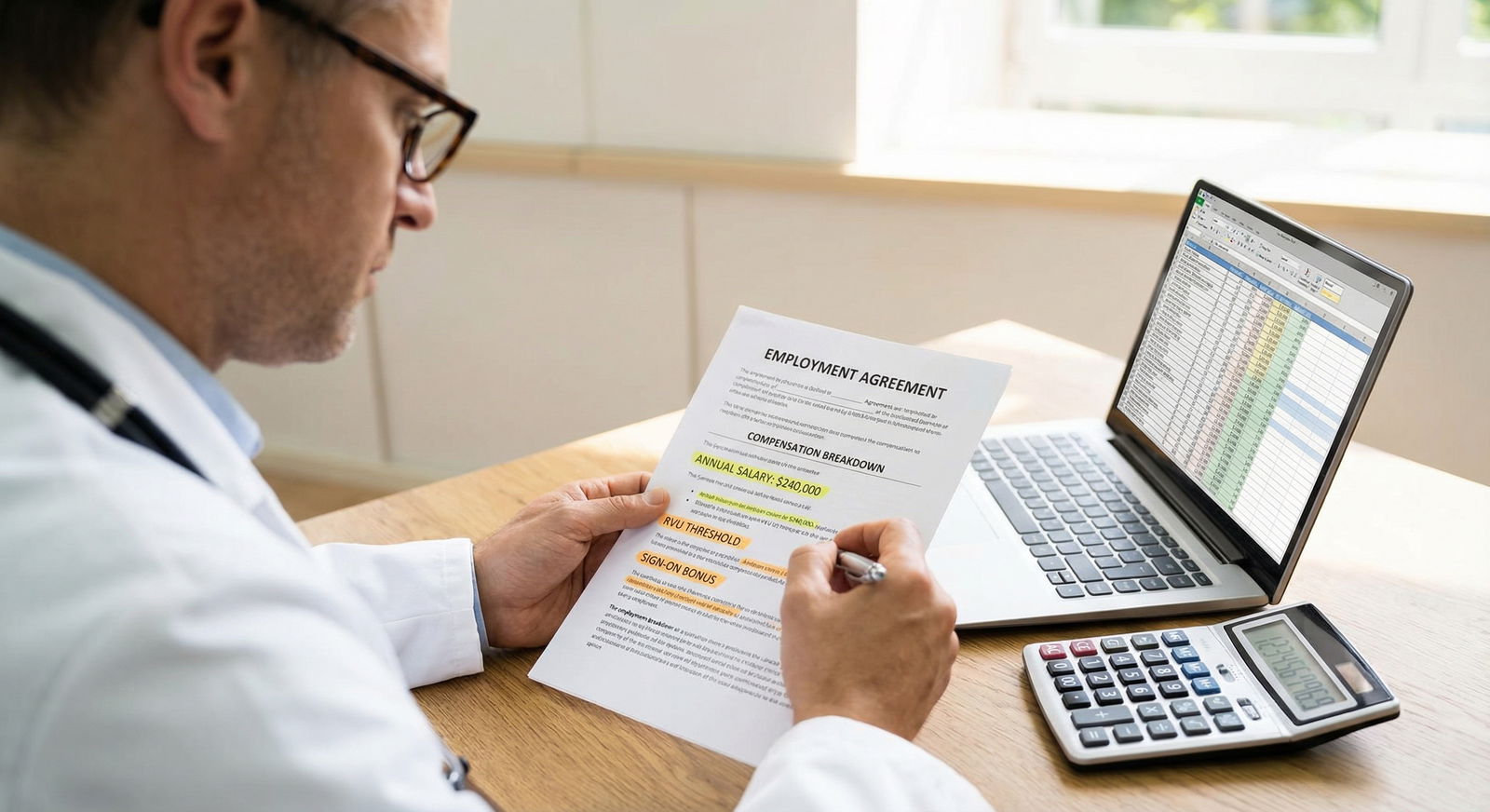
5.2 Core Principles of Physician Salary Negotiation
Regardless of your chosen model, Salary Negotiation skills can materially affect your long‑term financial trajectory.
Key steps:
Know your market value
- Use multiple data sources: MGMA, AAMC, specialty society surveys, and physician compensation reports.
- Filter by region, practice type, and years of experience.
Consider the full compensation package
- Base salary
- Sign‑on bonus and relocation funds
- Loan repayment assistance
- RVU or productivity bonus structure
- Call pay, extra shift pay, or weekend premiums
- CME funds, retirement match, and health benefits
- Tail coverage for malpractice when you leave
Clarify expectations and support
- Panel size expectations or RVU targets
- Staffing ratios (MA, RN, NP/PA support)
- Time for documentation, admin tasks, and non‑clinical work
- Protected time for teaching or research (in academic roles)
Get expert help when needed
- Consider having an attorney experienced in physician contracts review your agreement.
- Ask mentors or senior colleagues to help interpret clauses on non‑competes, termination, and productivity metrics.
Actionable tip:
Negotiate from a mindset of mutual benefit, not confrontation. Emphasize how fair compensation will allow you to build a stable, long‑term practice that benefits both the organization and patients.
FAQs: Physician Salaries, Career Planning, and Financial Strategy

1. How much do physicians really make, on average?
Average physician salaries vary widely by specialty, region, and practice type. As broad reference ranges:
- Primary care fields often see $220,000–$280,000 early to mid‑career.
- Many non‑surgical subspecialties fall in the $275,000–$400,000 range.
- Surgical and interventional specialties frequently exceed $450,000, with some surpassing $600,000–$700,000 in high‑volume settings.
These figures typically refer to total compensation (base + bonuses). Always consult up‑to‑date specialty‑specific surveys when planning.
2. Is it a mistake to choose a lower‑paying specialty if I have high student debt?
Not necessarily. Many physicians in moderate‑earning specialties manage substantial debt successfully by:
- Choosing lower cost‑of‑living areas or Rural Healthcare positions early on
- Using loan repayment programs (NHSC, PSLF, state programs, employer contributions)
- Maintaining controlled living expenses after training to prioritize debt payoff
- Supplementing income with moonlighting, telehealth, or academic stipends
Aligning your specialty with your interests and strengths is crucial for long‑term career satisfaction. A higher‑earning specialty you dislike can lead to burnout, which ultimately threatens both income and well‑being.
3. How much more can I earn by working in Rural Healthcare compared with an urban center?
Rural and underserved communities often offer:
- Base salaries that are 10–30% higher than urban counterparts for the same specialty
- Signing bonuses that can reach tens of thousands of dollars
- Substantial loan repayment packages over several years
However, these financial benefits must be weighed against lifestyle factors, call burden, proximity to family, and career goals. For some physicians, even a few years in a rural setting can dramatically accelerate wealth building.
4. What parts of a physician contract affect my long‑term income the most?
Key contract elements with major financial implications include:
- Compensation model (guaranteed vs RVU vs hybrid)
- RVU conversion factor and realistic productivity expectations
- Duration of salary guarantees and what happens afterward
- Partnership track details and buy‑in structure in private practice
- Non‑compete clauses, which can limit your options if you need to change jobs
- Tail malpractice coverage responsibility when you leave
Carefully reviewing these items—ideally with professional guidance—can prevent costly surprises.
5. How is the shift to value‑based care likely to affect physician salaries in the future?
As healthcare economics continue to evolve:
- Pure volume‑based fee‑for‑service compensation will likely decline over time.
- Primary care, hospital medicine, and some cognitive subspecialties may benefit as health systems prioritize outcomes, coordination, and population health.
- Procedural volumes will remain important, but documentation, appropriate utilization, and quality metrics will increasingly influence pay.
Physicians who understand quality metrics, care coordination, and health system operations will be well‑positioned to thrive in this environment and secure leadership or incentive‑rich roles.
Understanding the major factors that influence physician salaries—specialty, geographic location, healthcare economics, training, and employment models—allows you to make more strategic decisions at every stage of your career. Balancing financial realities with personal values, clinical interests, and lifestyle priorities is the key to building a sustainable, fulfilling life in medicine.



















