
Why Rural Medicine Deserves a Serious Look
Rural Medicine offers some of the most meaningful, flexible, and patient-centered healthcare careers available today. For many physicians, especially those early in their careers, rural practice combines:
- Broad clinical scope
- Deep community relationships
- Strong job satisfaction
- Competitive compensation and loan repayment
- Improved work-life balance compared with many urban settings
Yet not all rural environments are the same. Some states have invested heavily in recruiting and supporting rural physicians, offering robust physician opportunities, tailored incentives, and strong community infrastructure.
This guide highlights some of the best states for rural physicians based on job availability, financial and lifestyle benefits, and real-world practice conditions—while also giving you concrete tips on how to evaluate rural offers anywhere in the country.
What Makes a State Attractive for Rural Physicians?
When comparing rural practice options, look beyond the job posting. Consider a structured framework that covers both professional and personal priorities.
Key Factors to Evaluate
1. Physician Opportunities and Job Market
- Number of rural hospitals, critical access hospitals, and FQHCs (Federally Qualified Health Centers)
- Presence of Health Professional Shortage Areas (HPSAs) and Medically Underserved Areas (MUAs)
- Availability of positions in your specialty (especially family medicine, internal medicine, emergency medicine, OB-GYN, general surgery, psychiatry)
- Recruitment patterns: are positions frequently open because of growth, or high turnover?
2. Compensation, Loan Repayment, and Financial Incentives
- Base salary plus productivity bonuses (e.g., RVU-based)
- Sign-on bonuses, relocation assistance, and retention bonuses
- State or federal loan repayment programs (e.g., National Health Service Corps, state-specific programs)
- Rural stipends or hardship pay for particularly remote sites
- Cost of living (housing, childcare, commuting costs)
3. Work-Life Balance and Practice Structure
- Call schedule and backup coverage (especially if you’re the only physician on site)
- Access to specialists and telehealth support
- Staffing levels (nursing, advanced practice providers, ancillary staff)
- Clinic/hospital schedule predictability and vacation policies
- Commuting time and flexibility in scheduling
4. Quality of Life and Community Fit
- Safety, schools, and amenities for you and your family
- Access to outdoor recreation and nature
- Travel access (nearest airport, major highways)
- Cultural, artistic, or faith communities you value
- How welcoming the community is to newcomers and diverse backgrounds
5. Professional Development and Long-Term Growth
- Support for CME, conferences, and board certification maintenance
- Opportunities to teach residents, students, or PAs/NPs (via regional academic affiliations)
- Availability of leadership roles (medical director, CMO, committee leadership)
- Use of telemedicine and digital health tools that expand your clinical reach
When choosing among states—or among rural jobs within the same state—use these factors as a checklist to guide your questions during interviews and site visits.
Top States for Rural Physicians: Opportunities and Lifestyle Advantages
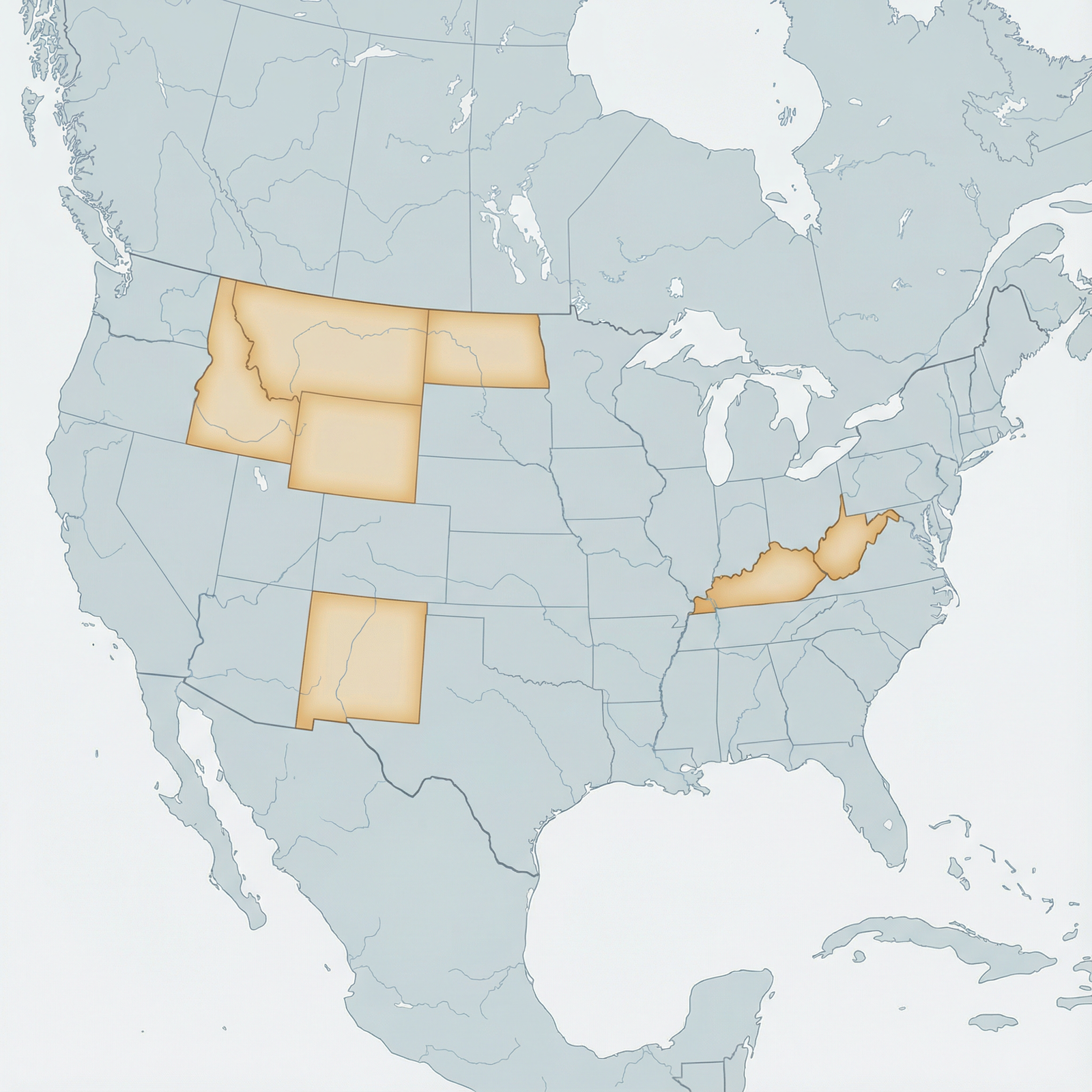
The following states consistently stand out for Rural Medicine due to workforce need, incentive structures, community environments, and physician feedback. They are especially relevant if you’re seeking strong healthcare careers in underserved areas with a favorable work-life balance.
1. Montana: Big Sky, Broad Scope of Practice
Montana’s vast geography and low population density create high demand for rural clinicians. For physicians interested in practicing the full breadth of their training, Montana offers both challenge and reward.
Key Physician Opportunities
- Numerous HPSA and MUA designations provide eligibility for NHSC and state loan repayment
- Need for family medicine, emergency medicine, internal medicine, psychiatry, and OB-GYN in frontier communities
- Positions in critical access hospitals, rural health clinics, and tribal health systems
Compensation and Incentives
- Rural employers often offer:
- Above-average base salaries
- Significant sign-on and relocation bonuses
- Loan repayment or tuition reimbursement packages
- Some facilities negotiate flexible schedules (e.g., block schedules, 7-on/7-off ED coverage)
Lifestyle and Work-Life Balance
- World-class outdoor recreation (hiking, skiing, fly-fishing, camping)
- Short commutes and minimal traffic contribute to a less stressful daily routine
- Smaller schools and tight-knit communities can make family life easier
- Physicians often report high job satisfaction, citing autonomy and meaningful patient relationships
Pro tip: When interviewing, ask specifically about call backup, telemedicine access to specialists, and trauma transfer arrangements given Montana’s long distances between facilities.
2. Wyoming: Low Malpractice, High Reward
Wyoming combines a small population with broad rural need, making it a hot spot for physicians who value autonomy, outdoor adventure, and favorable practice environments.
Practice Environment and Professional Advantages
- Some of the lowest malpractice insurance premiums in the U.S.
- Communities eager to recruit and retain physicians, often offering:
- Rural stipends
- Leadership opportunities
- Flexible schedules and part-time options
- Strong demand for primary care, emergency medicine, general surgery, and anesthesia
Financial and Career Incentives
- Competitive compensation relative to cost of living
- Loan repayment options through state and federal programs
- Many hospitals and clinics are willing to negotiate:
- CME stipends
- Dedicated administrative time
- Coverage for licensure and board fees
Lifestyle and Community
- Easy access to national parks (Yellowstone, Grand Teton), mountains, and wide-open spaces
- Very low population density leads to quiet communities and less congestion
- Physicians often serve as key community leaders—valuable if you enjoy public health and advocacy roles
Consideration: Ask about weather-related transportation (especially winter conditions), and how this impacts transfers, on-call demands, and clinic attendance.
3. North Dakota: Growing Populations, Growing Need
Fueled by energy sector development and an evolving agricultural economy, North Dakota has experienced population shifts that stress existing healthcare systems.
Strong Demand for Rural Physicians
- Many communities qualify as HPSAs, opening doors to loan repayment
- High need for:
- Family medicine
- Internal medicine
- Hospitalists
- Behavioral health providers
- Opportunities to work in integrated systems that serve both urban and rural areas, allowing hybrid practice models
Advantages for Early-Career Physicians
- “Practice-ready” roles with broad procedural experience in rural hospitals
- Supportive communities that frequently integrate physicians into local leadership, school boards, or health committees
- Lower housing costs and cost of living compared with many coastal states
Lifestyle and Wellbeing
- Short commute times and predictable schedules in many practices
- Outdoor activities: hunting, fishing, cross-country skiing, lake recreation
- Strong community identity and family-centered culture, which supports work-life balance
Actionable tip: During site visits, ask current physicians how they maintain professional boundaries in tight-knit communities and how that affects their job satisfaction.
4. Kentucky: Appalachian Commitment and Cultural Richness
Kentucky’s rural and Appalachian regions face significant health disparities, making them ideal places for physicians seeking impact-driven healthcare careers.
Rural Medicine Opportunities
- High need in primary care, addiction medicine, OB-GYN, psychiatry, and general surgery
- Many areas qualify for:
- NHSC loan repayment
- State-based rural incentive programs
- Opportunities for innovative care models addressing:
- Opioid use disorder
- Chronic disease (e.g., diabetes, COPD, cardiovascular disease)
- Maternal health in underserved communities
Financial Packages and Training Pathways
- Rural-focused residency tracks and fellowships that pipeline into Kentucky’s underserved areas
- Enhanced loan repayment, scholarships, and service-commitment contracts for trainees who plan to stay
- Stable salaries with potential productivity bonuses, plus robust benefits in many health systems
Lifestyle and Cultural Environment
- Scenic landscapes, including rolling hills, Appalachian mountains, and rivers
- Vibrant music (bluegrass, country), local festivals, and a strong sense of local heritage
- Cost of living generally below the national average, allowing physicians to build financial security more quickly
If you value: cultural engagement, community-based public health work, and being part of long-term solutions to entrenched disparities, Kentucky can be an especially rewarding choice.
5. New Mexico: Cultural Diversity and Mission-Driven Practice
New Mexico is a standout for physicians who are committed to working with diverse populations and addressing structural health inequities.
Unique Rural and Frontier Needs
- Significant healthcare need among:
- Native American communities
- Rural Hispanic communities
- Remote border regions
- Strong demand in family medicine, internal medicine, pediatrics, psychiatry, and OB-GYN
Incentives and Career Development
- The New Mexico Department of Health and other agencies support:
- Loan repayment for service in HPSAs
- Relocation grants and rural stipends
- Collaborative public health initiatives
- Strong use of telehealth to connect rural clinics with urban specialists and academic centers
Lifestyle and Community Experience
- Distinct blend of Native American, Hispanic, and Anglo cultures
- Renowned arts, cuisine, and festivals (Santa Fe, Albuquerque, and smaller communities)
- Outdoor recreation: hiking, mountain biking, skiing, desert exploration
- Many physicians report deep professional fulfillment from long-term relationships with multigenerational families
Key question to ask: How does the practice support cross-cultural communication (interpreters, cultural liaisons, community health workers) to ensure sustainable, respectful care?
6. Idaho: Expanding Systems, Community-Oriented Practice
Idaho’s fastest-growing population and expanding healthcare networks make it a promising state for physicians seeking rural and semi-rural roles.
Growing Rural Medicine Infrastructure
- Expansion of hospital systems into rural counties
- Increased use of advanced practice providers and telemedicine, with physicians in key supervisory and leadership roles
- Demand for:
- Family medicine
- Emergency medicine
- OB-GYN
- Orthopedics and general surgery
Compensation and Career Flexibility
- Competitive salaries, especially in high-need regions
- Opportunities for mixed practice:
- Outpatient + inpatient
- Clinic + ED coverage
- Part-time or flexible scheduling for physicians prioritizing work-life balance
- Many employers provide strong CME support and mentorship for new graduates
Idaho Lifestyle and Wellbeing
- Mountains, rivers, and forests ideal for skiing, rafting, hiking, and camping
- Growing but still manageable urban centers (Boise, Idaho Falls) with access to cultural amenities, while living in nearby rural communities
- Sense of safety and community that appeals to many families
7. West Virginia: Rural Health Innovation in Mountain Communities
West Virginia faces some of the greatest health challenges in the nation—making it a place where motivated physicians can make a visible, measurable difference.
High-Impact Physician Opportunities
- Significant need in:
- Primary care
- Addiction medicine and psychiatry
- Pulmonary and cardiology consultative services
- OB-GYN and women’s health
- Many communities with HPSA designations and strong eligibility for loan repayment
- Active efforts to improve rural infrastructure, telehealth, and chronic disease management
Incentives and Support Programs
- Strategic rural health programs that:
- Offer financial incentives for service commitments
- Support rural residencies and training tracks
- Foster collaborations between academic centers and critical access hospitals
- Potential to engage in research, quality improvement, and population health projects even in small communities
Lifestyle, Nature, and Community
- Scenic mountains, rivers, and state parks with outstanding hiking, whitewater rafting, and mountain biking
- Tight-knit communities where physicians are highly valued and often know their patients for decades
- Strong community engagement, with many opportunities to participate in school health, local events, and public health initiatives
Important to clarify: Ask how the practice helps manage burnout risk in high-need populations (team-based care, behavioral health integration, realistic panel sizes).
Beyond Geography: The Rural Lifestyle and Day-to-Day Experience
Regardless of state, the Rural Medicine lifestyle has consistent themes that may be exactly what you’re looking for—or may not fit your personal goals. It’s essential to be realistic and introspective.
Core Lifestyle Advantages
- Close-knit communities: You’ll often care for multiple generations of the same families, creating meaningful continuity and high job satisfaction.
- Less congestion, slower pace: Short commutes and quieter towns reduce daily stress.
- Time for family and hobbies: Compared with some high-intensity urban roles, rural schedules can be more predictable, especially in outpatient-focused roles.
- Community recognition and impact: Your work is highly visible, and your presence often transforms access to care for an entire region.
Common Challenges to Consider
- Professional isolation: Fewer local colleagues or on-site specialists; you’ll rely more on phone consults and telehealth.
- Resource limitations: Smaller hospitals and clinics with fewer diagnostic tools or subspecialty services on site.
- Blurred boundaries: Patients may be neighbors, teachers, or community leaders; maintaining professionalism while staying engaged takes intentionality.
- Travel for personal needs: You may have to drive longer distances for certain amenities, shopping, or specialized medical care for your own family.
Strategies to Maximize Satisfaction in Rural Practice
- Negotiate clear expectations for call coverage, clinic volume, and administrative tasks.
- Confirm access to telemedicine and specialist backup, especially for high-acuity cases.
- Build a professional network through state medical societies, rural health associations, and alumni networks.
- Invest early in community relationships—schools, civic organizations, local public health—if you plan to stay long-term.

Frequently Asked Questions About Working as a Rural Physician
1. Which specialties are most in demand in Rural Medicine?
Rural areas consistently need:
- Family Medicine and Internal Medicine (including hospitalist roles): backbone of primary care and inpatient care
- Emergency Medicine: especially in critical access hospitals and small EDs
- OB-GYN and Women’s Health: due to maternity care deserts in many rural regions
- Psychiatry and Behavioral Health: including addiction medicine and integrated primary care behavioral health
- General Surgery and Anesthesia: for basic surgical services and trauma stabilization
If you’re in a subspecialty, consider hybrid roles (e.g., general internal medicine with a focus area) or telehealth-supported models.
2. How can I find rural physician opportunities in these states?
Use multiple strategies:
- National job boards with rural filters (e.g., AAFP, ACP, ACOEP, NEJM CareerCenter)
- State medical society websites and rural health associations
- National Health Service Corps (NHSC) job board listing approved HPSA sites
- Contact rural residency programs and ask about alumni destinations
- Work with recruiters, but clarify your requirements (e.g., loan repayment, call expectations, location preferences) early
When you identify a position, request a site visit to experience the community and speak directly with current physicians and staff.
3. Are there robust educational and professional development resources for rural physicians?
Yes. While you may be physically distant from academic centers, many states and health systems invest heavily in rural support:
- Tele-education networks (e.g., Project ECHO) for case-based learning
- Virtual CME programs and online conferences
- Regional academic affiliations that allow you to precept students and residents
- Rural-focused leadership programs and quality-improvement collaboratives
When evaluating a job, ask how the organization supports CME, mentorship, and leadership development for rural clinicians.
4. Does working in a rural area mean I’ll earn less?
Not necessarily—and often the opposite is true. In many of the states highlighted:
- Base salaries are competitive or higher than urban counterparts due to recruitment needs.
- Loan repayment (federal and state) can substantially boost your effective compensation.
- Cost of living is usually lower, so your income stretches further.
- Incentives such as sign-on bonuses, rural stipends, and relocation support are common.
To accurately compare offers, consider total compensation (salary + bonuses + loan repayment + benefits) against local cost of living and your expected schedule.
5. What should I ask during interviews for rural physician positions?
Focus on questions that clarify both clinical realities and lifestyle impact, such as:
- What is the typical patient panel size and daily visit volume?
- How is call shared, and who provides backup?
- What procedures and services are expected from my specialty in this setting?
- How are complex or high-acuity cases transferred, and to which facilities?
- What telehealth or specialty support is available after hours?
- How long have current physicians stayed, and why did previous physicians leave?
- How does the organization support physician wellness and prevent burnout?
These questions help you gauge the true work-life balance, sustainability, and culture of the practice.
Conclusion: Choosing the Right Rural Path for Your Career
States like Montana, Wyoming, North Dakota, Kentucky, New Mexico, Idaho, and West Virginia offer some of the strongest environments for Rural Medicine in the U.S.—combining:
- Abundant physician opportunities
- Competitive financial packages and loan repayment
- Supportive communities and meaningful patient relationships
- Enhanced work-life balance and high job satisfaction
For residents and early-career physicians, these locations can accelerate growth, expand clinical skills, and provide leadership experiences that are harder to access in large urban centers.
As you explore rural healthcare careers, approach each potential position with a structured framework: analyze compensation, call structure, community fit, professional development, and lifestyle alignment. Visit in person, talk with current clinicians, and be honest with yourself about the environment in which you will thrive.
If you value impact, community, and a more balanced way of practicing medicine, Rural Medicine in the right state may offer precisely the career—and life—you’re looking for.




















