
Understanding the Neurosurgery Residency Landscape as an MD Graduate
For an MD graduate aspiring to neurosurgery, program selection is a strategic exercise—not just a numbers game. Neurosurgery remains one of the most competitive specialties in the allopathic medical school match, with high academic expectations, long training (7+ years), and highly variable program cultures. Your program selection strategy must balance ambition with realism while maximizing your chances of matching and setting yourself up for a sustainable, fulfilling career in brain surgery residency training.
This article will walk you through how to choose residency programs in neurosurgery, how many programs to apply to, and how to build a rational program list that fits your profile as an MD graduate.
We’ll focus on:
- Understanding competitiveness and your candidacy
- Defining your personal and professional priorities
- Categorizing programs into reach/target/safety tiers
- Deciding how many programs to apply to
- Strategic use of signals, away rotations, and geographic preferences
- Practical step-by-step approach to program selection
Step 1: Assess Your Competitiveness as an MD Graduate
Before you can design a program selection strategy, you need an honest assessment of where you stand as an applicant in the neurosurgery residency landscape.
Core Competitiveness Factors in Neurosurgery
Program directors in neurosurgery residency commonly look at:
USMLE/COMLEX Performance
- Step 1 is Pass/Fail, but performance still matters indirectly (e.g., school transcript, timing of pass, narrative comments).
- Step 2 CK score remains a key numerical filter for many programs.
- For MD graduate residency applicants, Step 2 CK is often the dominant standardized metric.
Research Productivity
- Neurosurgery is research-heavy.
- Typical matched applicants have multiple publications/abstracts/posters, often in neurosurgery or neuroscience.
- Stronger candidates may have neurosurgery-specific publications, multi-institutional collaborations, and first-author work.
Letters of Recommendation (LORs)
- At least 2–3 letters from neurosurgeons are ideal (including the chair or program director at your home or away institution).
- Highly respected letter writers (e.g., department chairs, nationally recognized neurosurgeons) carry significant weight.
Clinical Performance
- Honors or high passes in surgery and neurology rotations.
- Strong neurosurgery sub-internship performance (home and/or away rotations).
- Evidence of work ethic, teamwork, and resilience.
Institutional Context
- Graduating from an allopathic medical school with a neurosurgery department often gives you more access to research, mentorship, and home sub-I opportunities.
- Coming from a school without neurosurgery is not disqualifying, but you must compensate via away rotations and networking.
Additional Distinguishers
- Advanced degrees (PhD, MPH, MS in neuroscience, etc.)
- Prestigious research fellowships or gap year(s) in neurosurgery research
- Unique skills (e.g., engineering, data science) that align with neurosurgical innovation
Self-Classification: Where Do You Fit?
To create a rational program list, first classify yourself into a rough competitiveness tier. This is not official, but it guides your program selection strategy.
Highly Competitive MD Graduate (Top Tier)
Typical features:
- Step 2 CK: Well above national mean for neurosurgery (often > 250+ range, but benchmarks vary by year)
- Research: Multiple publications in neurosurgery/neuroscience, including first-author work
- Strong letters from well-known neurosurgeons
- Honors in major clinical rotations, especially surgery and neurology
- Strong performance on neurosurgery sub-internships, possibly with outstanding comments
Solid but Not Elite Candidate (Middle/Upper-Middle Tier)
Typical features:
- Step 2 CK: Around or somewhat above the neurosurgery average
- Research: Some publications or significant ongoing projects, possibly a mix of neurosurgery and other fields
- Strong LORs from neurosurgeons, though not necessarily nationally prominent
- Good clinical evaluations; maybe mixed honors/high passes
More Vulnerable or “At-Risk” Candidate (Lower/Middle-Lower Tier)
Typical features:
- Step 2 CK: Below the average range for neurosurgery applicants
- Limited neurosurgery-specific research or delayed start in research
- Fewer neurosurgery LORs or weaker connections to academic neurosurgeons
- Inconsistencies in clinical performance or academic record
- Potential red flags (course repeats, leaves of absence, professionalism concerns) that need explanation
None of these tiers guarantees success or failure. They simply help you tailor your target list and determine how many programs to apply to.
Step 2: Define Your Priorities Before Choosing Programs
A strong program selection strategy for neurosurgery shouldn’t only chase prestige; it should match your career goals and personal needs. Before asking “how many programs to apply,” you must clarify what type of brain surgery residency environment will help you thrive.
Academic vs. Community vs. Hybrid Programs
Most neurosurgery programs are based in academic medical centers, but their structure varies:
Highly Academic/Research-Intensive Programs
- Heavy emphasis on basic/translational or clinical research
- Strong pipelines to fellowships and academic careers
- Often larger departments with multiple subspecialty services
- May expect significant scholarly productivity during residency
Clinically Focused Academic or Hybrid Programs
- Excellent operative exposure and clinical training
- Moderate research expectations—often clinical research is emphasized
- Graduates may enter private practice or academic hybrid roles
Smaller or More Regional Programs
- Often fewer residents per year
- Closer faculty-resident relationships
- May have less research infrastructure but strong operative volume
- Graduates frequently enter community or regional practice, though some still pursue academic careers
Clarify where you see yourself: do you want a research-heavy environment aligned with an academic career, or are you primarily focused on clinical excellence and operative autonomy?
Geography and Lifestyle Considerations
As an MD graduate, your geographic preferences may be a major driver. But for neurosurgery, being overly restrictive can harm your match chances.
Consider:
Must-have vs. nice-to-have locations
- Family/partner needs, visa issues (if applicable), support system
- Areas where you have strong regional ties (programs often value this)
Urban vs. Suburban vs. Smaller City
- Cost of living and lifestyle
- Commute and housing options
Training Environment
- Patient population diversity
- Trauma level and case mix (Level 1 trauma, pediatric cases, complex spine, vascular, tumor)
You do not need to apply “everywhere,” but you should avoid narrowing yourself to a small cluster of high-cost or hyper-competitive cities without strong balancing options.
Operative Volume, Case Mix, and Fellowship Prospects
For a future neurosurgeon, operative exposure and mentorship are critical. When evaluating programs:
Look for:
- Operative volume per resident, not just total departmental volume
- Exposure to all major subspecialties (vascular, skull base, spine, functional, pediatrics, neuro-oncology, trauma)
- Graduates’ career paths: academic vs. community, types of fellowships
Questions to explore from program websites, current residents, or mentors:
- Are there fellows who may compete with residents for cases, or do they enhance teaching and case volume?
- Is there protected research time (e.g., 1–2 dedicated research years)?
- How is call structure managed, and what support do residents have?
Culture, Mentorship, and Wellness
Neurosurgery is demanding. Program culture and mentorship quality are as important as prestige.
Look into:
- Resident retention and attrition rates
- Reputation regarding resident support vs. burnout
- Diversity and inclusion efforts
- Availability of formal mentoring, career development, and wellness resources
Use your sub-internships/away rotations to directly sample culture. This should meaningfully influence your eventual rank list and even your initial program selection.
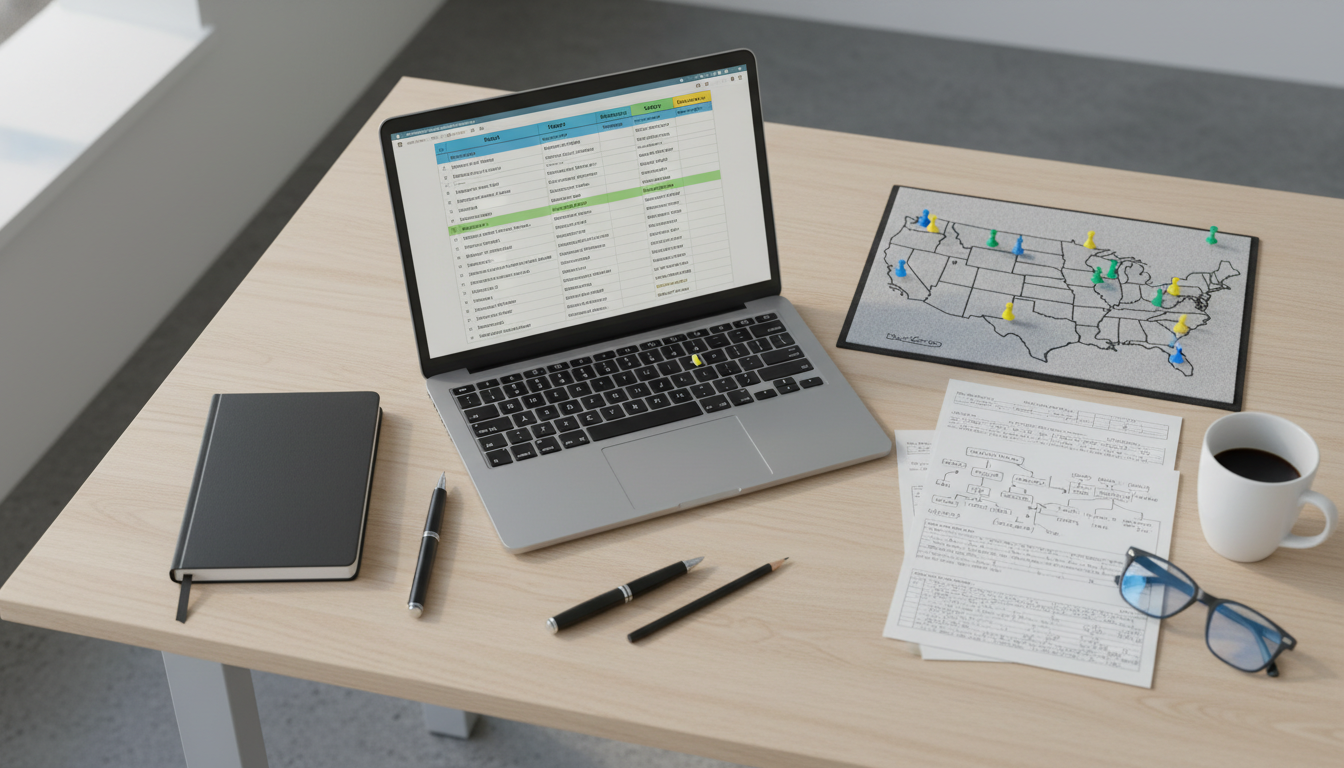
Step 3: Categorize Programs into Reach, Target, and Safety Tiers
Once you understand your competitiveness and priorities, the next step in your program selection strategy is building a balanced list of programs.
Building Your Initial Universe of Programs
Start broadly, then narrow:
Compile a master list of all ACGME-accredited neurosurgery residencies (from FREIDA, SF Match/NRMP data, or specialty society lists).
Filter by absolute constraints:
- Programs that don’t sponsor visas (if you need one)
- Locations you truly cannot live in (rare but valid)
- Programs without required pediatric or subspecialty exposure (if that’s essential to you)
Screen for alignment with your goals:
- Programs with strong research if you want an academic track
- Programs with recognized strengths in your area of interest (e.g., functional neurosurgery, spine, vascular)
- Geographic clusters where you have ties
Defining Tiers for Neurosurgery Programs
Your tiers are not official rankings; they’re a way to structure risk.
Reach Programs
- Historically match applicants with very strong metrics and research
- Often big-name academic centers, nationally known for neurosurgery
- You may be “within range” but not strongly competitive, or they may just be extremely selective for everyone
Target Programs
- Your Step 2 CK, research, and clinical record are clearly within or slightly above their typical matched profile
- Strong chance at interview if your application is well-prepared
- Mix of academic and hybrid programs that fit your goals
Safety (or “Safer”) Programs
- Programs where your metrics and experiences are clearly above their historical averages, or
- Programs in less popular geographic areas, smaller cities, or newer residencies that may attract fewer applicants
- Still fully capable of training excellent neurosurgeons, but potentially less brand recognition
Note: In neurosurgery, there are no “guaranteed safety” programs; all are competitive. “Safety” here is relative.
Example of Tiering for a Hypothetical Applicant
Imagine you’re an MD graduate with:
- Step 2 CK in the mid-240s
- 3 neurosurgery-related publications
- 2 neurosurgery away rotations with strong evaluations
- Solid LORs from known but not “celebrity” neurosurgeons
Your list might look like:
Reach (25–30%):
- Top-tier academic centers with very high research reputation and large applicant pools.
Target (40–50%):
- Mid- to high-level academic programs where your scores/research are well-aligned; strong clinical training with moderate research emphasis.
Safety (20–30%):
- Solid training programs in less popular cities or newer programs where your profile is more competitive than average.
This proportional approach helps avoid lists composed only of hyper-competitive institutions while still pushing for aspirational programs.
Step 4: How Many Neurosurgery Programs Should You Apply To?
This is the central question for many MD graduate residency applicants: how many programs to apply for neurosurgery?
General Numerical Ranges
Exact numbers change over time, but for neurosurgery—a low-N specialty with limited positions per program—most fully committed MD graduates will apply broadly.
Reasonable ranges for a typical MD graduate:
Highly competitive applicants
- Often apply to 25–40 programs
- May aim for more selective institutions with fewer “safer” backups, but still maintain diversity
Solid but not elite applicants
- Commonly apply to 40–60 programs
- Balanced mix of reach, target, and safer programs across different regions
At-risk or more vulnerable applicants
- May consider 60–80+ programs
- Particularly if they lack home neurosurgery programs, have weaker Step 2 scores, or limited research
- Still must be targeted—blanket applications without alignment are less helpful
The exact number for you depends on:
- Your competitiveness tier
- Your geographic flexibility
- The strength of your neurosurgery exposure and letters
- Whether you’re applying with a prior unsuccessful match attempt
Avoiding Two Common Extremes
Too Few Applications
- Applying to 10–15 programs, even if they are strong, is usually very risky in neurosurgery.
- The small cohort size and high variability in interview offers can easily leave qualified applicants unmatched.
Too Many “Random” Applications
- Applying to nearly every program without considering fit or feasibility can be:
- Financially costly
- Logistically overwhelming for interview season
- Less effective than a curated list aligned with your profile and goals
- Applying to nearly every program without considering fit or feasibility can be:
A thoughtful strategy is better than brute-force volume.
Matching Application Volume to Your Profile
Combine tiers and numbers:
Top-tier candidate:
- 10–15 reach, 10–20 target, ~5 safer programs
- Total: ~25–40
Middle-tier candidate:
- 10–15 reach, 20–30 target, 10–15 safer
- Total: ~40–60
Lower-tier/at-risk candidate:
- 10–20 reach (still worth some applications), 20–30 target, 20–30 safer
- Total: ~60–80+
Adjust based on:
- Feedback from neurosurgery mentors and your home PD
- Your financial and time capacity for interview travel (or virtual interviews)
- Any limitations (visa, family, serious location constraints)
Step 5: Advanced Program Selection Strategy Elements
Beyond raw numbers, nuanced tactics can strengthen your neurosurgery residency application strategy.
Strategically Using Away Rotations and Signals
In neurosurgery, sub-internships/away rotations are effectively month-long auditions:
- Use away rotations to:
- Showcase work ethic, teachability, and team compatibility
- Obtain strong letters specific to neurosurgery
- Clarify whether a program’s culture and volume fit your needs
These rotations should:
- Align with regions or programs you could realistically match at
- Include at least one “reach” and one “target/safety” program, if possible
If the ERAS or specialty system uses program signals or priority rankings in future cycles:
- Use signals for programs where:
- You’ve done an away rotation or have strong ties
- You are a strong fit but might otherwise be overlooked due to geography or profile
Geographic Clustering Strategy
Instead of scattering your applications across dozens of random locations, consider geographic clusters:
- Identify 2–4 major regions where you’d be happy to train (e.g., Northeast, Midwest, Southeast, West Coast).
- Apply to a mix of reach/target/safety programs within each cluster.
- Benefits:
- Increases the chance of multiple interviews in the same region.
- Reduces travel costs and logistical complexity.
- Shows plausible regional commitment, which some programs value.
Evaluating Programs Beyond Websites
Program websites are often aspirational and may not fully reflect day-to-day reality. To refine your list:
Talk to current residents:
- Ask about operative autonomy at different PGY levels
- Ask how often fellows do cases instead of residents
- Ask about burnout, wellness, and faculty support
Leverage mentors:
- Neurosurgery faculty at your home or away institutions can give unfiltered insight into program reputations, strengths, and weaknesses.
- Ask: “Given my application, which programs would you consider my targets and safeties?”
Look at graduates’ outcomes:
- Fellowship placements
- Types of practices they enter
- Academic vs. private practice balance
Adjusting Your List in Real Time
Your program selection strategy doesn’t end once you hit submit:
If you receive significantly fewer interviews than expected:
- Reassess your competitiveness and seek early feedback.
- Consider supplemental applications, if available.
- Strengthen your application for a potential reapplication if needed (research year, more neurosurgery exposure).
If you receive more interviews than you can handle:
- Prioritize:
- Programs that align best with your long-term goals
- Locations where you’d realistically rank highly
- Institutions where you have strong mentorship opportunities
- Prioritize:
Remember: the end goal is not just to match, but to match into a neurosurgery residency that fits your career aspirations and will support you through an intense, demanding training process.
Putting It All Together: A Practical Step-by-Step Plan
Here is a concise workflow for MD graduates developing a program selection strategy for neurosurgery:
Self-Assessment (Early MS4 / Pre-Application)
- Review Step 2 CK, research output, clinical performance, and letters.
- Meet with neurosurgery mentors for honest feedback.
Clarify Goals and Constraints
- Decide on academic vs. clinically focused trajectory.
- Outline geographic must-haves and flexibilities.
- Consider lifestyle, family, and financial factors.
Build a Master List
- Include all neurosurgery programs you might consider.
- Eliminate those that fail hard constraints (visa, absolute location no-go, etc.).
Tier Programs
- Classify each as reach, target, or safety based on your profile and mentor input.
- Ensure a balanced distribution.
Decide Application Volume
- Choose a total range (e.g., 40–60) based on your competitiveness.
- Make sure each tier is represented (e.g., 30–40% target, 20–30% reach, 20–40% safer).
Integrate Away Rotations and Signals
- Prioritize programs where you rotated or have ties.
- Allocate signals (if available) to your highest-priority and best-fit programs.
Refine with Extra Information
- Talk to residents and mentors about specific programs.
- Adjust list before final submission if you discover misalignment.
Monitor and Adapt
- Track interview offers by tier and region.
- If needed, consult mentors about how to re-strategize—either within the current cycle (e.g., interview prioritization) or for a future reapplication.
By treating neurosurgery program selection as a structured, data-informed process rather than a guesswork exercise, you significantly improve both your chances of matching and the likelihood that you end up in a residency that truly fits you.
FAQs: Program Selection Strategy for MD Graduates in Neurosurgery
1. As an MD graduate, is it harder or easier to match into neurosurgery compared with DO or IMG applicants?
Neurosurgery programs in the allopathic medical school match historically favor MD graduate residency applicants, especially from US allopathic schools, largely because of familiarity with curricula and established research pathways. This does not guarantee success, but as a US MD graduate you generally start with a relative advantage over DO or IMG applicants—particularly if you have neurosurgery exposure and research. That said, competition remains intense, and your individual profile (scores, research, letters, performance on sub-internships) still matters far more than degree type alone.
2. How important is research when choosing neurosurgery programs to apply to?
Research is critical in neurosurgery, but the type and emphasis of research vary by program. If you have strong research and want an academic career, target programs with dedicated research years, NIH funding, and strong basic science or clinical research infrastructure. If your interest is primarily clinical, you can still apply broadly but might prioritize programs where research expectations are more clinically oriented and integrated into patient care. Aligning your research profile with a program’s culture makes your application more compelling and can guide which programs you classify as reach, target, or safety.
3. Should I avoid applying to “top-tier” neurosurgery programs if my Step 2 CK is below 240?
Not necessarily. It’s reasonable to include some high-profile programs as reach choices, particularly if you have compensating strengths—such as substantial neurosurgery research, excellent sub-internship performance, or powerful letters from well-known neurosurgeons. However, you should not build your entire list around these programs. For a lower Step 2 CK, your program selection strategy should emphasize a robust set of target and safer programs where your overall profile is well-aligned, and where you can realistically secure interviews.
4. If I don’t match, how should I adjust my program selection strategy for the next cycle?
If you go unmatched in neurosurgery, first debrief with neurosurgery mentors and, if possible, program directors who can offer specific feedback. Common next steps include:
- Completing a dedicated neurosurgery or neuroscience research year
- Strengthening your neurosurgery exposure and obtaining new letters
- Broadening geographic flexibility and adding more target/safety programs
- Applying to a greater total number of programs (often in the 60–80+ range)
In the next cycle, your program selection strategy should be more conservative and data-driven, with intense focus on alignment and realistic tiers, while continuing to include a small number of reach programs that fit your improved profile.
A deliberate, evidence-based approach to choosing neurosurgery residency programs—grounded in honest self-assessment, clear priorities, and a structured application plan—will help you navigate one of the most competitive specialties in the allopathic medical school match and increase your chances of launching a successful brain surgery residency career.






















