
Understanding the Fellowship Landscape for Caribbean IMGs in Pathology
Caribbean medical school graduates are increasingly represented in pathology residency programs across the United States, including those who come from schools like SGU, AUC, Ross, and others. Many of these residents are already thinking well ahead about how to get fellowship positions in competitive subspecialties such as dermatopathology, hematopathology, GI pathology, cytopathology, and others.
As a Caribbean IMG in pathology, you may feel you have to “over‑prove” yourself compared with US MD graduates. That’s a realistic assessment—but it’s also an opportunity. The same habits and strategies that help you overcome the Caribbean IMG label are exactly what will make you a strong fellowship candidate in any program.
This article focuses on:
- How the fellowship application timeline really works in pathology
- What to do each year of residency to build a strong profile
- How to leverage your Caribbean background strategically
- How to stand out for competitive pathology fellowships
- Practical steps for preparing for fellowship while thriving in residency
Throughout, we’ll keep the specific perspective of a Caribbean medical school residency graduate in mind, drawing from the real dynamics you’re likely to face.
How Pathology Fellowships Work: Timeline, Competitiveness, and Realities
Understanding the structure of the fellowship market is the foundation of smart preparation. Pathology is unique among specialties: most residents pursue at least one fellowship, and many do two.
Types of Pathology Fellowships
Common fellowships include:
- Surgical Pathology (general or subspecialty-focused)
- Cytopathology
- Hematopathology
- Dermatopathology
- Gastrointestinal (GI)/Liver Pathology
- Breast, GYN, GU, Thoracic, Renal, Bone/Soft Tissue Pathology
- Molecular Genetic Pathology
- Transfusion Medicine/Blood Banking
- Forensic Pathology
- Informatics or Quality/Management (growing niches)
Some are highly competitive for everyone (Dermpath, Hemepath, GI, Molecular). Others are relatively more accessible but still require a strong application.
The Fellowship Application Timeline in Pathology
In pathology, the fellowship application timeline has traditionally been very early and somewhat chaotic, with many programs previously filling positions out of sync. There has been movement toward a more standardized schedule, but you must check up-to-date information through:
- Program websites
- Fellowship directories (e.g., Association of Pathology Chairs, specialty societies)
- Your program director and faculty mentors
As of recent trends (always verify current cycles):
- Applications often start in PGY‑2 or early PGY‑3 for fellowships that begin after PGY‑4.
- Many competitive fellowships interview and offer positions more than 18–24 months before the start date.
- Some fellowships (e.g., Forensic, certain community programs) may still accept applications somewhat later, but you should assume it’s early unless proven otherwise.
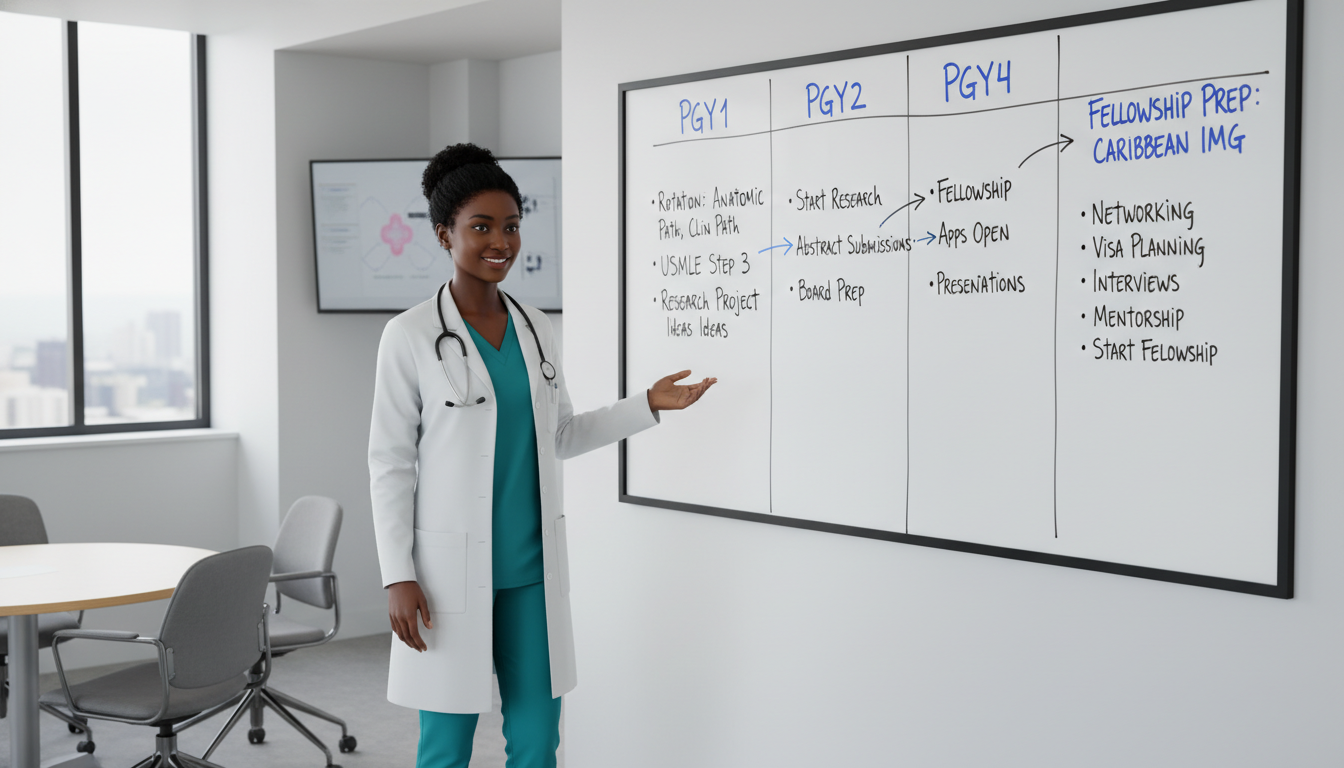
For a 4-year AP/CP resident, a typical pattern might be:
- PGY‑1: Explore subspecialties, build baseline performance, start small projects
- Early–mid PGY‑2: Decide target fellowship(s), strengthen research and letters
- Late PGY‑2 to early PGY‑3: Submit fellowship applications, attend interviews
- Mid–late PGY‑3: Secure fellowship spot(s), continue building expertise
- PGY‑4: Finalize skills, aim for leadership roles, consider second fellowship if desired
Because you’re a Caribbean IMG, you should assume you’ll need to be better prepared and slightly earlier than your peers to be maximally competitive.
Year-by-Year Strategy: What to Do in Each Stage of Residency
PGY‑1: Build Your Foundation and Reputation
Your first year is about credibility. As a Caribbean IMG, much of the unspoken question is: “Can you perform at the level of—or above—US grads?” Your answer is your daily work.
Goals in PGY‑1:
Master the basics of AP and CP workflows
- Be reliable with grossing, sign-out preparation, and lab medicine tasks.
- Ask structured questions; show that you’re learning efficiently, not randomly.
Establish professionalism and work ethic
- Be on time, responsive, and prepared at sign-out.
- If you’re less experienced in US systems, reflect that you’re “green but rapidly improving,” not “clueless.”
Identify early mentors
- Pay attention to faculty who:
- Enjoy teaching
- Are active in your potential subspecialty interests
- Are respected in the department
- Ask for advice early: “I’m interested in preparing for fellowship in hematopathology; how can I best use my PGY‑1 year?”
- Pay attention to faculty who:
Start low-risk scholarly activities
- Case reports, image-based teaching files, QA projects, or co-authoring a review.
- Even one or two small projects in PGY‑1 sets a tone of academic engagement.
Understand your relative strengths/weaknesses as a Caribbean IMG
- Are your test-taking skills strong? That will help on boards and ITE.
- Do you need support in scientific writing, statistics, or lab medicine? Seek it now.
Actionable tips:
Keep a “fellowship preparation” notebook (digital or paper) where you log:
- Rotations you enjoyed (and why)
- Faculty who gave you strong feedback
- Skills you want to improve
- Ideas for projects related to your target subspecialty
Ask at least one trusted faculty member by the end of PGY‑1:
- “From what you’ve seen so far, which areas should I focus on to be competitive for [subspecialty] fellowship?”
PGY‑2: Clarify Your Path and Build a Niche
PGY‑2 is when fellowship strategy becomes real. You should be moving from “I like pathology generally” to “I’m likely to apply for [1–2 subspecialties].”
Key decisions in PGY‑2:
Choose your target fellowship(s) thoughtfully Consider:
- Your genuine interest: Can you see yourself reading these cases daily for decades?
- Job market: Some subspecialties (like GI, breast, GU) are attractive to private groups; others (e.g., molecular) may be tied to academic centers.
- Competitiveness: If you want dermatopathology, hemepath, or GI, you must plan especially early and aggressively.
Align your rotations and electives
- Request extra time in your intended field (e.g., additional hemepath at a tertiary center).
- If your home program is weak in your area of interest, consider away electives (with PD approval).
Strengthen your academic profile
- Aim for 1–3 concrete scholarly outputs this year:
- Case series, retrospective chart review, quality improvement project.
- Posters at national or regional meetings (USCAP, CAP, ASCP, subspecialty societies).
- If possible, target at least one project where you’re first author.
- Aim for 1–3 concrete scholarly outputs this year:
Develop early leadership or teaching involvement
- Help teach medical students on pathology rotations.
- Be the “go-to” resident for digital slide sets, boards review sessions, or resident teaching conferences.
Monitor your in-service exam (ITE) and board prep
- Strong exam performance backs your application, especially as a Caribbean IMG.
- If your scores are borderline, discuss a structured remediation/study plan with your PD early.
By the end of PGY‑2, you should have:
- A clear primary fellowship goal (e.g., cytopathology, hemepath, GI) and one backup plan.
- At least one mentor in your chosen subspecialty who knows you well.
- CV entries that show a trajectory: “Serious, academically engaged, and improving.”
PGY‑3: Application Season and Visibility
For most residents, PGY‑3 is when the pathology match for fellowships—informal as it may be—really happens.
Major tasks in PGY‑3:
Finalize your fellowship targets and list of programs
- Create a spreadsheet of:
- Programs you’re interested in
- Requirements (US citizenship/visa, prior AP/CP rotation, research, etc.)
- Application deadlines and specific instructions
- Include both reach and safety programs, especially as a Caribbean IMG.
- Create a spreadsheet of:
Fine-tune your CV and personal statement
- Highlight:
- Pathology-specific strengths (independence at sign-out, strong grossing, CP knowledge).
- Your subspecialty experiences and any related research.
- Professional growth since starting residency, especially if your Caribbean background required adaptation.
- Avoid over-explaining your Caribbean medical school; instead, frame it as:
- Evidence of resilience and adaptability
- A source of clinical breadth and patient diversity exposure
- Highlight:
Secure strong letters of recommendation
- At minimum, you typically want:
- Letter from your Program Director
- Letter from a key subspecialty mentor in your chosen field
- Possibly an additional letter from another faculty member who knows your work well
- Ask early, and provide:
- Updated CV
- Draft personal statement
- Summary of rotations/projects you did with them
- At minimum, you typically want:
Apply early and broadly
- For competitive fellowships, apply as soon as the cycle opens.
- Submit to more programs than your US MD peers might—this is part of the reality as a Caribbean IMG.
- Make sure visa status (if relevant) is clear and correctly documented.
Prepare intentionally for interviews
- Be ready to explain:
- Why this subspecialty
- Why this specific program
- How your background (including Caribbean medical school residency training) adds value
- Come with informed questions:
- “What kind of case mix and volume will fellows see?”
- “How are fellows prepared for academic vs private practice careers?”
- “What are your recent graduates doing now?”
- Be ready to explain:
During PGY‑3, you’re not just applying; you’re also auditioning daily in your own department. Many residents secure fellowship offers within their own institution partly through consistent local performance.
PGY‑4: Consolidate Skills and Think Beyond Fellowship
Once you’ve secured a fellowship position, PGY‑4 is about finishing strong and preparing for the next phase:
- Achieve higher independence in sign-out and lab management.
- Continue scholarly work that you can carry into fellowship.
- If considering a second fellowship, start researching options and timelines early in PGY‑4.
- Prepare intensively for board exams, as passing on the first attempt strengthens your credibility going into fellowship and job search.
Strengthening Your Application as a Caribbean IMG

Being a Caribbean IMG can be perceived differently by programs. Your goal is not to “hide” your background, but to demonstrate clearly that any initial doubts are unfounded.
Academic and Clinical Excellence Are Non-Negotiable
Consistently strong evaluations
- Avoid “mixed” narratives in your performance reviews. Work with your chief residents and PD to address weaknesses early.
Evidence of progression
- Programs want to see growth: “Resident X started with moderate diagnostic ability and is now excellent and independent.”
- Ask faculty for concrete feedback and act on it.
Board and in-service exam performance
- High scores help offset biases about training background.
- If you’ve historically struggled with standardized exams (step scores, etc.), get support early—tutoring, study groups, structured plans.
Strategic Research and Scholarly Work
You don’t need dozens of publications to enter a good fellowship, but you do need quality and relevance:
Aim for subspecialty-aligned projects.
- Want hemepath? Work on lymphoid or myeloid neoplasm studies, flow cytometry QA, or marrow correlation projects.
- Want GI? Participate in colon polyp research, inflammatory bowel disease pathology, or liver biopsy studies.
Prioritize projects likely to finish before applications go out.
- A completed poster and submitted manuscript carry more weight than multiple vague “works in progress.”
Present at national meetings.
- USCAP, CAP, ASCP, and subspecialty meetings are powerful for:
- Networking
- Showing initiative
- Gaining visibility outside your home program
- USCAP, CAP, ASCP, and subspecialty meetings are powerful for:
When people ask later “how to get fellowship in a competitive pathology subspecialty as a Caribbean IMG,” your answer should be: “I used my residency years strategically and consistently.”
Networking and Visibility
For Caribbean IMGs, networking is a major multiplier:
Within your home institution
- Attend departmental conferences even when not on that rotation.
- Volunteer to present unknown cases or journal club.
- Offer to help with teaching archives or digital slide sets.
Outside your institution
- Introduce yourself to faculty at conferences from potential fellowship programs.
- Join professional societies (e.g., USCAP, CAP) and subspecialty organizations (e.g., hematopathology or dermpath societies).
- Reach out respectfully to fellowship directors:
- Brief email, attach CV
- Express specific interest (not generic)
- Ask if they anticipate openings for your cycle and whether they accept applications from Caribbean IMGs/visa-holders if relevant.
Networking is not about begging for positions; it’s about allowing programs to see your seriousness, preparation, and personality ahead of application review.
Addressing the Caribbean Background Without Overemphasis
In your personal statement and interviews:
- Do not apologize for attending a Caribbean medical school.
- Instead, highlight:
- Resilience in adapting to new environments and systems
- Exposure to broad clinical conditions and diverse patient populations
- Your deliberate choice to pursue pathology despite an initial route that often leads to other clinical specialties
You want the narrative to be:
“Yes, I’m a Caribbean IMG, but more importantly, I’m a high-performing, motivated pathology resident with clear subspecialty commitment and a track record of productivity.”
Planning Beyond Fellowship: Career Direction and Second Fellowships
When preparing for fellowship, you must also think about what comes after. Your end goal—community practice vs academic career—will shape important choices.
Clarify Your Career Vision Early
Ask yourself:
Do I see myself in academic pathology?
- Teaching residents and students
- Conducting research
- Presenting at conferences, writing regularly
Or do I prefer high-volume private practice or hybrid models?
- Broader case mix
- Possibly more emphasis on surgical pathology and CP skills
- Less protected research time
Your answer guides:
- Which fellowships you pursue (e.g., molecular pathology often aligns with academics; breast or GI may align well with community groups).
- How deeply you invest in research vs operational/quality improvement projects.
When to Consider a Second Fellowship
Many pathologists pursue two fellowships, especially when:
Combining surgical subspecialty + a high-value field
- Example: GI pathology + cytopathology
- Example: Hemepath + molecular pathology
Strengthening overall marketability for private practice
- Example: General surgical pathology + transfusion medicine
When thinking about how to get fellowship positions for a second year, the process mirrors the first, but with advantages:
- You have more specialized references.
- You have more mature scholarly work.
- Fellowship directors may value your added expertise.
However, beware of:
- Extending training unnecessarily if it doesn’t align with realistic job goals.
- Piling fellowships just to delay employment, which programs may interpret negatively.
Practical Steps in “Preparing for Fellowship” and Beyond
During residency:
- Keep an updated CV and document all teaching, research, and departmental contributions.
- Save de-identified interesting cases for future teaching and presentations (per institutional policies).
During fellowship:
- Focus on building depth in your subspecialty.
- Seek chances to write reviews or book chapters with your fellowship attendings.
- Attend job fairs or networking receptions at national meetings.
Approaching the job search:
- Use mentors to understand:
- Which kinds of groups are hiring
- What a realistic first job looks like with your training
- Tailor your job applications: highlight how your fellowship(s) and Caribbean medical school residency experience have developed your resilience, adaptability, and ability to work in diverse systems.
- Use mentors to understand:
Common Pitfalls and How to Avoid Them
Even strong residents make mistakes that weaken their fellowship prospects. Watch for:
1. Waiting Too Long to Engage With Mentors
If you wait until late PGY‑3 to tell faculty what you’re interested in, you lose precious time:
- They can’t easily involve you in projects that would have helped your application.
- They may not know you well enough to write truly strong letters.
Solution: Start these conversations by mid‑PGY‑2 at the latest.
2. Unfocused Applications
Applying to every fellowship type in existence signals lack of clarity.
Solution: Identify 1–2 primary interests and 1 reasonable backup. Apply accordingly and be able to articulate why.
3. Neglecting CP or General Skills
Some residents become hyper-focused on a subspecialty (e.g., dermpath) and neglect general AP/CP skills, which can harm both fellowship and future job performance.
Solution: Even while targeting a niche, continue to excel on general services. Most programs still value well-rounded pathologists.
4. Underestimating Visa and Licensing Issues
If you require a visa:
- Some fellowships don’t sponsor visas.
- Delays in prep for licensing exams and ECFMG paperwork can cause problems.
Solution: Clarify your visa status early with your GME office and target programs known to sponsor your visa category.
5. Poor Communication or Professionalism
As a Caribbean IMG, you are often under closer scrutiny for professionalism and communication style:
- Email etiquette, timeliness, and follow-through matter.
- How you handle stress on busy services will be remembered.
Solution: Seek early feedback on your communication style and professionalism, and adjust proactively.
FAQs: Fellowship Preparation for Caribbean IMGs in Pathology
1. As a Caribbean IMG, do I have to do a fellowship to get a job in pathology?
Realistically, yes in most settings. While a few positions might hire straight from AP/CP residency, the norm in current practice—especially for a Caribbean medical school residency graduate—is to complete at least one fellowship, often in a high-value area such as surgical pathology, cytopathology, or hemepath. Fellowship training makes you more competitive, especially against US grads.
2. How many research projects do I need to match into a competitive pathology fellowship?
There is no strict number, but as a guideline:
- 1–3 meaningful projects (with at least one where you’re first author) is usually sufficient if they are high quality and relevant to your subspecialty.
- Presentations at national meetings, particularly in your desired area, carry significant weight.
- Fellowship directors value depth and follow-through more than sheer quantity.
3. Can I match into top-tier fellowships (e.g., dermpath, hemepath at major academic centers) as a Caribbean IMG?
Yes, it’s possible—but you must be exceptionally prepared:
- Strong clinical performance and clear subspecialty commitment
- Robust letters from respected faculty
- Subspecialty-focused research or presentations
- Competitive board/ITE scores
- Professionalism and maturity in interviews
Programs may initially hesitate because of your Caribbean background, but a strong, coherent record can override that hesitation.
4. When should I start my fellowship application if I want to do GI or hemepath?
Assuming a traditional 4-year AP/CP program:
- Start serious planning and mentor discussions by mid‑PGY‑2.
- Begin preparing your CV, personal statement, and program list in late PGY‑2.
- Be ready to submit applications early in PGY‑3, or as soon as your target programs open their cycle (sometimes even late PGY‑2, depending on the year).
- Always confirm the current fellowship application timeline on each program’s website and with your PD, as policies can change.
By approaching residency with a clear plan, strategically leveraging your experiences as a Caribbean IMG, and understanding the nuances of the pathology fellowship landscape, you can position yourself competitively for the pathology match and beyond. Your background does not define your ceiling; it simply shapes the path you must walk—deliberately, consistently, and with a long-term view of your career in pathology.




















