
Neurology is one of the most rapidly evolving fields in medicine, and subspecialty training is increasingly essential for DO graduates who want to build a robust, flexible career. Whether your goal is epilepsy, stroke, neuromuscular medicine, movement disorders, neurocritical care, or another subspecialty, thoughtful fellowship preparation during residency can dramatically expand your options.
As a DO graduate in neurology, you bring unique strengths—holistic training, strong communication skills, and a patient-centered approach—but you also face specific questions: How will osteopathic training be viewed? Does your path differ from MD applicants? What’s the realistic fellowship application timeline? And practically, how do you get from residency to your ideal neuro fellowship?
This guide walks through the process step-by-step, from intern year to submitting your applications, with a focus on neurology and the realities of being a DO graduate residency trainee.
Understanding the Fellowship Landscape for Neurology DO Graduates
Why Neurology Fellowship Matters More Than Ever
Modern neurology practice increasingly favors subspecialization. Many academic and even community positions now expect—or strongly prefer—fellowship training. Subspecialty fellowship can:
- Deepen your expertise in a focused area (e.g., epilepsy, stroke, neuroimmunology)
- Increase your competitiveness for academic positions and research roles
- Open doors to niche clinical practices (e.g., botulinum toxin clinics, EMG labs, neuro-oncology programs)
- Enhance earning potential and negotiation power
- Position you for leadership roles and program development
For DO graduates, subspecialty training can also help neutralize any lingering bias from program directors who are less familiar with osteopathic training pathways. A strong fellowship and robust CV make “DO vs MD” less relevant over time.
Common Neurology Fellowships to Know
You don’t need to commit early, but you should understand the major neurology fellowship categories so you can target your early experiences. Popular options include:
- Vascular Neurology (Stroke)
- Epilepsy / Clinical Neurophysiology
- Neurocritical Care
- Movement Disorders
- Neuromuscular Medicine / EMG
- Multiple Sclerosis / Neuroimmunology
- Headache Medicine
- Behavioral Neurology / Dementia
- Neuro-oncology
- Interventional Neurology / Endovascular Surgical Neuroradiology (variable routes)
- Pain Medicine (often via anesthesia/PM&R but open to neurology)
- Autonomic Disorders
- Neurohospitalist (often not formal ACGME, but some structured programs exist)
Each has its own competitiveness level, structure (1 vs 2 years), and mix of clinical, procedural, and research focus. Early in residency, let curiosity drive you: read widely, talk to faculty, and watch where your interest naturally deepens.
DO Graduate Residency Background: How It Impacts Fellowship
The days of a separate “osteopathic residency match” are gone—neurology residencies now fall under a single accreditation system (ACGME), but your DO background still shapes your path:
Advantages of being a DO graduate:
- Strong training in physical exam skills and patient communication
- Holistic approach that fits well in chronic neurologic care
- Many DO graduates have broad community and inpatient exposure—valuable for vascular, neurocritical care, and general neurology fellowships
Potential challenges:
- Some highly academic programs may historically have fewer DO graduates, meaning you may have to be more proactive in demonstrating your research and scholarly potential
- If your neurology residency has lower name recognition, you may need extra effort in networking, letters of recommendation, and research output
The good news: neurology as a specialty is relatively DO-friendly, and many programs have DO faculty or prior DO fellows. The key is to build a CV and application that clearly demonstrates excellence, regardless of degree.
Year-by-Year Fellowship Preparation Roadmap During Neurology Residency
Your best chance of success comes from turning fellowship preparation into a structured, multi-year process—not a last-minute scramble in PGY-4.
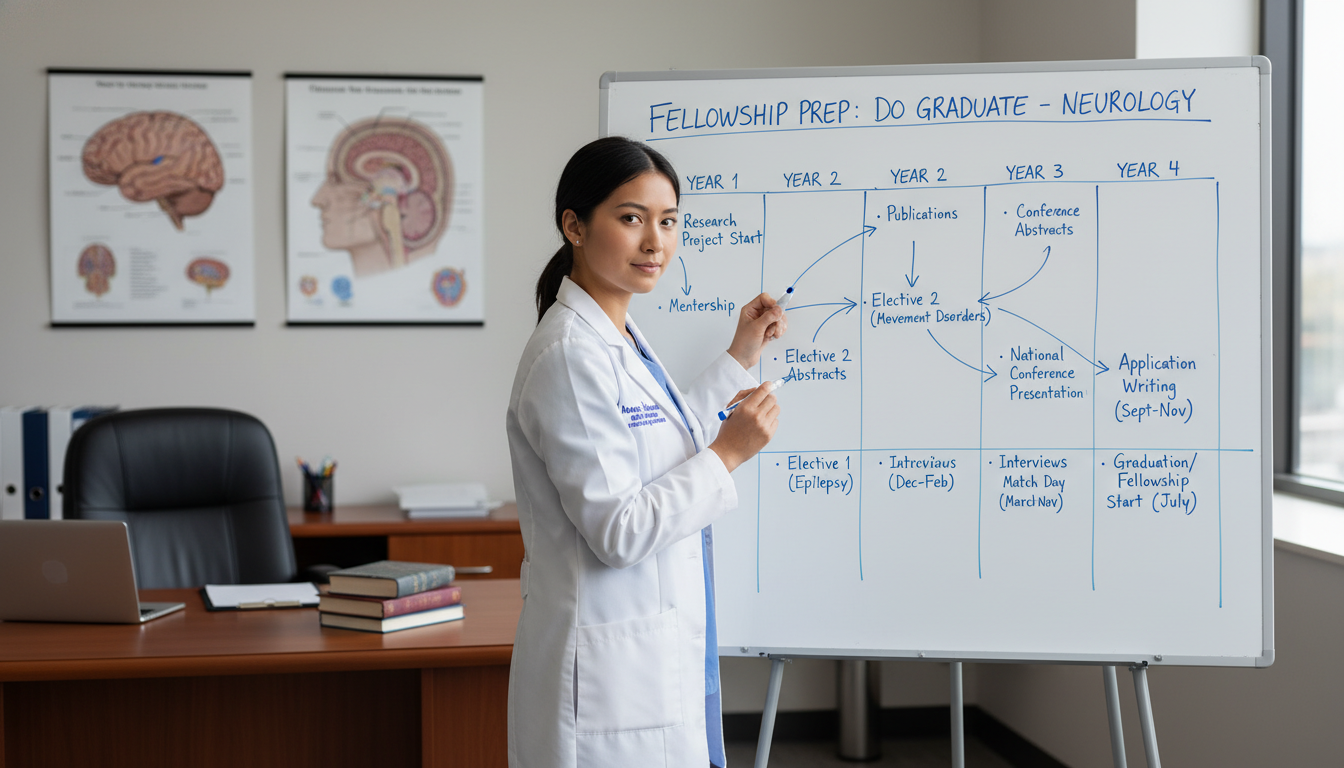
PGY-1 (Intern Year): Laying the Foundation
Whether you’re in a transitional year, internal medicine prelim, or categorical neurology program, intern year is about building habits and situational awareness.
Key objectives:
Understand the fellowship landscape
- Talk with senior residents and fellows about what fellowships exist and what they actually do day-to-day.
- Attend neurology grand rounds even when rotating off-service if possible.
- Identify 2–3 subspecialties that genuinely interest you (e.g., epilepsy, stroke, movement disorders) without locking yourself in.
Start networking lightly
- Introduce yourself to subspecialty attendings on your neurology months.
- Let them know you’re curious about their field and would like to shadow or work on a project later.
- Ask current fellows informal questions: “What would you do differently in residency to prepare?”
Reset your study habits
- Prepare for neurology residency by building a strong general medicine base—this matters for neurocritical care, vascular, and general neurology.
- Use your intern year to create a sustainable reading routine: brief daily reading on cases you see, plus a weekly deeper dive.
Documentation and professionalism
- Many fellowship directors explicitly look for “safe,” reliable, professional residents.
- Build a reputation early as someone who:
- Is dependable and shows up prepared
- Communicates clearly with nurses, consultants, and patients
- Handles feedback constructively
Your main task in PGY-1 isn’t to publish multiple papers; it’s to become a strong clinician-in-training and to start observing which aspects of neurology energize you.
PGY-2: Clarifying Interests and Building a Fellowship-Friendly Profile
PGY-2 is often the busiest year clinically—but it’s also when you start truly signaling your subspecialty interests.
1. Clarify your subspecialty direction
As you rotate through different neurology services, ask:
- Which patients do you look forward to seeing?
- Are you drawn more to acute, high-acuity care (stroke, neurocritical care) or longitudinal, outpatient care (movement, MS, epilepsy, headache)?
- Do you enjoy procedures/technical work (EMG, EEG, LPs, Botox, interventions)?
By mid-to-late PGY-2, try to narrow down to 1–2 subspecialties you’d be happy pursuing.
2. Start or join research projects
For many neurology fellowships—especially academic ones—some research experience is expected.
- Ask attendings in your area of interest:
“I’m a PGY-2 interested in [subspecialty]. Are there any ongoing projects I could help with, even in a small way?” - Look for:
- Case reports and case series
- Retrospective chart reviews (e.g., stroke outcomes, epilepsy surgery series)
- Quality improvement (QI) projects
- Aim initially for “doable wins”:
- One case report or poster in PGY-2
- A role in a larger project, even if it won’t finish until PGY-3
As a DO graduate, building a research track record helps strengthen your fellowship application, especially at highly academic programs.
3. Attend conferences if possible
- Regional or national meetings (e.g., AAN, subspecialty society meetings) offer exposure and networking.
- Presenting a poster—even a small project—helps:
- Demonstrate scholarly activity
- Put you face-to-face with potential fellowship mentors at other institutions
If funding is tight, ask your program about:
- GME travel funds
- Departmental support
- Student/resident scholarship opportunities through neurology societies
4. Study plan and in-training exams
Consistent performance on in-training exams is increasingly important. While there’s no formal “neuro match score,” program directors do review your in-training performance.
- Make a realistic schedule: e.g., 20–30 minutes of reading most days, plus more focused time pre-exam.
- Use core texts and question banks recommended by your senior residents.
A strong exam record reassures fellowship programs that you will pass boards and handle the cognitive load of subspecialty training.
PGY-3: Execution Phase – Positioning for the Neuro Match
PGY-3 is critical. This is when much of your visible fellowship preparation happens.
1. Solidify your subspecialty choice by early PGY-3
Ask yourself:
- Can I see myself practicing this area for decades?
- Am I interested enough to read about it on off days?
- Do I have or can I develop at least one mentor in this field?
If you’re truly torn between two areas (e.g., epilepsy vs neurocritical care), talk this through with multiple mentors. It’s still possible to strategically apply to more than one type of fellowship, but your story should remain coherent.
2. Plan targeted electives
Use elective time to:
- Spend dedicated weeks on your subspecialty (e.g., epilepsy monitoring unit, neuromuscular clinic, MS center)
- Explore potential fellowship sites if your program allows away electives (some do during PGY-3)
- Demonstrate commitment and build relationships with faculty who could eventually write letters
If an away rotation isn’t logistically possible:
- Consider a “virtual away” via telehealth clinics, remote case conferences, or joint research projects—many programs remain open to these models after the pandemic era.
3. Strengthen your CV in a focused way
To prepare for fellowship, your CV should demonstrate:
- Clinical excellence
- Genuine engagement with your chosen subspecialty
- Some form of scholarship or academic activity
Concrete targets for PGY-3:
- At least one poster or abstract accepted (regional or national)
- Ongoing involvement in a larger project (even if results aren’t submitted yet)
- Participation in teaching (medical students, junior residents, or community education)
If you’re aiming for a highly competitive niche (e.g., neuroimmunology at a top academic center), more research will help. If you’re aiming for a solid clinical fellowship at a mid-sized program, a moderate but consistent scholarly record is often sufficient.
4. Build and nurture mentorship
You will typically need 3–4 strong letters of recommendation for your fellowship application. Start cultivating these relationships now.
Ideal letter writers:
- One or two subspecialists in your chosen field who know you well
- Your program director or chair
- Another general neurology attending who can speak to your overall clinical abilities
As a DO graduate, it’s particularly valuable if at least one letter writer is:
- Well-known regionally or nationally, or
- Connected to fellowship directors at other institutions
Meet with mentors every few months to:
- Update them on your interests, projects, and plans
- Ask honest questions about your competitiveness and strategy (e.g., “Should I apply broadly?” “Are there programs that particularly value DO graduates?”)
5. Begin thinking about the fellowship application timeline
Different neurology fellowships have different application cycles. Many use SF Match or ERAS, but some remain off-cycle or use direct application.
As you approach mid-PGY-3:
- Create a document listing:
- Target subspecialty(ies)
- Preferred geographic areas
- Programs of interest
- Application platform (ERAS, SF Match, or email/direct)
- Estimated application open dates, deadlines, and interview windows
This is the backbone of your fellowship application timeline.
PGY-4: Application, Interviews, and Decision-Making
PGY-4 is where all your preparation culminates into concrete steps: applications, interviews, and ranking or accepting offers.

1. Finalizing your fellowship application timeline
“How to get fellowship” depends heavily on hitting structural milestones on time. While exact dates shift annually and by subspecialty, a generalized framework:
- 12–18 months before fellowship start
- Many neurology fellowships open applications (e.g., around spring of PGY-3 for a July start after PGY-4)
- Interviews
- Typically 9–12 months before fellowship start
- Offers/Match
- Some go through formal neuro match systems; others offer positions on a “first come, first serve” rolling basis
Because there is substantial variation:
- Check each program’s website individually.
- Email coordinators early if information is unclear.
- Talk to senior residents: they often have “hidden curriculum” knowledge about actual timelines, especially for niche fellowships.
2. Application materials: making them DO-strong, not DO-limited
Your core application elements:
Curriculum Vitae (CV)
- Clearly list your DO degree and residency training
- Emphasize neurology-specific achievements
- Highlight your scholarly work, teaching, leadership, and QI projects
Personal Statement
- Tell a concise, coherent story:
- Why neurology?
- Why this subspecialty?
- How your DO training shaped your clinical perspective (e.g., whole-person care, communication, longitudinal relationships)
- What you hope to do with your fellowship training (clinical practice, teaching, research, program-building)
- Keep it focused on professional growth rather than revisiting medical school application themes.
- Tell a concise, coherent story:
Letters of Recommendation
- Request letters at least 1–2 months before deadlines.
- Provide your CV, personal statement draft, and a brief highlights document (bullet points about key clinical encounters or projects you shared with the letter writer).
- If there are concerns (e.g., you struggled early in residency but improved), discuss whether and how they might address your growth.
Transcript and Board Scores
- Ensure everything is updated and submitted correctly.
- Some fellowships may be less rigid about specific score cutoffs in neurology than in ultra-competitive fields like dermatology or plastics, but strong performance is always an asset.
3. Targeting the right programs as a DO graduate
When crafting your programs list:
- Consider:
- Historical openness to DO graduates (ask current fellows, look at alumni pages)
- Clinical vs research emphasis
- Case volume and disease mix
- Faculty interests and mentoring track records
- Fellowship graduates’ career paths
Apply broadly enough to:
- Avoid overconcentration on only “top 5” institutions
- Include a mix of:
- Highly academic programs
- Strong clinical programs
- A few safety options (if your application is middle-of-the-road)
For many DO graduates, this balanced strategy leads to a healthier neuro match outcome.
4. Interview preparation and performance
Before interviews:
- Research each program:
- Key faculty names in your subspecialty
- Unique features (e.g., specialized clinics, research centers, procedures)
- Recent publications in their area
Prepare to answer:
- “Why this subspecialty?”
- “Why our program?”
- “What are your 5- and 10-year career goals?”
- “Tell me about a challenging clinical case and what you learned.”
- “What does being a DO mean in your day-to-day care?”
As a DO graduate, be ready to articulate:
- How your osteopathic background shapes your neurologic care (e.g., attention to function, lifestyle, and psychosocial context)
- How you’ve succeeded in an ACGME neurology residency and worked effectively on multidisciplinary teams
During interviews:
- Be collegial and curious
- Ask specific questions:
- “How are fellows integrated into teaching?”
- “What do your fellows typically do after graduation?”
- “How is mentorship structured for research or quality projects?”
- Pay attention to program culture:
- How fellows are treated
- Faculty dynamics
- Workload, call structure, and support systems
5. Ranking and making a final decision
If your subspecialty uses a formal match, you’ll submit a rank list. If not, you may receive offers by email or phone and have to decide quickly.
Consider:
- Fit with your career goals (academic vs community; research vs clinical)
- Geographic needs (family, partner, cost of living)
- Program culture and mentorship
- Case mix and procedural exposure
Think long-term: preparing for fellowship is not just about the next 1–2 years, but about the trajectory it will set for your neurology career.
Special Considerations for DO Graduates in Neurology
Addressing Osteopathic Training in Your Application
You do not need to apologize for or over-explain being a DO graduate. Instead:
- Mention osteopathic principles as a strength:
- Holistic patient assessment
- Attention to functional outcomes
- Emphasis on communication and patient autonomy
- If you use OMT in practice (less common in neurology, but possible):
- Briefly describe when and how—without making it the center of your narrative unless relevant to the fellowship (e.g., headache medicine, pain).
Emphasize that your clinical training aligns fully with ACGME neurology standards and that you’ve cared for diverse, complex neurologic patients.
From Osteopathic Residency Match Mindset to Fellowship Strategy
If you experienced the transition from the osteopathic residency match system to the unified ACGME process, you may have lingering questions about how competitive you are compared with MD peers.
To recalibrate:
- Ask your program leadership for transparent feedback on your standing.
- Look at where recent graduates (DO and MD) from your program have matched for neurology fellowship.
- Use that data to guide your target list and level of program competitiveness.
Preparing for Fellowship vs Preparing for Practice
You might be torn between going straight into practice after residency vs pursuing fellowship.
As you weigh options:
- Consider your desired scope of practice:
- Do you want a highly specialized neuro practice (e.g., exclusively movement disorders)?
- Or a broad general neurology practice with a subspecialty niche?
- Talk to:
- Recent graduates who went straight into practice
- Recent fellows who completed subspecialty training
Remember, some neurologists practice for a few years, then return to fellowship. However, some fellowships prefer or require recent residency graduates, and your application may be stronger if you maintain ongoing academic engagement.
Preparing for Fellowship While Looking Ahead to Post-Fellowship Life
Fellowship is a bridge—not the final destination. As you’re preparing for fellowship, also think about how to get fellowship training to pay dividends in the long-term.
Academic vs Community Career Paths
Academic path
- More emphasis on research, teaching, and program-building
- Fellowship training is often expected or required
- A strong fellowship (with mentors and projects that lead to publications) is especially important
Community or private practice path
- Fellowship can still provide marketable expertise (e.g., EMG, EEG, Botox injections, MS treatment)
- May allow you to negotiate better positions (e.g., building a stroke program, leading a headache clinic)
Preparing for Future Leadership and Advanced Training
During fellowship, opportunities may arise for:
- Additional certifications (e.g., neurosonology, EEG/EMG boards, neuroimaging certifications)
- Research skills training (e.g., clinical trials methodology, outcomes research)
- Leadership courses or quality improvement training
By starting your planning early in residency:
- You can choose fellowships that align with longer-range leadership or academic goals.
- You can put yourself on a clear path to answer not only “how to get fellowship,” but also “how to make fellowship the launchpad for the career you really want.”
FAQs: Fellowship Preparation for DO Graduates in Neurology
1. As a DO graduate in neurology, am I at a disadvantage when applying for fellowship?
Many neurology fellowship programs are DO-friendly, and the unified ACGME era has reduced barriers. Your competitiveness depends far more on your overall profile (clinical performance, letters, research, professionalism) than on your degree alone. That said, if you’re aiming for top-tier academic centers, you may need to be especially proactive in building research experience and networking. Strong mentoring and targeted applications can more than offset any residual bias.
2. When should I start seriously preparing for fellowship during residency?
Awareness should start in PGY-1, but serious, structured preparation ramps up in PGY-2 and especially PGY-3. By early PGY-3, you should ideally:
- Have a narrowed subspecialty interest (or two)
- Be involved in at least one scholarly project
- Be planning subspecialty electives
- Be building relationships with potential letter-writers
By late PGY-3, you should be assembling your fellowship application timeline and materials.
3. How important is research for neurology fellowship, especially for DO graduates?
Research is not mandatory for all fellowships, but it helps significantly—especially for academic or highly competitive programs. At minimum, aim for:
- One or two case reports or posters
- Participation in at least one substantive project
For research-heavy fields (e.g., neuroimmunology, cognitive neurology at academic centers), more substantial research may be expected. As a DO graduate, scholarly work can help demonstrate academic engagement and offset any preconceived notions.
4. Can I still get a good fellowship if my neurology residency is not at a big-name academic center?
Yes. Many excellent fellows come from smaller or community-based neurology programs. To maximize your chances:
- Seek strong mentorship and letters from respected faculty
- Build a clear, focused CV with evidence of subspecialty interest
- Attend conferences and network
- Apply broadly, including institutions that traditionally welcome trainees from a variety of backgrounds
Programs value motivated, clinically strong applicants who will fit well with their teams—name recognition helps, but it’s not the only route to a successful neuro match.
Fellowship preparation as a DO graduate in neurology is about strategy, consistency, and self-awareness—much more than it is about pedigree. By understanding the landscape, building a strong neurology residency foundation, and using PGY-2 and PGY-3 wisely, you can enter the fellowship application cycle with confidence and a clear story about who you are as a neurologist and where you’re headed.




















