
In today’s rapidly evolving healthcare environment, Health Policy is no longer an abstract concept reserved for legislators and think tanks. It shapes how patients access care, how healthcare professionals practice, how Public Health programs are funded, and how Health Disparities are addressed—or perpetuated.
For medical students, residents, and early-career clinicians, understanding Health Policy and Healthcare Advocacy is now a core professional competency. This practical guide expands on the fundamentals, walks through the policymaking process, and offers actionable strategies to help you engage meaningfully, even with limited time and experience.
Understanding Health Policy: Foundations for Future Clinicians
Health Policy encompasses the decisions, plans, and actions undertaken to achieve specific healthcare and Public Health goals within a society. These policies influence:
- How medical and preventive services are organized and financed
- Who has access to care, and under what conditions
- The quality and safety standards for healthcare delivery
- How Health Disparities are identified and addressed
At its core, Health Policy is about choices: what to fund, whom to prioritize, how to balance individual rights with population health, and how to allocate finite resources fairly and efficiently.
Key Domains of Health Policy
Health Policy touches multiple domains relevant to your future practice:
Access to Care
Policies determine who can obtain Medical Services, under which insurance plans, and at what cost. Examples:- Medicaid eligibility rules
- Telehealth coverage policies
- Network adequacy standards (e.g., distance and wait-time requirements)
Quality and Safety of Care
Policies guide clinical standards, reporting requirements, and quality improvement:- National quality measures (e.g., readmission rates, infection rates)
- Accreditation standards (Joint Commission, NCQA)
- Patient safety regulations (e.g., medication reconciliation, surgical checklists)
Healthcare Costs and Financing
Policies define how care is paid for and how funds flow through the system:- Medicare reimbursement rules
- Value-based purchasing and bundled payments
- Drug pricing and pharmacy benefit management regulations
Public Health Initiatives
Policies structure population-level interventions:- Immunization mandates and school-entry requirements
- Pandemic preparedness and emergency response
- Environmental and occupational health regulations
Workforce and Training
Policies shape how many clinicians are trained, where they practice, and in what settings:- Graduate Medical Education (GME) funding caps
- Licensure and scope-of-practice regulations
- Loan repayment programs for underserved areas
Understanding how these domains interact will help you see how a single policy change can ripple through clinical practice, Public Health, and patient outcomes.
Why Health Policy Matters for Medical Students and Residents
Even if you never set foot in a legislature, Health Policy will influence your daily work, your patients’ lives, and your own career options.
1. Direct Impact on Patient Access and Outcomes
Policies determine whether your patients can afford the medications you prescribe, obtain specialty referrals, or access mental health services. For example:
- Medicaid expansion under the Affordable Care Act (ACA) significantly reduced uninsured rates and improved access to primary care and preventive services.
- Policies that limit coverage for gender-affirming care, reproductive health, or addiction treatment directly shape morbidity, mortality, and Health Disparities.
Clinicians who understand the policy context can better anticipate barriers to care and help patients navigate the system.
2. Equity, Social Justice, and Health Disparities
Health Disparities arise not only from individual factors but also from structural and policy-level decisions. Zoning laws, housing policy, environmental regulation, and school funding all affect health.
Examples of how policy can reduce disparities:
- Expanding Medicaid improves access for low-income populations and communities of color.
- Investing in community health workers can bridge linguistic and cultural gaps.
- Policies promoting transportation access improve appointment adherence for rural and low-income patients.
As a clinician, you’re uniquely positioned to recognize patterns—who is consistently left behind and why—and use that insight to inform equitable Health Policy and Healthcare Advocacy.
3. Shaping the Practice Environment
Health Policy affects:
- Your workload (e.g., documentation requirements, prior authorizations)
- Your income and job options (e.g., reimbursement models, loan repayment programs)
- Your autonomy (e.g., scope-of-practice rules, clinical decision support mandates)
Engaging with policy is partly about protecting your ability to deliver ethical, high-quality care without unnecessary administrative and systemic barriers.
4. Professional Responsibility and Advocacy
Major professional organizations (AMA, ACP, AAFP, APHA, etc.) increasingly emphasize that advocacy is part of medical professionalism. The AMA Code of Medical Ethics and other frameworks explicitly call on clinicians to:
- Advocate for vulnerable populations
- Address systemic contributors to illness
- Support policies that promote Public Health and fairness
Even small-scale advocacy—such as supporting a local public health ordinance or testifying about the effects of a policy on your patients—can have outsized impact.
The Health Policy Process: From Ideas to Implementation
To navigate Health Policy effectively, it helps to understand the lifecycle of a policy: how problems are identified, solutions proposed, laws passed, and programs implemented—and how you can intervene at each stage.
1. Policy Formulation: Identifying Problems and Crafting Solutions
What happens here:
- A problem is recognized (e.g., high maternal mortality rates, rising drug overdose deaths, long ED wait times).
- Stakeholders propose solutions—policy options—based on data, values, and feasibility.
- Draft legislation, regulations, or institutional policies are written.
Who is involved:
- Legislators and their staff
- Government agencies (e.g., HHS, CDC, CMS)
- Professional societies and advocacy groups
- Health system leaders and Public Health departments
- Patients and community organizations
How you can engage:
- Contribute clinical data or case examples that illustrate a problem.
- Participate in institutional committees (e.g., quality improvement, ethics, DEI) that recommend policy changes.
- Provide feedback on draft guidelines or institutional policies circulated for comment.
2. Policy Adoption: From Proposal to Law or Regulation
What happens here:
- Proposed policies move through legislative committees or regulatory comment processes.
- Negotiation, amendment, and coalition-building occur.
- Votes or formal decisions are taken; policies are approved, rejected, or tabled.
Key venues:
- Local councils and boards of health
- State legislatures and regulatory boards
- National bodies (e.g., Congress, federal agencies, judicial rulings)
How you can engage:
- Submit written comments during public comment periods (often underused but highly valued).
- Participate in “lobby days” with professional societies.
- Provide testimony (written or in-person) on how a proposed policy affects patients.
3. Policy Implementation: Translating Law into Practice
What happens here:
- Agencies create rules, programs, and operational guidance.
- Health systems revise clinical workflows and documentation.
- Funding is allocated and programs launch.
Examples:
- A new opioid prescribing law leads hospitals to revise pain management protocols.
- Expanded telehealth coverage prompts clinics to adopt video visit platforms.
How you can engage:
- Participate in quality-improvement (QI) projects that operationalize new policies.
- Help design workflows and education for colleagues and patients.
- Share feedback when implementation is causing unintended harm (e.g., rigid metrics discouraging appropriate care).
4. Policy Evaluation: Measuring Impact and Refining Approaches
What happens here:
- Outcomes are monitored: Does the policy improve health? Reduce costs? Affect equity?
- Data are used to refine, strengthen, or repeal the policy.
How you can engage:
- Collaborate on research projects evaluating policy outcomes (e.g., pre- and post-policy analyses).
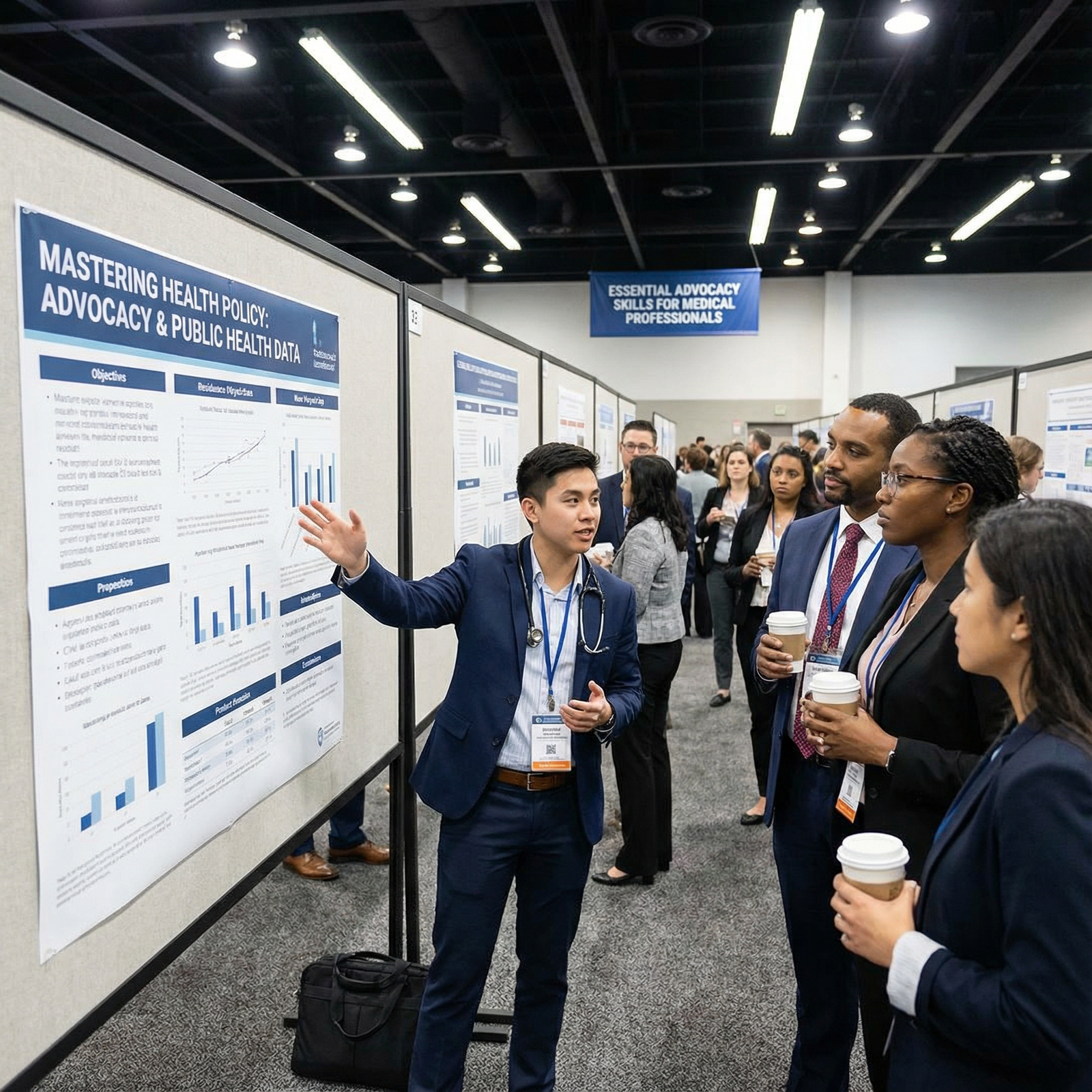
- Present findings at conferences and publish in peer-reviewed journals.
- Use evaluation data in advocacy efforts to support or oppose policy renewal.
Understanding this cycle helps you identify realistic points of entry for involvement, even as a trainee with limited time.
Practical Strategies to Learn and Engage with Health Policy
You do not need a dual MD/MPH or policy fellowship to start engaging. You can build competence and influence incrementally with a structured approach.
1. Build a Strong Knowledge Base
a. Curate high-yield reading and listening
Start with manageable, high-impact sources:
Journals and blogs
- Health Affairs (especially their “Health Affairs Forefront” blog)
- The New England Journal of Medicine Perspective pieces on Health Policy
- JAMA Health Forum
Books for foundational understanding
- The Healing of America by T.R. Reid (global perspective)
- An Introduction to U.S. Health Care Policy by Thomas Rice
- Policy and Politics in Nursing and Health Care (for team-based perspectives)
Podcasts and webinars
- “Tradeoffs” (Health Policy podcast)
- “The Dose” by the Commonwealth Fund
- Webinars by APHA, Kaiser Family Foundation (KFF), and specialty societies
Set a realistic goal: for example, one policy article or podcast per week.
b. Take focused courses
Consider:
- Online courses in Health Policy or Public Health (Coursera, edX, FutureLearn)
- Medical school or residency electives in Health Policy and Healthcare Advocacy
- Certificate programs in Public Health or Health Policy (shorter and more focused than full degrees)
2. Track Relevant Legislation and Regulatory Changes
Understanding what is changing is the first step to influencing it.
Tools and strategies:
Government websites
- Congress.gov for federal legislation
- State legislature websites for local bills
- CMS, CDC, FDA, and HHS for regulatory guidance and Public Health updates
Nonpartisan policy organizations
- KFF (Kaiser Family Foundation)
- Commonwealth Fund
- Center on Budget and Policy Priorities (CBPP)
Professional societies
- Most have policy and advocacy pages summarizing key issues and action alerts (e.g., AMA, ACP, AAFP, AAP).
Set up email alerts or RSS feeds for issues aligned with your interests (e.g., maternal health, mental health, rural care).
3. Engage in Civic and Professional Advocacy
You can scale your advocacy to match your capacity.
Low-barrier actions:
- Sign up for advocacy alerts from your specialty society or APHA.
- Email or call your representatives about a specific bill (use template scripts, then personalize with a clinical story).
- Attend local board of health or city council meetings when health issues are discussed.
Intermediate actions:
- Participate in a “White Coat Day” at your state capitol.
- Write an op-ed or letter to the editor about a Health Policy issue affecting your patients.
- Join your hospital’s government relations or advocacy committee, if available.
Advanced actions:
- Serve on local boards (e.g., school health advisory boards, nonprofit boards).
- Collaborate with community-based organizations on advocacy campaigns.
- Consider formal training programs (e.g., health policy fellowships, academic tracks).
4. Network with Others Working in Health Policy
Policy and advocacy are team sports. Relationships amplify your impact.
Where to connect:
Professional associations
- Join policy committees or sections (e.g., health policy sections of ACP, AMA, APHA).
- Attend advocacy-oriented sessions at conferences.
Academic and clinical institutions
- Seek mentors who publish in Health Policy, sit on guideline panels, or lead Public Health initiatives.
- Join interdisciplinary projects (e.g., social medicine, global health, population health).
Student and resident groups
- American Medical Student Association (AMSA) advocacy projects
- Resident unions or housestaff councils
- Student-run clinics involved in policy and systems-level solutions
Networking not only creates collaboration opportunities but also demystifies pathways into Health Policy roles.
5. Contribute to Research and Quality Improvement with Policy Relevance
Even traditional clinical research and QI projects can have policy implications.
Examples of projects with policy relevance:
- Evaluating the impact of a new prior authorization requirement on treatment delays.
- Studying outcomes before and after a local smoke-free ordinance or syringe services program.
- Analyzing ED utilization trends before and after Medicaid expansion in your state.
Turn your findings into policy influence:
- Include a “policy implications” section in your abstracts and manuscripts.
- Share concise policy briefs with hospital leadership or local Public Health departments.
- Present to community groups and governing bodies to inform decisions.
Real-World Examples: How Effective Health Policy Changes Lives
Understanding concrete successes and failures helps clarify how policy choices play out in practice.
Tobacco Control Policies
Comprehensive tobacco control policies (taxation, advertising restrictions, smoke-free laws, plain packaging, and cessation support) have:
- Reduced smoking prevalence dramatically in many countries
- Lowered rates of lung cancer, cardiovascular disease, and COPD
- Narrowed some Health Disparities, though targeted marketing persists in marginalized communities
Clinicians contributed through research on harms, patient stories, and advocacy for smoke-free environments.
Vaccination and Immunization Policies
Robust vaccination policies—such as school-entry immunization requirements and funded national immunization programs—have:
- Nearly eliminated diseases like polio and measles in many regions
- Reduced morbidity and mortality substantially
- Required ongoing public communication and equity-focused strategies to reach underserved groups
During the COVID-19 pandemic, clinician advocacy and engagement in Public Health communication were central to vaccine rollout.
The Affordable Care Act (ACA)
The ACA is a pivotal example of large-scale Health Policy:
- Expanded insurance coverage for millions through marketplaces and Medicaid expansion
- Protected patients with pre-existing conditions from coverage denial
- Increased access to preventive services without cost-sharing
- Introduced payment reforms to encourage value-based care
However, uneven state adoption of Medicaid expansion has contributed to persistent geographic and racial Health Disparities—underscoring how implementation decisions matter as much as legislative intent.
Policies Addressing the Opioid Epidemic
Responses have included:
- Prescription drug monitoring programs (PDMPs)
- Expanded access to medications for opioid use disorder (MOUD)
- Good Samaritan laws for overdose reporting
- Harm reduction policies such as naloxone distribution and syringe services programs in some regions
Clinician engagement—both advocating for evidence-based treatment and cautioning against overly restrictive measures that harm pain patients—has reshaped these policies over time.

Frequently Asked Questions (FAQ) on Health Policy and Advocacy
1. I’m a busy medical student/resident. How can I realistically get involved in Health Policy?
Start small and integrate policy into what you already do:
- Dedicate 15–20 minutes weekly to a Health Policy article or podcast.
- Join one policy-related group (e.g., your school’s advocacy interest group or a section of your specialty society).
- Participate in a single advocacy action per quarter: email your representative, sign on to a letter, or attend a virtual town hall.
As your schedule allows, you can layer in one time-limited project (e.g., a QI project with policy relevance or a short elective in Public Health or Health Policy).
2. What kinds of careers exist in Health Policy for physicians and other clinicians?
Many paths blend clinical work with policy and Public Health:
- Clinical + academic Health Policy: Split time between patient care, research, and teaching.
- Government roles: Work for federal, state, or local agencies (e.g., CDC, CMS, health departments).
- Health system leadership: Serve as a chief medical officer, quality officer, or population health leader.
- Nonprofit and think tank work: Conduct policy analysis, program design, and advocacy.
- Professional association roles: Guide policy priorities for specialty societies or Public Health organizations.
Training can include MPH or MPP degrees, health policy fellowships, or on-the-job learning through advocacy and committee service.
3. How does understanding Health Policy actually improve my patient care?
Policy awareness helps you:
- Anticipate insurance and access barriers and plan around them.
- Connect patients to relevant benefits (e.g., Medicaid, disability, social services).
- Use existing policy levers (e.g., patient assistance programs, community health resources) to support adherence.
- Recognize when systemic patterns—like repeated denial of a critical service—indicate a policy issue requiring escalation or advocacy.
In many cases, the difference between a theoretical treatment plan and a feasible one is determined by policy.
4. I’m not comfortable with partisan politics. Can I still engage in advocacy?
Yes. Healthcare Advocacy does not require partisan alignment. You can:
- Focus on evidence-based policies that improve health outcomes and equity.
- Emphasize nonpartisan goals such as preventing disease, protecting children’s health, and improving access to high-quality care.
- Work through professional organizations that frame recommendations based on data and consensus rather than party platforms.
Being clear that you are advocating for patients and Public Health, not for a political party, helps maintain professionalism and build trust across diverse audiences.
5. What are some concrete first steps I can take this month?
Here is a simple, actionable starter plan:
- Week 1: Subscribe to one Health Policy newsletter (e.g., Health Affairs, KFF) and skim it once a week.
- Week 2: Attend one virtual or in-person talk/webinar on a Health Policy or Public Health topic.
- Week 3: Identify one policy issue affecting your patients (e.g., prior authorization delays, lack of coverage for a key service) and discuss it with a mentor.
- Week 4: Send a brief, respectful email to a legislator or health system leader describing that issue and one potential solution, grounded in your clinical experience.
Over time, these small actions build your knowledge, confidence, and professional voice in the realm of Health Policy and Healthcare Advocacy.
By steadily expanding your understanding of Health Policy, engaging in targeted Healthcare Advocacy, and collaborating with Public Health and community partners, you can help shape a system that delivers high-quality, equitable Medical Services and reduces Health Disparities. Your clinical insight is not only valuable at the bedside—it is essential in the rooms where policy decisions are made.

















