
Understanding the Role of a Preliminary Medicine Year
For an MD graduate planning a preliminary medicine year (prelim IM), the program selection strategy can feel very different from applying to a categorical internal medicine or other core residency. A preliminary medicine year is typically a one-year, non-continued position in internal medicine that satisfies the clinical training requirement before entering an advanced specialty (e.g., neurology, anesthesiology, dermatology, radiology, PM&R).
Before deciding how to choose residency programs and how many programs to apply, you need a clear understanding of what the prelim year is meant to accomplish in your specific career path.
1. Why Preliminary Medicine Instead of Categorical IM?
MD graduates pursue a preliminary medicine year for several reasons:
- Matched into an advanced specialty (e.g., Radiology, Anesthesiology, Neurology) that requires a separate PGY‑1 year
- Planning to apply again to a competitive specialty and want strong inpatient experience plus letters of recommendation
- Desire for a broad-based clinical year before research, fellowship, or non-clinical work
Unlike categorical IM, a prelim IM year:
- Does not include guaranteed continuation to PGY‑2 IM training
- Is more service-heavy in some programs, especially at community hospitals
- Can vary widely in educational quality, procedural exposure, and schedule intensity
Understanding this distinction is critical to developing a program selection strategy that fits your goals.
2. Clarify Your Objective for the Prelim Year
Your strategic choices will depend heavily on your primary goal:
Matched to an Advanced Program Already (e.g., Radiology, Neurology)
- Priority: Solid clinical training, not burning out, geographic fit with advanced program.
- You can often be more selective and apply to fewer programs, provided your application is strong.
Reapplicant to a Competitive Specialty (e.g., Derm, Ortho, ENT, Plastics)
- Priority: Strong mentorship, time and support for research, opportunities for specialty-aligned rotations, high-quality letters.
- Program selection should focus on academic environments where you can network in your target field.
IM-Curious or Bridge Year While Reassessing Specialty Choice
- Priority: Thorough exposure to internal medicine, supportive teaching culture, good generalist training.
- Consider programs where you could potentially convert to categorical IM if the opportunity arises (not guaranteed, but sometimes possible).
Visa-Dependent or Location-Constrained Applicants
- Priority: Programs that sponsor your visa type (J‑1, H‑1B), and locations where you can reasonably live and work.
- You may need to apply more broadly numerically, but within your constraints.
Write down your goal explicitly; it will guide every downstream decision.

Core Factors in Choosing Preliminary Medicine Programs
When thinking about how to choose residency programs for a prelim IM year, avoid treating it as an afterthought to your advanced specialty. Your PGY‑1 experience will profoundly shape your clinical skills, confidence, and wellbeing.
Here are the key factors to evaluate systematically.
1. Program Type: Academic vs Community vs Hybrid
Academic Medical Centers
- Pros: Tertiary/quaternary care, specialty exposure, more sub-specialty consults, more teaching.
- Good for: Those planning academic careers, research, or competitive specialty reapplication.
- Cons: Often busier, complex patients, sometimes less time for research in prelim roles.
Community Hospitals
- Pros: More hands-on responsibility, continuity with attendings, potentially more procedures.
- Good for: Those wanting strong generalist skills and autonomy.
- Cons: Fewer research opportunities, less exposure to rare conditions, variable teaching.
Hybrid (University-Affiliated Community)
- Pros: Balance of hands-on experience and academic resources.
- Good for: Many prelim applicants seeking well-rounded training.
Align this with your goal: an MD graduate repeating applications to a competitive advanced field may prioritize academic centers; someone already matched into radiology in the same city might choose a nearby, less intense community prelim year.
2. Geographic Priorities
Geography matters for both lifestyle and career strategy:
- Proximity to your advanced program (if already matched)
- Family or partner considerations
- Cost of living vs PGY‑1 salary
- Regions with better networking opportunities in your target specialty
Some MD graduates strategically pick a prelim IM program near academic centers where they hope to do research or where their advanced program is located. Lower cost-of-living areas may be attractive if you’re carrying significant educational debt.
3. Workload, Call Structure, and Schedule
For a preliminary medicine year, the schedule can vary significantly between programs:
Inpatient vs Outpatient Balance
Many prelim IM programs are heavily inpatient-focused with minimal clinic requirements. Review:- Number of inpatient months
- Night float vs traditional overnight call
- ICU rotations and their call schedules
Call Intensity
Even with work-hour rules, some programs are known for high-intensity ward months and frequent cross-cover. Consider:- Maximum consecutive days on service
- Weekend frequency
- Documentation support (scribes, templates, EMR efficiency)
If your advanced specialty is cognitively and procedurally demanding (e.g., neurosurgery, interventional radiology), you may prioritize a prelim program that trains you well without overwhelming burnout.
4. Educational Culture and Support
Even though it’s a one‑year position, the educational environment still matters:
- Daily teaching: morning report, noon conferences, grand rounds
- Bedside teaching and feedback
- Simulation opportunities (codes, procedures)
- Access to faculty mentors (both in IM and in your advanced specialty)
Look for signs that prelim residents are not treated as expendable extra hands but integrated into the learning environment. Review:
- Program website descriptions specifically for prelims
- Online reviews and word-of-mouth feedback
- Whether prelims attend the same conferences and didactics as categoricals
5. Role and Status of Prelim Residents at the Program
Some programs treat prelims and categoricals nearly identically; others segregate them significantly.
Ask or research:
- Do prelims carry the same patient load?
- Are prelims assigned disproportionately to less desirable rotations?
- Are prelims given access to electives?
- Are prelims included in wellness initiatives, retreats, and resident events?
For MD graduates planning future competitive applications, elective months and networking opportunities can be critical.
6. Career Development and Letter-Writing
If you’re using your prelim IM year as a bridge to a future application (reapplication or new specialty), ask:
- Are there faculty willing to mentor and advocate for you?
- Do prelims historically secure strong letters from IM faculty or subspecialists?
- Is there flexibility to do rotations in your target specialty (e.g., neurology, dermatology) or research time?
Review program alumni outcomes:
- How many prelims have successfully matched into advanced specialties or fellowships?
- Do program leaders actively support prelims in the next application cycle?
How Many Preliminary Medicine Programs Should You Apply To?
For MD graduates, the question of how many programs to apply to often generates anxiety. There’s no universal number, but we can outline practical ranges and decision rules.
1. General Ranges for MD Graduates
These numbers assume you are an MD graduate of an allopathic medical school (U.S.-trained), applying to prelim IM without major red flags.
Strong Applicant, Matched to Advanced Specialty Already
- US allopathic grad, solid USMLE/COMLEX scores, no major gaps
- Reasonable geographic flexibility
- Typical safe range: 10–20 prelim IM programs
- You can bias your list toward programs in or near your advanced specialty location.
Average Applicant with Minor Concerns
- Mid-range scores, perhaps a minor gap or a single exam failure
- Some geographic preference but some flexibility
- Typical range: 20–30 programs
Applicant with Significant Concerns or Constraints
- Multiple exam attempts, academic probation, large gaps, or strong geographic limitation
- Or requiring specific visa support with narrow regions
- Typical range: 30–40+ programs, depending on constraints
Remember: these are general guidelines, not guarantees. Your specific program selection strategy should be discussed with an advisor knowledgeable about the allopathic medical school match and current cycle competitiveness.
2. Factors That May Require You to Apply More Broadly
You should increase the number of programs if:
- You have any of the following:
- Multiple exam failures or a major professionalism concern
- Graduation >1–2 years ago with limited recent clinical experience
- Disciplinary history or leaves of absence
- You need:
- H‑1B visa sponsorship (fewer IM programs offer this)
- Strict geographic limitations (e.g., “only within 50 miles of X city”)
- You are:
- Applying late in the cycle (after many interviews are given)
- Reapplying after an unmatched year
In these cases, breadth is protective. However, it should still be smart breadth—only apply to places you would truly be willing to train.
3. When You Can Safely Apply to Fewer Programs
You may consider a smaller list (but still not tiny) if:
- You are a:
- U.S. MD graduate from a well-known allopathic medical school
- With solid Step scores (or passed on first attempt across exams)
- No gaps, strong letters, decent clinical evaluations
- You already have:
- A secured advanced position in the same geographic area
- Support from your home department with strong advocacy
Even then, it’s generally unwise to go below 10–12 prelim applications unless you have compelling data or institutional advising supporting an even smaller number.
Step-by-Step Program Selection Strategy for MD Graduates
Instead of randomly choosing programs, use a deliberate, structured program selection strategy. Below is a practical framework.
Step 1: Define Your Non-Negotiables
Start with a short list of absolute requirements. Examples:
- Must be within X distance of my advanced residency
- Must sponsor J‑1 or H‑1B visas (if applicable)
- Must be in specific regions due to family responsibilities
- Must not exceed a certain cost of living threshold
Filter programs using FREIDA, program websites, and NRMP data to create an initial master list.
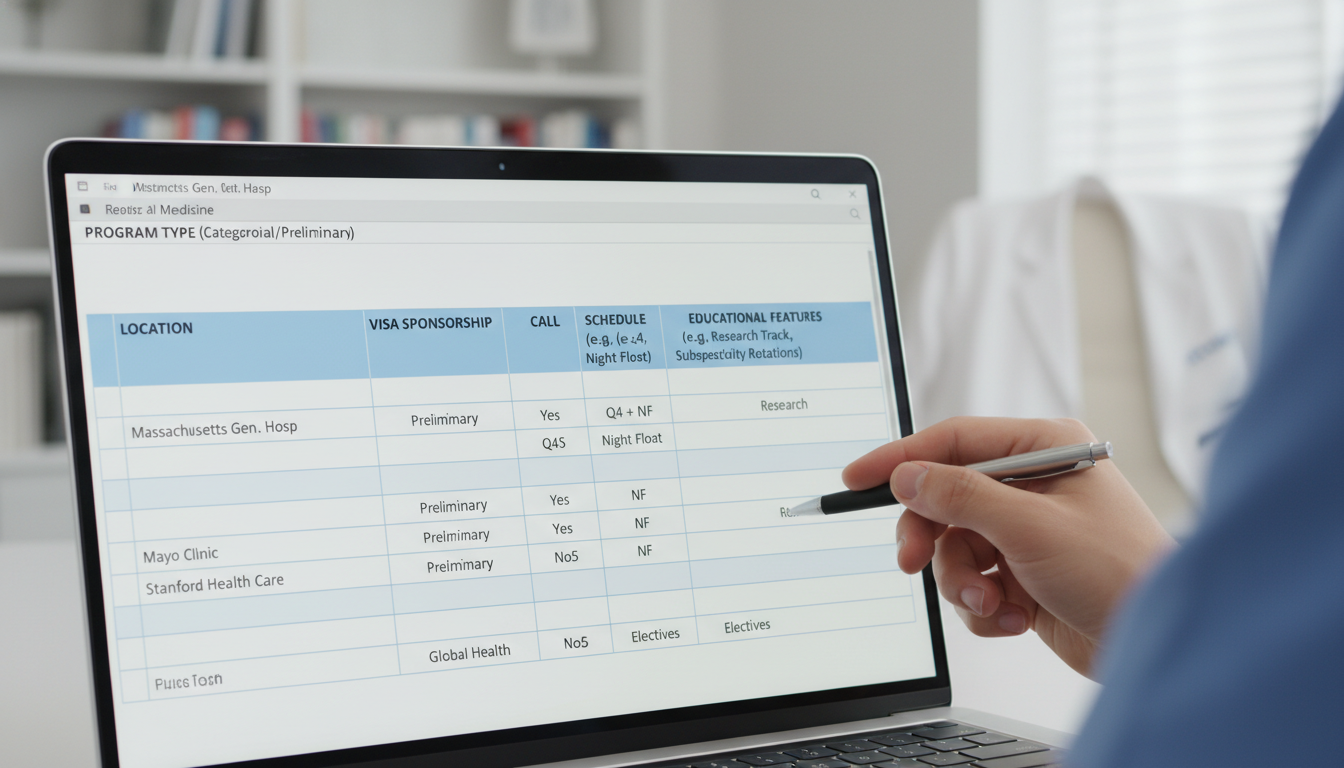
Step 2: Stratify by Program Type and Fit
Categorize each prelim IM program as:
- Academic university
- University-affiliated community
- Community, non-university
Then think about your goals:
- If you’re planning research or reapplication to a competitive field, prioritize academic or hybrid programs with:
- Research infrastructure
- Subspecialty faculty in your area of interest
- If you’re more focused on strong clinical skills and a less political environment, include more community programs with a reputation for hands-on training.
Aim for a balanced portfolio: some reach, many realistic, and some safety options.
Step 3: Research Program Culture and Prelim Experience
For each program on your shortlist:
Read the website carefully for:
- Specific sections about preliminary medicine tracks
- Sample schedules and rotation blocks
- Call/night float descriptions
- Whether elective time is offered to prelims
Seek out:
- Online forums and residency review platforms (interpret with caution)
- Alumni or senior residents from your medical school who trained or rotated there
- Program videos or resident-led virtual Q&A sessions
Key questions:
- Are prelims integrated with categoricals in teaching and social events?
- Are prelims represented in program leadership meetings?
- Do prelims have success stories published on the website or in alumni lists?
Step 4: Map Your List to Interview Probability
Programs differ in competitiveness. Estimate your chances empirically:
- Look for:
- Percentage of positions filled by U.S. MDs vs DOs vs IMGs in prior years
- Size of the prelim cohort (larger cohorts may be slightly easier to enter)
- Consider your:
- Step scores or pass/fail history
- Clinical performance and letters
- Whether you have a home or regional connection
Then categorize your target programs into:
- Likely (safety)
- Realistic (targets)
- Aspirational (reach)
Ensure you have enough likely programs to anchor your list—particularly if there are any weaknesses in your application.
Step 5: Balance Number vs Depth
Knowing how many programs to apply is not just about a raw number; it’s about how well-matched your list is to your profile.
- Too few programs + only aspirational choices → high risk of going unmatched.
- Too many indiscriminate applications → you spend time and money without strategic benefit and may be overwhelmed by interview logistics.
A refined approach:
- Start with a master list (e.g., 40–60 programs).
- Apply final filters (geography, visa, cost of living, type of program).
- Narrow to your targeted application list (e.g., 20–30), maintaining:
- ~25–40% safety
- ~40–50% realistic
- ~15–25% aspirational
Step 6: Coordinate with Your Advanced Specialty Plan
If you already have or are simultaneously applying to an advanced specialty (e.g., neurology, radiology):
- Try to align:
- Geographic regions (same city or commutable distance)
- Institutional affiliations (prelim at same hospital as advanced program when possible)
- For the allopathic medical school match, some advanced programs:
- Prefer or require you to train at certain affiliated prelim IM programs.
- Strongly recommend specific sites.
Check with:
- Current residents in your advanced specialty
- PD or APD of the advanced program
- Your medical school’s advising office
This alignment can significantly improve your continuity and networking.
Practical Examples of Program Selection Scenarios
To make all of this more concrete, consider three common MD graduate scenarios.
Scenario 1: Radiology Match with Local Preference
- U.S. MD, matched to DR at a large academic center in City A.
- No major red flags; wants a manageable but solid prelim IM experience close to City A.
Strategy:
- Focus on prelim IM programs:
- Within City A and surrounding metro area.
- University-affiliated community hospitals with good reputation.
- Apply to 10–15 programs, mostly realistic and safety-level.
- Prioritize:
- Reasonable call schedule
- Strong inpatient exposure
- Limited commute
Scenario 2: Reapplicant to Dermatology
- U.S. MD, strong research, average board scores.
- Unmatched in dermatology; wants to improve application while doing prelim IM.
Strategy:
- Emphasize prelim IM programs at academic centers with:
- Active dermatology departments
- Opportunities for research/electives in Derm
- Faculty with history of strong letter-writing
- Apply to 25–30 prelim programs across multiple states.
- Accept more intense workloads when they come with strong academic advantages.
Scenario 3: Visa-Dependent Applicant With Family Ties
- U.S.-trained MD on a visa requiring sponsorship.
- Needs to stay near family in the Midwest.
Strategy:
- Screen for:
- J‑1/H‑1B sponsoring internal medicine programs in Midwest.
- Build a list of 30–40 prelim IM programs based on:
- Sponsorship
- Acceptable commute ranges or same-city locations
- Mix of academic, hybrid, and community programs.
- Use advisors to prioritize programs that historically take visa-dependent prelims.
Common Pitfalls to Avoid in Prelim IM Program Selection
Being strategic also means avoiding mistakes that many MD graduates make.
1. Treating Prelim IM as “Any Program Will Do”
Even if your “real” specialty is something else, your prelim year:
- Shapes your clinical foundation and confidence.
- Influences your wellbeing and burnout risk.
- Can affect letters and career opportunities.
Do not apply blindly to every prelim program; vet them for educational quality and culture.
2. Ignoring the Prelim-Categorical Divide
At some institutions, prelims are:
- More service-heavy
- Less integrated in electives and research
- Lower priority for scheduling preferences
Ask directly or infer from:
- Rotation block charts
- Resident testimonials
- Interview-day questions: “How are prelim residents integrated?”
3. Overemphasizing Name Prestige
A big-name academic brand does not always guarantee:
- A humane schedule
- Supportive environment for prelims
- Time for research or reapplication
Sometimes a smaller university-affiliated community program can offer:
- Better educational support
- More direct mentorship
- More flexible scheduling for your goals
4. Miscalculating Application Numbers
Two extremes to avoid:
- Underapplying: 5–8 prelim programs with no safety options.
- Overapplying without strategy: 60+ scattered applications without geographic or program-type rationale.
Anchor your decisions with data, self-assessment, and advisor input.
FAQs: Preliminary Medicine Program Selection for MD Graduates
1. Is it better to do my preliminary medicine year at the same institution as my advanced residency?
When possible, yes, there are advantages:
- Easier transitions and onboarding (same EMR, same hospital systems).
- Earlier integration into your future department’s culture and team.
- Less moving and logistical stress.
However, it’s not mandatory. A strong prelim IM experience at a nearby or even different institution can still be excellent, especially if the call schedule and educational environment suit your needs.
2. As a U.S. allopathic MD graduate, can I safely apply to just a few prelim IM programs?
Even strong applicants should be cautious about very small numbers. While some MD graduates match with as few as 5–10 prelim applications, that’s riskier than necessary. Unless advised otherwise by a highly knowledgeable advisor with specific data about your situation, aim for at least 10–12 prelim programs, calibrated to your profile and constraints.
3. How important are letters of recommendation from my preliminary medicine year?
If you are reapplying or pivoting to another specialty, letters from your prelim year can be crucial:
- They demonstrate performance as a physician, not just a student.
- Strong evaluations from IM faculty, subspecialists, or ICU attendings can significantly strengthen your future application.
- For those already matched to an advanced program, letters may matter less for matching but can influence fellowship, academic opportunities, and future recommendations.
When choosing programs, consider whether faculty have the time and interest to mentor prelims and write detailed letters.
4. Should I prioritize programs with easier schedules or those with stronger academic reputations?
It depends on your goals and resilience. A balanced perspective:
- If you are repeating a stressful application process, you may want a program that offers both solid training and reasonable work hours to prevent burnout.
- If your main aim is to enter a super-competitive specialty or academic career, you may accept a more rigorous program that offers:
- Research time
- Strong mentors
- Significant referral weight of letters
Ideally, select programs that provide good training, educational support, and a livable workload rather than choosing solely on either extreme.
By applying this structured program selection strategy—anchored in your specific goals, realistic self-assessment, and the dynamics of the allopathic medical school match—you can build a thoughtful, targeted list of preliminary medicine year programs. For an MD graduate, this approach not only increases your chance of securing a strong prelim IM position, it also sets you up for a smoother transition into your long-term specialty and career.






















