Understanding the Landscape: Fellowships After Anesthesiology Residency for DO Graduates
For a DO graduate in anesthesiology, fellowship preparation starts long before you submit your first application. The fellowship training environment is increasingly competitive, but DO graduates are matching into top programs in every major subspecialty. The key is understanding the landscape and building a strategic, stepwise plan.
Common Anesthesiology Fellowships
Most anesthesiology residents—MD and DO—who pursue advanced training tend to gravitate toward a core set of ACGME-accredited fellowships:
- Adult Cardiothoracic Anesthesiology
- Critical Care Medicine
- Pain Medicine
- Pediatric Anesthesiology
- Regional Anesthesiology & Acute Pain Medicine
- Obstetric Anesthesiology
- Neuroanesthesiology (fewer programs formally accredited but growing)
- Research or Clinician–Scientist tracks (often customized)
As a DO graduate, you are eligible for the same anesthesiology fellowship opportunities as MD colleagues, particularly now that accreditation has unified under the ACGME. However, your application must clearly demonstrate competitiveness and address any lingering misconceptions some faculty may have about osteopathic training.
Why Fellowship Makes Sense for Many DO Anesthesiologists
Reasons DO anesthesiologists often pursue fellowship training include:
- Depth of expertise in a niche area (e.g., regional, cardiac, peds)
- Improved job opportunities and marketability, particularly in academic or quaternary centers
- Higher earning potential in some subspecialties (e.g., pain, cardiac)
- Scholarly career foundation, especially if you are preparing for fellowship with an eye toward research or education
- Professional identity and satisfaction, doing the type of work you enjoy most every day
When planning how to get fellowship positions, you should first define your career goals and then align your residency experiences, scholarly work, and mentorship around that vision.
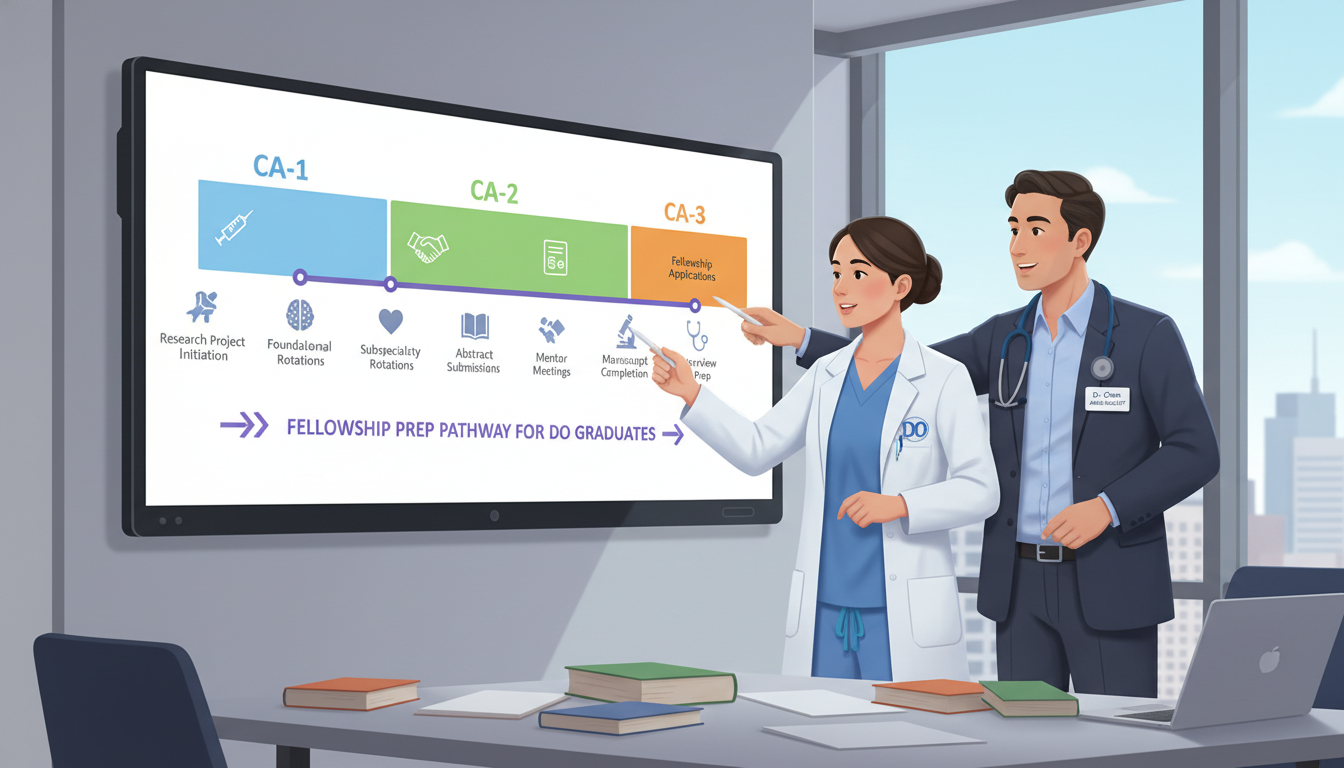
Timeline: When to Start Preparing for Fellowship
Understanding the fellowship application timeline is crucial. Most anesthesiology subspecialty fellowships participate in the SF Match or NRMP match (depending on specialty), with application dates that may feel surprisingly early in residency.
General Timeline Overview
Exact dates vary by subspecialty and year, but a typical structure looks like this:
- CA‑1 (PGY‑2) Year
- Early exploration and career conversations
- Begin targeted reading and exposure to subspecialties
- Start participating in a research or QI project
- CA‑2 (PGY‑3) Year
- Core year for decisions and preparation
- Solidify specialty interest by mid-year
- Request and complete focused elective rotations
- Intensify scholarly output and networking
- Start drafting your personal statement by spring
- Late CA‑2 to Early CA‑3 (PGY‑3 to PGY‑4)
- Most anesthesiology fellowship applications open and are due
- SF Match or NRMP registration
- Interview season
- CA‑3 (PGY‑4) Year
- Rank lists, match result, and contract signing
- Transition planning for fellowship
Because applications often go in toward the end of CA‑2 or very early CA‑3, the real work of preparing for fellowship happens in CA‑1 and CA‑2.
Specialty-Specific Timing Nuances
- Pain Medicine (NRMP)
- Applications often open late CA‑2, with interviews across CA‑3
- Critical Care and Adult Cardiothoracic (SF Match/NRMP depending on program)
- Similar early CA‑3 match cycles; some variability
- Pediatric, Regional, Obstetric Anesthesiology
- Usually align with common timelines but always check SF Match and individual program websites
Action step: By mid‑CA‑1 year, look up current anesthesiology subspecialty deadlines via SF Match, NRMP, and key society websites (e.g., ASA, SCA, SOAP, SPA, ASRA, SCCM).
Building a Competitive Fellowship Profile as a DO Resident
The fundamentals for a strong anesthesia match at the fellowship level are similar for DO and MD graduates—but DO residents must be especially intentional in a few areas: academic productivity, visibility, and standardized metrics.
1. Clinical Excellence and Evaluations
Nothing substitutes for being a consistently reliable, technically solid resident.
Fellowship program directors commonly look for:
- Strong rotation evaluations, especially in relevant subspecialty rotations (cardiac, peds, ICU, OB, regional)
- Evidence of progressive responsibility: management of complex cases, leadership in the OR, and comfort with sick patients
- Professionalism and teamwork: your reputation among CRNAs, nurses, surgeons, and fellow residents often finds its way into letters and conversations
As a DO graduate, robust evaluations help underscore that your performance is indistinguishable from (or better than) your peers from any background.
Actionable tips:
- Ask for feedback at the midpoint of each rotation and implement changes quickly.
- On key electives (e.g., cardiac if you want CT anesthesia), explicitly tell the rotation director you’re preparing for fellowship so they can observe you for a potential letter.
- Keep a simple log of notable cases and responsibilities—it will help you reflect and articulate your growth in your personal statement and interviews.
2. Board Exams and Standardized Metrics
Many DO anesthesiology residents now take:
- COMLEX-USA (required for DOs)
- USMLE Step exams (optional but often beneficial for competitive subspecialties or academic centers)
By the time you are preparing for fellowship, your Step/COMLEX scores are already set, but you can:
- Highlight improvement over time if your early scores were modest but later exams (e.g., ITE, BASIC exam) are stronger.
- Emphasize successful completion of the ABA BASIC exam and strong in-training exam performance as evidence of content mastery.
If your metrics are average, you can offset this through strong letters, excellent interview performance, and evidence of commitment to your chosen subspecialty.
3. Scholarly Activity: Research, QI, and Education
In today’s anesthesiology fellowship market, a DO graduate residency profile without any scholarly activity is at a disadvantage, especially for university-based programs.
Common, realistic pathways:
- Case reports and case series (especially in peds, cardiac, neuro, or complex regional techniques)
- Quality improvement projects (e.g., ERAS protocols, postoperative pain pathways, POCUS documentation initiatives)
- Retrospective chart reviews (e.g., outcomes with certain blocks, airway strategies, transfusion practices)
- Educational projects (developing a simulation curriculum or workshops for medical students)
Aim for:
- At least one to two abstracts or posters presented at a regional or national meeting (ASA, ASRA, SCA, SOAP, SPA, SCCM, etc.).
- Submitting at least one manuscript by the time you apply, even if still under review.
For a DO graduate, this is particularly helpful in demonstrating your academic potential and neutralizing any lingering structural biases that some historically MD-dominant institutions may still harbor.
How to start quickly:
- In CA‑1, ask your department’s research director: “I’m interested in [pain/cardiac/peds/critical care/regional]. Are there any active projects where I can plug in now?”
- Leverage existing databases and QI initiatives rather than designing a project from scratch.
- Learn simple tools: REDCap, basic statistics via R or SPSS (even just enough to collaborate effectively).
4. Letters of Recommendation: Whom and How to Ask
Strong, specific letters can make or break an anesthesia match to fellowship.
You’ll usually need 3–4 letters, including:
- Program Director (PD) or Department Chair
- Subspecialty mentor in your chosen field (e.g., fellowship-trained cardiac anesthesiologist if applying CT)
- Another faculty who knows you well clinically or through research
For DO graduates, letters from well-known, academically active attendings can be especially valuable.
Strategies:
Target potential letter writers early in CA‑2, and let them know you’re hoping to earn a letter based on your performance.
Provide them with:
- Your updated CV
- Draft of your personal statement
- Bullet points of experiences and accomplishments you’d like them to highlight
- The specific subspecialty and program types you’re aiming for
Choose attendings who can say, for example:
“I have worked with dozens of fellows and residents over 20 years, and Dr. X (DO) performs at the top tier in clinical judgment, work ethic, and technical skills.”
That sort of comparative statement carries weight.
Strategic Career Planning: Choosing the “Right” Fellowship for You
Knowing how to get fellowship training starts with choosing the fellowship that fits your specific skills, values, and life goals—not just the one that seems most prestigious.
Key Questions to Clarify Early
Ask yourself:
- What patient population and pace do I enjoy?
- High-acuity ICU vs. controlled OR environment vs. clinic-based pain practice
- How important is schedule predictability vs. procedural intensity?
- Pain medicine and some regional practices may offer more outpatient, business-hours work; cardiac and critical care can be more demanding and variable.
- Do I envision a primarily clinical, academic, or hybrid career?
- Academic tracks often favor fellowships with strong research and teaching infrastructure.
- Where do I want to live and practice long-term?
- Some fellowships are strong regional pipelines (e.g., a major academic center often feeds into its own or affiliated health systems).
Specialty-Specific Considerations
- Adult Cardiothoracic Anesthesiology
- Ideal if you enjoy TEE, high-stakes physiology, and complex hemodynamics
- Best for those comfortable with long cases and intensive intraoperative management
- Critical Care Medicine
- Heavy focus on physiology, multi-organ failure, ventilator management, and longitudinal patient relationships
- Can be a bridge to academic careers and leadership roles in ICU medicine
- Pain Medicine
- Hybrid of clinic, procedures, and often multidisciplinary care
- Business aspects and regulatory landscape (opioids, interventional coding) are important to understand
- Pediatric Anesthesiology
- Requires comfort with children and families, specialized physiology, and often high-acuity surgeries in a narrow patient-size range
- Regional Anesthesiology & Acute Pain
- Great if you love ultrasound, anatomy, and perioperative pain optimization
- Plays a central role in ERAS and outpatient surgery growth
- Obstetric and Neuroanesthesiology
- More niche but valuable in tertiary centers and academic practice
DO-Specific Career Strategy Tips
As a DO graduate:
- Consider fellowships at institutions with a track record of training DO residents and fellows. These programs may already recognize the strengths of osteopathic training.
- But don’t limit yourself—you can absolutely match at historically MD-heavy academic centers. The key is a strong CV, strong letters, and deliberate networking.

Making Your Application Stand Out: Practical Steps for DO Anesthesiology Residents
The core components of your fellowship application are:
- CV
- Personal statement
- Letters of recommendation
- Application form (ERAS, SF Match, or institutional system)
- Interview performance
Crafting a Compelling CV
Your CV should tell a cohesive story that supports your subspecialty choice.
Key sections:
- Education and training (include both DO school and residency)
- Honors and awards (chief resident, teaching awards, scholarships)
- Research and publications (list in standard citation format)
- Presentations (posters, oral presentations, invited talks)
- Leadership and service (committee roles, resident council, medical student teaching)
- Professional memberships (ASA, subspecialty societies, osteopathic associations)
For a DO graduate, consider:
- Including osteopathic-related activities (e.g., OMM workshops, DO leadership roles) if relevant, but contextualize them in terms of broader educational or clinical impact.
- Emphasizing longitudinal growth—how you built from smaller roles (e.g., case reports) to larger ones (e.g., QI project lead).
Personal Statement: Tell a Focused Story
Your personal statement is not a generic essay; it should answer three subtle questions:
- Why this subspecialty?
- Why you? (What do you bring?)
- Why now, and what are your long-term goals?
Consider this structure:
- Opening vignette: A concise clinical moment that crystallized your interest (e.g., your first time managing a failing ventricle on bypass, a complex pediatric case, or a challenging chronic pain patient whose function improved).
- Development of interest: Specific rotations, mentors, or projects that reinforced your commitment.
- What you’ve done to prepare: Skills, research, leadership, teaching, QI.
- Career vision: How the fellowship will help you achieve short- and long-term goals (clinical excellence, academic work, system improvement).
If you feel your osteopathic background is an asset—for example, in pain medicine or regional anesthesia where whole-person care and physical exam skills matter—briefly highlight how your DO training shapes your patient interactions and philosophy without turning it into the entire essay.
Targeted Program Selection and Networking
To improve your odds in the osteopathic residency match for fellowships:
- Create a tiered list of programs:
- Reach (highly competitive academic centers)
- Target (strong fit with your profile)
- Safety (programs where your mentors believe you will be very competitive)
Use multiple data sources:
- Fellowship program websites
- Current and past fellows from your institution
- Society directories (e.g., SCA, SPA, ASRA lists)
- Program reputations for DO-friendliness (ask senior residents and faculty)
For networking:
- Attend at least one major conference in your subspecialty during CA‑2 or early CA‑3.
- Introduce yourself to program directors or key faculty after attending their talks or poster sessions.
- When emailing, keep it concise and specific:
- Who you are (DO anesthesiology resident, PGY level)
- Your subspecialty interest
- A brief note about your research or clinical focus
- A question or expression of interest in their fellowship
Networking cannot guarantee a position, but it can ensure your application is read more carefully and sometimes translates into interview offers.
Interview Preparation: Converting Interviews into Offers
Once interviews are secured, your focus shifts to:
- Communicating clearly who you are and what you want
- Demonstrating maturity, teachability, and alignment with the program’s mission
Expect to discuss:
- Complex or challenging clinical cases and what you learned
- Your research or QI work—understand your methodology and outcomes
- Why this specific fellowship and this institution
- How you handle stress, conflict, and error disclosure
As a DO applicant, you may occasionally be asked (explicitly or implicitly) about your choice of osteopathic training. This is an opportunity, not a trap:
- Frame it positively: emphasize comprehensive care, communication skills, and how your training prepared you to integrate procedures with whole-patient management.
- Avoid defensiveness—your goal is to project confidence and professionalism.
Practice:
- Arrange mock interviews with mentors or program leadership.
- Prepare 3–4 concrete stories that illustrate:
- Leadership under pressure
- Managing a complication or error
- Teaching or mentoring junior trainees
- A situation where you improved a process or system
Balancing Residency Demands with Fellowship Preparation
The residency life and challenges phase is real—you’re juggling night calls, complex cases, exams, and real human lives, all while preparing for fellowship and sometimes planning for family or partner considerations.
Time Management Strategies
- Block off protected time monthly for career development tasks:
- Updating your CV
- Literature review in your subspecialty
- Touching base with your primary mentor
- Use micro-moments:
- Read one article during downtime between cases or in the call room
- Draft bullet points for your personal statement on your phone after a memorable case
- Batch tasks:
- Send all recommendation requests in one well-planned wave
- Set aside a weekend to finalize application materials before busy call months
Wellness and Sustainability
Burnout is a real risk during this period. To maintain performance while preparing for fellowship:
- Protect sleep around critical days (e.g., exam days, key rotations, interviews).
- Keep at least one non-negotiable wellness habit (exercise, journaling, spiritual practice, or regular time with loved ones).
- Use your institutional resources if needed—resident wellness programs, counseling, or peer support.
Remember: fellowship directors want trainees who are not only high-performing but also sustainable, self-aware clinicians.
FAQs: Fellowship Preparation for DO Anesthesiology Graduates
1. As a DO anesthesiology resident, can I realistically match into top academic fellowships?
Yes. Many DO graduates successfully match into competitive academic fellowships in cardiac, critical care, pain, peds, and regional. Your competitiveness depends far more on:
- Clinical evaluations and reputation
- Scholarly activity and letters
- Interview performance and fit
than on degree type alone. Strategic preparation, strong mentorship, and visible engagement in your chosen subspecialty can more than offset any historical bias.
2. Do I need to take USMLE as a DO to be competitive for anesthesiology fellowship?
Not strictly, but it can help—particularly for historically MD-dominant, research-heavy academic centers that are accustomed to interpreting USMLE scores. If you already took and passed USMLE during medical school, great—include it. If not, by residency it’s too late to change that; instead:
- Emphasize strong COMLEX performance
- Highlight ABA BASIC and in-training exam results
- Strengthen the rest of your application (research, letters, clinical excellence)
3. How early should I start research if I know I want an anesthesiology fellowship?
Ideally early in CA‑1. Starting then allows enough time to:
- Learn the basics of study design and data collection
- Present abstracts at regional or national meetings
- Potentially get a manuscript accepted or in-press before applications
If you’re starting later (late CA‑1 or early CA‑2), focus on feasible projects (case reports, chart reviews, QI initiatives) that can still generate presentable work within months, not years.
4. What if I’m undecided about which fellowship to pursue during CA‑1?
That’s common. Use CA‑1 and early CA‑2 to:
- Gain broad exposure: take every opportunity on cardiac, OB, neuro, peds, and regional cases.
- Arrange short, focused electives in 1–2 areas you’re most curious about.
- Talk to attendings and fellows about their daily work, career satisfaction, and lifestyle.
Aim to narrow down to one primary target subspecialty by mid‑CA‑2, so you can align electives, research, and letters with that choice before the anesthesia match cycle starts.
By approaching your anesthesiology residency with intention—aligning rotations, mentorship, scholarship, and networking around clearly defined goals—you position yourself as a compelling, well-prepared DO graduate for any anesthesiology fellowship. The path is demanding, but with a structured plan and the right support, it is absolutely achievable.




















