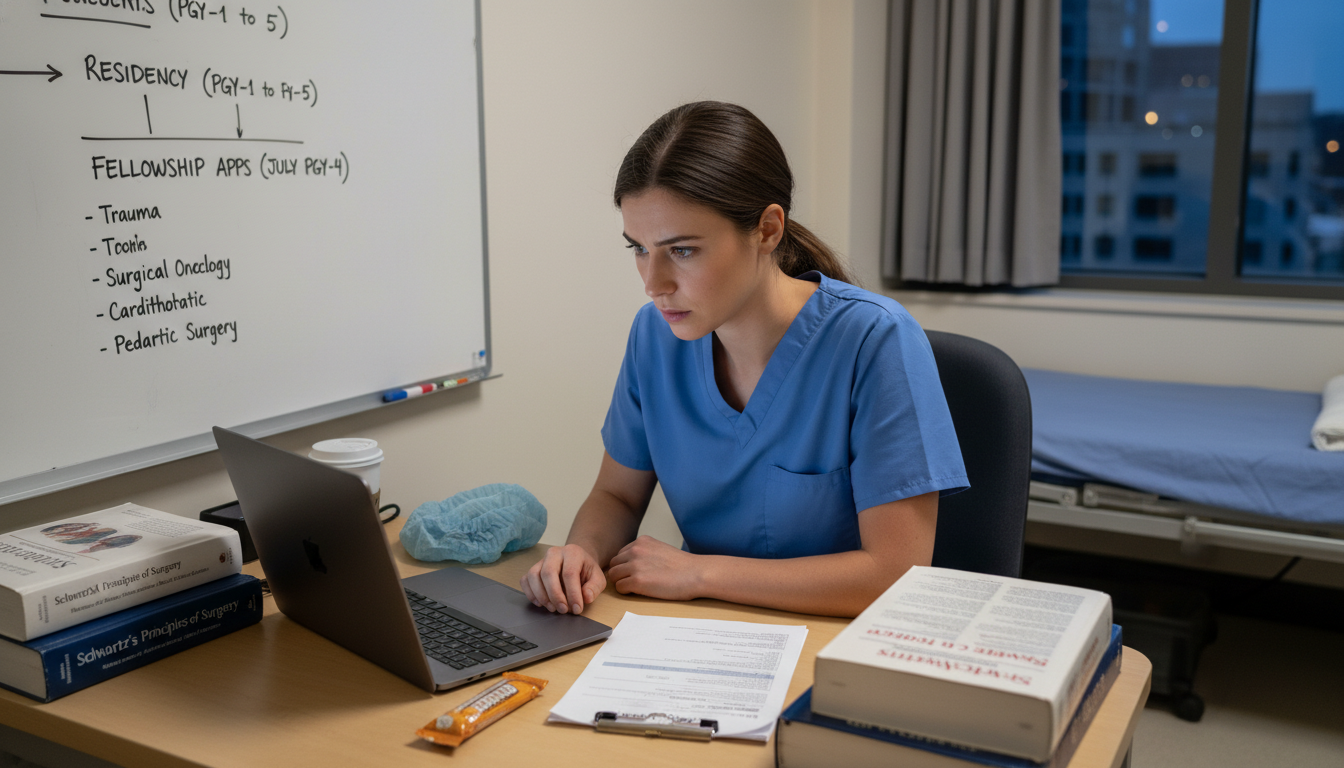
Understanding the Fellowship Landscape for General Surgery MD Graduates
For an MD graduate in general surgery, fellowship preparation begins far earlier than most residents realize. The pathway from allopathic medical school match to a successful surgery residency match and, ultimately, to a competitive fellowship is a continuum. Strategic planning during residency can dramatically expand your options later, whether you aim for surgical oncology, minimally invasive surgery, colorectal, vascular, trauma/critical care, pediatric surgery, or another subspecialty.
Fellowship training has become the norm rather than the exception in general surgery. In many programs, well over 70% of chief residents pursue at least one fellowship. Understanding this landscape early allows you to make deliberate choices instead of scrambling in your PGY-4 year.
Key early concepts:
- Fellowship is highly structured and competitive. Timeline, letters, case logs, and research all matter.
- Your reputation is your currency. Faculty opinions, OR performance, and professionalism will follow you.
- Your goals may evolve. You don’t need to declare as an intern, but you do need to explore thoughtfully.
This article walks through a practical, stepwise approach to fellowship preparation specifically for MD graduates in general surgery, from PGY-1 through application season and beyond.
Clarifying Your Career Vision: Do You Need a Fellowship?
Before you commit to a particular fellowship application timeline, you need clarity on your long-term goals. Not every general surgeon needs fellowship training, but most academic and many high-volume community positions now expect subspecialty expertise.
Questions to Ask Yourself
What kind of practice do I envision?
- Largely elective vs. emergency/trauma-heavy
- Academic vs. community vs. hybrid model
- Rural, suburban, or urban
- Outpatient-focused vs. OR-heavy vs. ICU-based
Which rotations have energized me the most?
- Do you lose track of time in the OR during colorectal or endocrine?
- Do you love the complexity of trauma resuscitations and ICU management?
- Do you enjoy longitudinal relationships (breast, bariatric, colorectal)?
How much do I value research, teaching, and leadership?
- Academic tracks and certain fellowships (surgical oncology, transplant, pediatric) favor research-heavy residents.
- Some clinically focused fellowships (MIS, colorectal) may emphasize case volume and technical performance more heavily, though research still matters.
Lifestyle, geography, and family considerations
- Some fellowships are more geographically clustered (e.g., pediatric surgery, transplant).
- Call burden and acuity vary greatly between, say, breast surgery and trauma/critical care.
Common Fellowships After General Surgery
You don’t need to choose now, but recognizing options helps you shape your experiences:
- Surgical Oncology
- Minimally Invasive/Bariatric Surgery
- Colorectal Surgery
- Vascular Surgery (independent track)
- Trauma and Surgical Critical Care
- Acute Care Surgery
- Hepatopancreatobiliary (HPB) Surgery
- Breast Surgical Oncology
- Transplant Surgery
- Endocrine Surgery
- Pediatric Surgery
- Cardiothoracic Surgery (traditional independent route in some settings)
Each has different competitiveness levels, research expectations, and required case exposures.
Actionable step (PGY-1 to PGY-2):
Create a simple “interest map” listing 3–4 fellowships that currently appeal to you. For each, note:
- Why it interests you
- Major perceived pros/cons
- Any faculty at your institution in that subspecialty
You aren’t committing; you’re setting targets for exploration.
Building a Competitive Fellowship Profile During Residency
From the moment you enter your surgery residency match program, each year builds your narrative. Fellowship directors look for patterns of commitment, excellence, and growth, not perfection from day one.
1. Academic and Clinical Performance
As an MD graduate from an allopathic medical school, you already demonstrated you can succeed in structured environments. Now that continues in residency.
Core expectations:
- Strong clinical evaluations: Consistently “meets” or “exceeds” expectations in:
- Clinical reasoning and decision-making
- Situational awareness and team communication
- Reliability and ownership of patient care
- Operative performance: Progressive responsibility in the OR:
- Knowing the steps and anatomy cold
- Anticipating instruments and next moves
- Soliciting feedback and acting on it
Fellowship directors pay attention to:
- Patterns in semiannual evaluations
- Comments about professionalism, work ethic, and leadership
- Milestone progression (e.g., ACGME milestones)
Actionable advice:
- Ask senior residents and faculty directly: “What are 1–2 things that would make me stronger as a PGY-2/3 aiming for fellowship X?”
- Track your own OR cases monthly; note where you are primary vs. assistant.
2. Research and Scholarly Activity
For many competitive fellowships, particularly in academic settings, research is a major differentiator.
Types of scholarly activity that matter:
- Peer-reviewed publications: Clinical outcomes, quality improvement, basic science (depending on your interest)
- Conference presentations: Oral or poster presentations at ACS, SAGES, AAS, EAST, SSAT, etc.
- Quality improvement (QI) projects: Especially if tied to publication or measurable impact
- Book chapters or review articles: Show depth in your chosen subspecialty
Timing and expectations by fellowship:
- Highly competitive, academic fellowships (surgical oncology, pediatric surgery, transplant, HPB):
- Often expect multiple first- or co-first-author publications
- A dedicated research year (or two) significantly strengthens your profile
- Clinically focused fellowships (MIS, colorectal, trauma/critical care, breast):
- Research is still valued but may not require a 1–2 year dedicated research block
- Even 2–4 well-executed projects can help your application stand out
Actionable steps by training level:
- PGY-1 to early PGY-2:
- Join a faculty project in a potential interest area (retrospective chart review, database analysis, QI).
- Learn basic data management tools (Excel, REDCap, basic statistics).
- PGY-2 to PGY-3:
- Aim to lead at least one project as first author.
- Submit abstracts to regional/national meetings.
- Decide whether a dedicated research year aligns with your goals and your program’s culture.
- PGY-3 to PGY-4:
- Focus on completing and submitting manuscripts.
- Strategically prioritize projects most aligned with your desired fellowship.
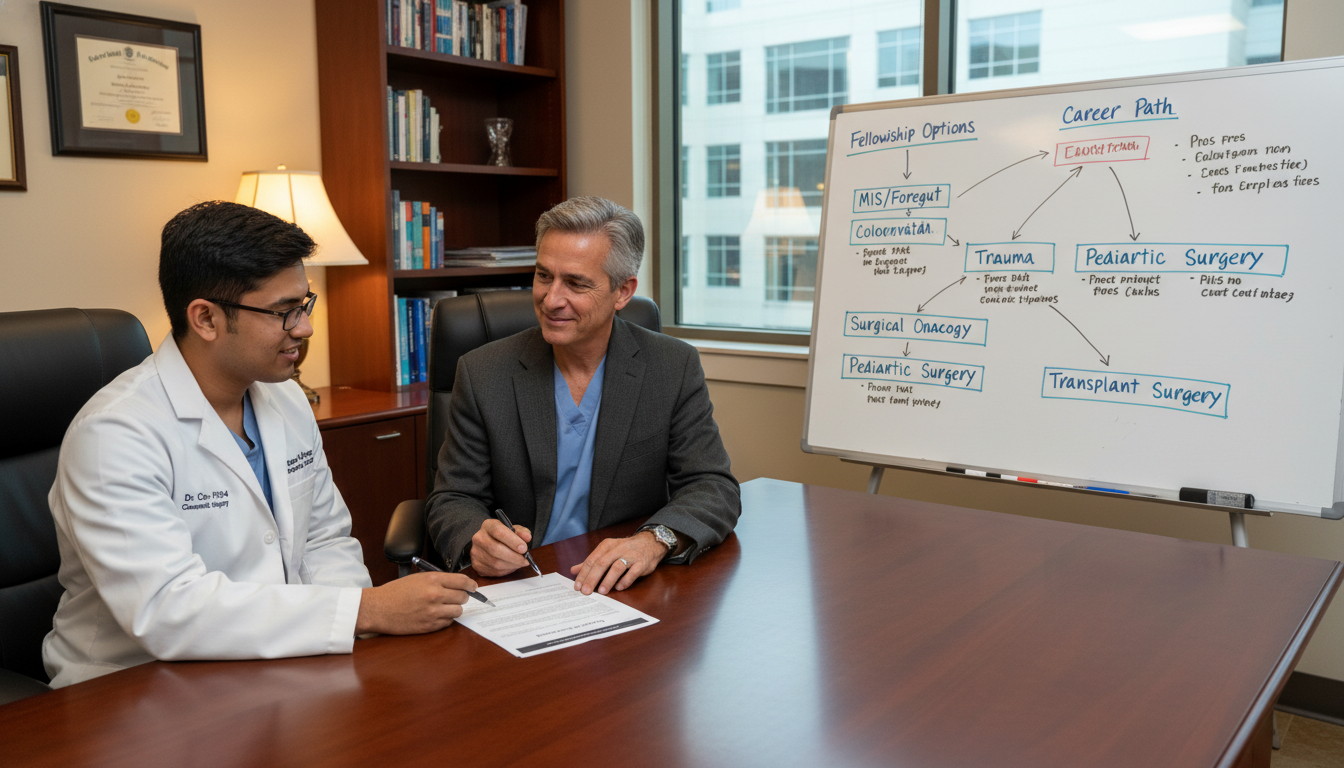
3. Mentorship and Networking
Mentorship is one of the most powerful determinants of fellowship success, both for guidance and for strong letters of recommendation.
Types of mentors you need:
- Career mentor: Helps you think long-term about whether and how to get fellowship, academic vs. community career, and work–life balance.
- Content mentor (subspecialty): A surgeon in your area of interest who can connect you to research, conferences, and key people nationally.
- Process mentor: Someone who recently navigated the same fellowship application timeline (chief resident, recent graduate, or junior faculty).
How to build these relationships:
- Schedule annual or semiannual check-ins with your main mentor.
- Seek consistent involvement with one or two subspecialty services (elective rotations, research meetings, M&M, tumor board).
- Attend national conferences and introduce yourself to leaders in the field; your faculty mentors can facilitate introductions.
Red flags to avoid:
- Depending on a single letter writer who is too busy or not well known in the field.
- Waiting until PGY-4 to tell potential mentors you’re interested in their subspecialty.
Fellowship Application Timeline: Year-by-Year Roadmap
Your fellowship application timeline will differ slightly by subspecialty and by whether the match is via NRMP, SF Match, or another system. Still, the overall framework is similar for most general surgery fellowship paths.
PGY-1: Exploration and Foundation
- Focus: Becoming a safe, reliable intern.
- Start documenting:
- Cases and index procedures
- Any research you join
- Attend:
- Departmental grand rounds
- Subspecialty conferences (tumor board, M&M, specialty conferences)
Target actions:
- Identify at least one possible subspecialty interest.
- Join 1–2 research or QI projects (even as a collaborator).
PGY-2: Narrowing Interests and Early Productivity
- Focus: Taking on more operative responsibility, demonstrating growth.
- Academic:
- Aim to submit at least one abstract.
- Attend a national meeting if feasible.
- Career:
- Choose 1–2 fellowship paths to explore more seriously.
- Meet with at least one potential subspecialty mentor formally.
Target actions:
- Ask your program leadership about expectations and support for a research year (if appropriate).
- Begin to understand specific fellowship application cycles (e.g., colorectal vs. MIS vs. trauma).
PGY-3: Commitment and Strategic Positioning
This is often the pivotal year for fellowship preparation.
- Clinical:
- Solidify your OR skills and leadership on call.
- Research:
- Lead at least one project as first author.
- Plan to submit manuscripts before application season.
- Career:
- Decide whether you will apply for fellowship during PGY-4 or after a research/transition year.
- Identify your top 1–2 subspecialties definitively.
Target actions:
- Confirm which match system your desired fellowship uses (NRMP, ERAS, SF Match, or direct applications).
- Request early, informal feedback from mentors: “If I apply to [subspecialty], what will be my strengths and weaknesses?”
PGY-4: Application Preparation and Submission
This is the most intense phase of the fellowship application timeline.
Spring / Early PGY-4:
- Finalize your subspecialty choice.
- Update and polish your CV (clinical, academic, leadership).
- Write a draft personal statement; share with 2–3 trusted reviewers.
- Confirm:
- Opening dates for applications (often late winter to early summer)
- Deadlines for specific programs
- Match/offer dates
Letters of recommendation:
- Typically 3–4 letters, including:
- Program director’s letter
- Subspecialty mentor letter (ideally well-known in the field)
- Additional letters from respected faculty who know you well clinically and technically
- Ask at least 8–10 weeks before applications are due.
- Provide each letter writer with:
- Updated CV
- Draft personal statement
- Brief bullet list of your major accomplishments and goals
Summer / Mid PGY-4:
- Submit applications early in the cycle; some programs begin reviewing as soon as portals open.
- Begin interview preparation:
- Mock interviews with faculty or recent fellows.
- Review your own research and know it in depth.
- Be ready to discuss challenging cases, ethical dilemmas, and complications.
PGY-5: Interviews, Ranking, and Transition to Fellowship
- Interviews may run from late PGY-4 into PGY-5 depending on the fellowship.
- Continue to:
- Build your case log and operative independence.
- Finish and submit any pending research.
- Participate in:
- Mock OR teaching sessions
- Senior leadership roles (chief resident responsibilities)
After matching:
- Confirm onboarding requirements (licenses, hospital privileges, visas if applicable).
- Clarify expectations for your role and schedule during fellowship.
- If preparing for fellowship in a different region or country, plan for relocation early.

Strengthening Your Fellowship Application: Components and Strategy
To succeed in the surgery residency match, you learned how to package your story as a future general surgeon. For fellowship, you must demonstrate depth and focus within that story.
1. Curriculum Vitae (CV)
Your CV should clearly show the evolution from MD graduate to a maturing surgeon with a distinct subspecialty interest.
Key sections to optimize:
- Education and training (emphasize allopathic medical school match and reputable residency)
- Leadership roles (chief resident, committee member, QI initiatives)
- Research and publications (group by peer-reviewed, abstracts, invited talks)
- Teaching and mentoring (medical student teaching awards, simulations, workshops)
- Certifications and skills (ATLS, laparoscopic skills courses, advanced endoscopy training if relevant)
Tips:
- Use consistent formatting and clear headings.
- Highlight subspecialty-related activity; group relevant items where appropriate.
- Avoid clutter; fellowship reviewers skim dozens of CVs at a time.
2. Personal Statement
Your personal statement should be concise, specific, and future-oriented.
Address clearly:
- Why this subspecialty?
- What clinical and academic path led you here?
- How have you tested this interest (rotations, cases, research, mentors)?
- What specific fellowship features are you seeking?
- What do you hope to contribute to the field long term?
Pitfalls to avoid:
- Generic language that could describe any subspecialty.
- Overly dramatic or unsubstantiated claims.
- Excessive length; aim for about one page.
3. Letters of Recommendation
Strong letters are often the deciding factor in how to get fellowship offers from top programs.
Ideal letters:
- Written by faculty who know you well both in and out of the OR.
- Provide concrete examples of:
- Technical skill
- Clinical judgment
- Work ethic and resilience
- Growth over time
- Compare you favorably with peers (e.g., “top 5% of residents I’ve trained in 20 years”).
Strategies:
- Rotate frequently with your intended letter writers in PGY-3/4.
- Ask explicitly: “Do you feel you can write a strong letter for a fellowship in [subspecialty] for me?”
- Provide talking points that highlight subspecialty-relevant achievements.
4. Interviews and Program Fit
During fellowship interviews, programs are assessing both your technical potential and how well you will fit their team culture and clinical mission.
Common interview themes:
- “Walk me through a challenging case and how you managed it.”
- “Tell me about a complication you’ve had and what you learned.”
- “Where do you see yourself 5–10 years after fellowship?”
- “What strengths and weaknesses will you bring to our program?”
Your evaluation of programs:
Ask pointed questions about:
- Case volume and case mix (aligned with your goals?)
- Graduates’ career outcomes (academic vs. community)
- Faculty-to-fellow ratio and operative autonomy
- Research infrastructure and expectations
- Call responsibilities and ICU exposure (if relevant)
Preparing for Fellowship and Beyond: Transitioning from Resident to Subspecialist
Once you match into fellowship, preparation is not over—it simply shifts focus from “getting in” to “succeeding as a fellow” and preparing for your post-fellowship career.
Clinical Readiness
- Review core content in your subspecialty before starting:
- Key guidelines (e.g., NCCN for oncologic fields, SAGES for MIS)
- Landmark trials and practice-changing studies
- Update your case log:
- Identify gaps in experience you want to address during fellowship.
- Discuss those goals early with your fellowship director.
Professional Identity and Networking
- Use fellowship to:
- Build national-level relationships.
- Join subspecialty societies and interest groups.
- Volunteer for committee work if time permits.
Preparing for Your First Job
As you are preparing for fellowship and then moving toward independent practice, you will need to:
- Understand the timeline for job applications in your field.
- Clarify your priorities:
- Academic rank vs. operative volume vs. lifestyle
- Geographic constraints
- Seek job-search mentorship from:
- Fellowship director
- Recent graduates of your program
For some highly competitive fellowships (e.g., surgical oncology, HPB, transplant), the “job search” may begin informally during fellowship interviews and national meetings. Maintaining professionalism and reliability during both residency and fellowship will pay long-term dividends.
FAQs: Fellowship Preparation for MD Graduates in General Surgery
1. When should I decide if I want to pursue a fellowship?
You do not need to decide during your intern year, but by mid–PGY-3 you should have a strong sense of whether you are leaning toward fellowship and in which general area. This gives you enough time to build a focused record of experience and scholarship, align with mentors, and prepare a strong application during PGY-4.
2. Do I need a dedicated research year to match into a good fellowship?
It depends on your target subspecialty and the competitiveness of programs you’re aiming for. For highly academic fellowships (pediatric surgery, surgical oncology, transplant, HPB), a research year significantly strengthens your profile and is common among successful applicants. For MIS, colorectal, trauma/critical care, and some other clinically oriented fellowships, a dedicated research year is helpful but not mandatory if you can demonstrate solid productivity alongside your clinical duties.
3. How many programs should I apply to for fellowship?
This varies by subspecialty and your competitiveness. In more competitive fields, applicants often apply broadly (20+ programs). For others, 10–20 may suffice. Discuss this with your mentors; they can realistically assess your competitiveness and advise on a range that balances breadth and manageability in terms of interviews.
4. How do I balance fellowship preparation with my responsibilities as a chief resident?
During PGY-5, your primary responsibility remains safe patient care and leadership within your residency. Start the bulk of your application work in late PGY-3 and early PGY-4 so that by the time you are a chief, the major components (CV, publications, letters, and most interviews) are already in place. As a chief, leverage your experience: use your role to demonstrate leadership, maturity, and readiness for the next level—qualities fellowship directors value highly.
Thoughtful, early, and intentional fellowship preparation allows you to shape your career rather than simply react to opportunities. By understanding the fellowship landscape, building a coherent profile during residency, and managing the application process strategically, you can position yourself for a fulfilling subspecialty career that aligns with your skills, values, and long-term goals as a general surgeon.




















