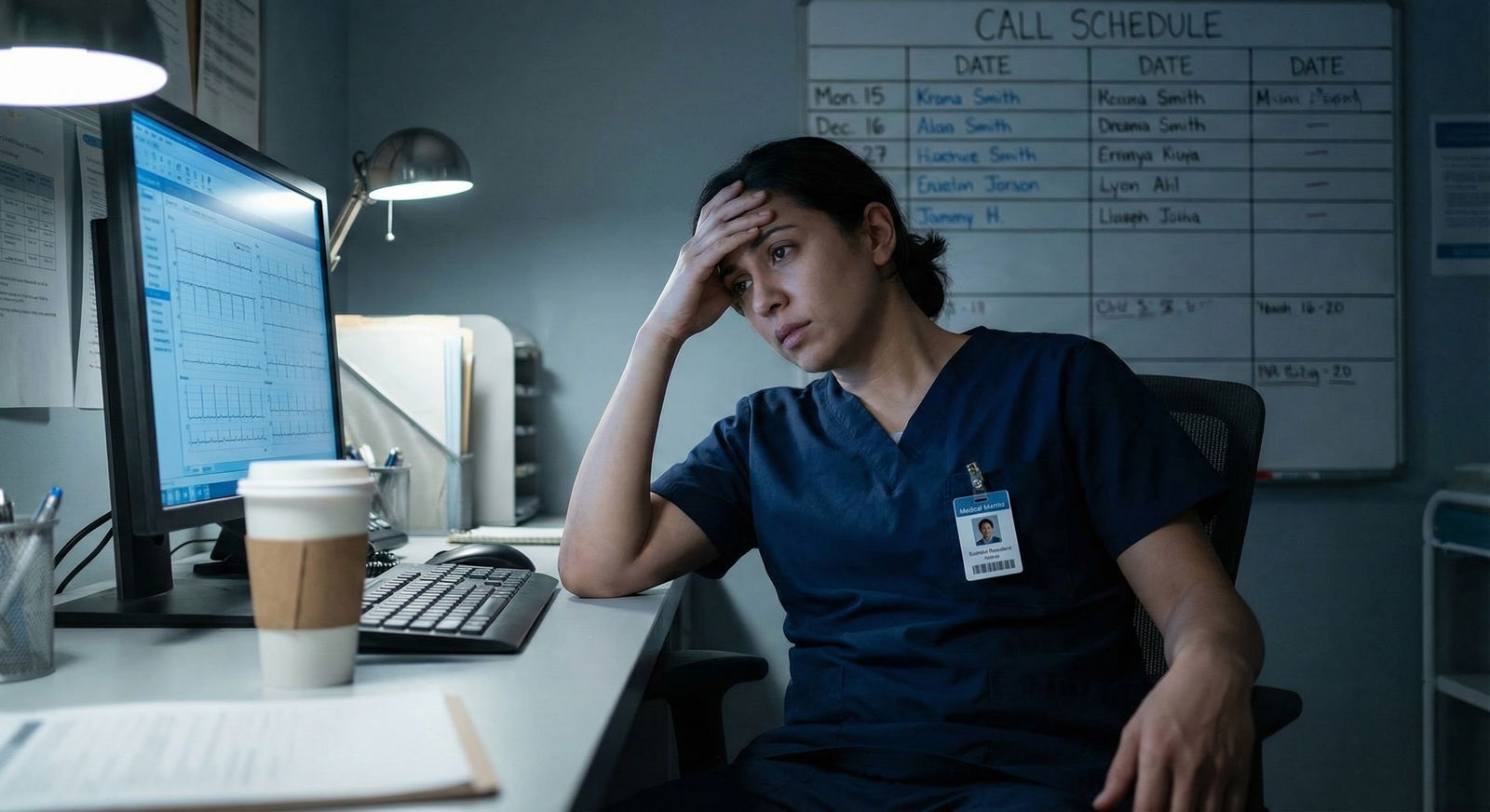
It’s March. You’re in the call room between pages, scrolling through your email. Results are out. You already know it’s bad before you even open NRMP. “You did not match to any position.” Your stomach drops. You’ve been working 70–80 hours a week as a prelim, you’ve done “everything right,” and somehow you’re looking at no job for July.
Everyone around you is talking about their PGY‑2 plans, new cities, new apartments. You’re secretly googling “what to do if unmatched after prelim year” on your phone between consults. You feel embarrassed, angry, and—honestly—terrified.
This is where you are.
Here’s how to get from “this is a dead end” to “I have a new, concrete path.”
Step 1: Stabilize the Next 4–6 Weeks (While You’re Still a Prelim)
First priority isn’t your five‑year career plan. It’s the next month. You’re still an employee, under contract, and how you finish this year will follow you.
A. Protect your references right now
Today or tomorrow, you email or talk in person with:
- Your program director
- Your associate program director (if applicable)
- One or two attendings who actually know your work
Script (adapt it, but keep the bones):
“Dr. X, I wanted to let you know directly that I did not match into a PGY‑2 position. I’m disappointed, but I’m committed to finishing this year strong and taking a thoughtful next step. I’d really value your honest feedback on my application and your advice on next options. I also hope I can count on you for a letter if I reapply or pursue another pathway.”
Do not disappear. Don’t start checking out. PDs remember who kept showing up after bad news.
B. Get the unfiltered truth
You need to know why you did not match. Not your guess. The actual perception from people who see hundreds of applications.
Ask your PD directly:
- “If you saw my application as another PD, what would you think is the main red flag?”
- “Would you re-rank me if I reapplied here for a categorical next year?”
- “If not, what would I need to change to become rankable?”
If multiple faculty say the same thing—Step score, professionalism concern, weak letters, too competitive a specialty—you treat that as fact, not opinion.
Write it down. This becomes your problem list.
Step 2: Define Your Realistic Option Set
You have more options than “reapply same thing or quit medicine.” But not all options are good for you.
Let’s classify where you stand.
| Profile | Typical Situation |
|---|---|
| Competitive Specialty Try | Prelim medicine/surgery after applying to derm, ortho, etc. |
| Step/Clinical Red Flag | Low Step, fail, or professionalism issue; did prelim IM/Transitional |
| Visa/IMG Barrier | Strong prelim year but limited by visa or IMG status |
| Geographically Rigid | Only applied to one region or small number of programs |
| Burnout/Misfit | Realize current specialty is not a good long-term fit |
Your path depends which box you’re mostly in.
A. Reapply to the same specialty vs. switch
Blunt truth:
If you went for a hyper‑competitive field (derm, plastics, ortho, ENT, rad onc) and couldn’t land a PGY‑2 after a solid prelim year, the odds next cycle are usually worse, not better—unless you significantly change something (dedicated research year with real output, new letters from big names, different geographic strategy).
If you applied IM, FM, psych, peds and still didn’t match, something major is off:
- Application strategy obviously poor (too few programs, terrible personal statement, obvious red flag not addressed)
- Or your record has a serious issue (Step failure, professionalism, repeated leaves of absence, very bad letters)
In both situations, you should seriously consider:
“Would I rather be in a less competitive specialty as a practicing physician, or outside of clinical medicine entirely?”
That’s not a soft question. That’s the pivot point.
Step 3: Decide: Short-Term Bridge vs. Immediate Reapply
Your prelim year ends in June. Your goal is to not be unemployed and clinically stale on July 1.
You’ve got three main short‑term structures:
- Second Prelim Year (Same or Different Program)
- Research/Non‑ACGME Clinical Job (e.g., hospitalist extender)
- Nonclinical Gap With a Plan (rarely ideal, sometimes necessary)
Let’s go through each.
1. Second prelim year
When it makes sense:
- You’re an IMG or visa-limited and need more US experience and letters.
- Your first prelim was at a high‑power place where you didn’t stand out; a smaller community prelim could give you a PD who can really advocate for you.
- You had some performance issues early that improved later; a “clean” second year can reset perceptions.
When it’s a trap:
- Same program. Zero plan. PD says vague things like “We’ll see next year” but won’t commit to ranking you or supporting a different specialty.
- You’re burned out and already hate this environment. Doubling down will make everything worse—and your evaluations might suffer.
Q to ask your PD before you agree:
- “If I do a second prelim here and perform well, would you support me strongly for IM/FM/another field?”
- “Have you successfully helped someone in my position match before? What did they do differently?”
If they can’t or won’t answer clearly, don’t rely on that program to save you.
2. Research or non‑ACGME clinical job
This can be a lifesaver if done right.
Types of roles:
- Research fellow in your specialty (or a related one you’d accept long‑term)
- Hospitalist extender / Inpatient clinician under attending supervision (common in some community hospitals, especially for IM)
- Postdoctoral clinical research roles that still keep you close to patient care

| Category | Value |
|---|---|
| Second Prelim | 35 |
| Research/Clinical Job | 40 |
| Switch to Different Specialty | 20 |
| Left Clinical Path | 5 |
Good signs a research year will actually help:
- You’re at or can move to an institution where your research PI is tight with PDs in your target field.
- You’ll be writing, presenting, and getting your name on papers—not just data cleaning in a basement.
- The job allows ongoing clinical contact (BP checks on study patients, shadowing, etc.) so you aren’t clinically rusty.
Red flag version:
- “Research job” that’s actually unpaid, unguided, and not tied to anyone known.
- You’re doing random QI projects nobody cares about.
- No one is talking to you about letters and advocacy from day 1.
If you go this route, you treat it as a professional campaign:
- Month 1–2: Learn the environment, find 1–2 strong mentors.
- Month 3–6: Get at least one meaningful project leading to a poster or manuscript.
- Month 6–9: PDs in your desired field know your name and have seen your work ethic.
- Month 9–12: Strong letters + updated CV + targeted application round.
3. Nonclinical gap (and when it’s not career suicide)
I’ve seen people take a nonclinical year and still match. But they did it the right way:
- They framed it clearly: family illness, health, immigration, or clear career reassessment.
- They volunteered clinically, kept some degree of patient exposure, and lined up at least one US physician who could still vouch for their skills.
- They didn’t hide it; they explained it.
If you’re considering stepping out completely for a year, ask yourself:
- Will I realistically come back to 60–80 hour weeks?
- Can I maintain some clinical relevance—volunteer clinic, telehealth scribe, etc.?
- Will this time resolve the problem that led to not matching?
If the answer to all three is no, pausing might just become quitting in slow motion.
Step 4: If You Reapply – How to Make This Cycle Different
Reapplying with the same strategy is just repetition, not resilience. You need a different playbook.
A. Expand or change your specialty target
Here’s the conversation I make people have with themselves:
“Would I rather be a practicing physician in a less glamorous specialty, or never be a practicing physician at all?”
If the answer is “I must be ortho or nothing,” then stop pretending you want options. Accept the gamble.
If the answer is “I just want a meaningful clinical career,” widen the door:
- Strong prelim IM → consider IM, FM, psych, prelim→anesth in some settings.
- Prelim surgery → consider categorical gen surg at smaller programs, or switch to anesthesia, radiology (if scores strong), or FM with procedural focus.
- IMG with visa issues → apply broadly to IM/FM/psych in visa‑friendly regions, not just coastal academic centers.
| Situation | Old Strategy | New Strategy |
|---|---|---|
| Prelim IM, ortho applicant | 60 ortho programs only | 25 ortho + 80 IM/FM |
| IMG, low Step, psych | 40 psych university | 120 psych+FM, mostly community |
| US‑grad, fail Step 1 | 30 mid-tier IM | 120 IM/FM in multiple states |
B. Fix the application content itself
You know the lazy advice: “Get good letters, improve your personal statement.” Here’s what that actually means.
Letters
- You want at least one letter that explicitly says:
“I have worked with Dr. X as a prelim resident and would be happy to have them in our own categorical program.” - If your current PD cannot or will not say something like that, that’s a problem—and you need letters from attendings who can use that level of language.
- You want at least one letter that explicitly says:
Personal statement
You’re not a med student anymore. You have evidence.Do not write: “I am passionate about internal medicine.”
Do write: “During my preliminary year at [Hospital], I managed X, Y, Z-level responsibilities and discovered I am most fulfilled by [___]. This experience confirmed that I am best suited to [specialty] because [specific, grounded reasons].”Also, own the reapplication directly in one paragraph. Something along:
“I applied previously to [specialty/path]. While I did not match to a PGY‑2 position, my preliminary year clarified that my strengths and long‑term interests align better with [new specialty OR same specialty with refined focus]. With faculty feedback, I have focused on [concrete improvements: clinical performance, exams, research] and am applying this cycle with a clearer, more realistic path.”
Red flag explanation
If you have a Step failure, LOA, or professionalism issue, script it, get it tight, and stick to it. No rambling, no blaming.
Step 5: Use Time Left in Your Prelim Year Strategically
You’re still in a residency. That’s leverage.
Here’s how to use the next few months.
A. Target rotations and relationships
You want to finish with:
- 2–3 attendings who will go to bat for you
- A PD who, even if they can’t keep you, will pick up the phone for you
- Clear evidence of improvement if you had any rough evals early
Practical moves:
- Volunteer for admissions or consult-heavy rotations where you can show judgment and work ethic.
- Ask to rotate in or shadow the specialty you’re pivoting to (e.g., switch from surgery to anesthesia → ask for anesthesia elective).
- Tell those attendings early: “I am exploring [specialty]. I’d like feedback on whether you think I’d be a good fit and, if so, help with a letter down the line.”

| Step | Description |
|---|---|
| Step 1 | Now |
| Step 2 | Meet PD & key attendings |
| Step 3 | Clarify red flags & goals |
| Step 4 | Choose next-year plan |
| Step 5 | Target high-yield rotations |
| Step 6 | Secure strong letters |
| Step 7 | Prepare new application |
B. Clean your record
If you had:
- Tardiness issues
- Chart completion problems
- Communication complaints
You can’t erase them, but you can bury them under months of good performance.
Tell your chief or PD:
“I know I had some issues early with [X]. I want you to know I’m actively working on it. If there’s anything else I can do in the last months to show reliability, I’m open to feedback.”
That sounds corny, but it changes how they talk about you on the phone.
Step 6: Consider Alternative Long-Term Clinical Paths
Sometimes, the reality is: categorical residency in the US in your desired specialty is unlikely. Still doesn’t mean “no medical career at all.”
Real options I’ve seen people take:
Switch to a less competitive specialty
- FM, psych, neurology, pathology, PM&R, sometimes anesthesia or radiology from a strong prelim base.
- Yes, ego will scream. But many people are happier five years later than they expected.
Return to home country / different system
- For some IMGs, moving back home, finishing training, then coming back to the US in a different capacity (hospitalist, fellowship, etc.) ended up being more realistic.
Non‑traditional medical careers
- Clinical research management
- Pharma (medical science liaison)
- Health tech, clinical informatics roles (especially if you’re tech‑inclined)
Those require some networking and repositioning—but your MD and prelim year aren’t wasted.

| Category | Value |
|---|---|
| Matched Different Specialty | 40 |
| Matched Same Specialty Later | 15 |
| Practicing Abroad | 20 |
| Nonclinical Medical Career | 25 |
Step 7: Fix the Psychological Part (Or It Will Sink You)
Being unmatched after working as a resident feels worse than not matching straight from med school. You’re watching co‑interns move on while you hit pause. If you don’t deal with the headspace, it leaks into everything: interviews, emails, the way you talk to PDs.
A few blunt points:
- Do not isolate. At least one person in your life—mentor, co‑resident, therapist—should know the full situation.
- You are not “the prelim who failed.” You are someone who tried a path, hit a wall, and is now deciding the next one. That’s it.
- PDs don’t actually care that you feel ashamed. They care whether you have a plan, insight, and stamina.
If you’re struggling, consider:
- Short‑term therapy or counseling through your GME office or employee health.
- Structured journaling: what actually went wrong, what’s in your control, what isn’t. Sounds cheesy, but clarity reduces panic.
- One written page: “If I fully commit to Plan A, and it doesn’t work, my Plan B and C are ___.” Having that on paper calms the catastrophic thinking.

Step 8: Concrete 30-Day Action Plan
Let’s put this into a simple 30‑day sprint.
Week 1–2:
- Meet PD + 2–3 key attendings. Get hard feedback. Ask explicitly for future letter support.
- Decide primary direction: reapply same specialty, switch, or seek second prelim vs research.
Week 2–4:
- If aiming for research/clinical job: start emailing PIs/programs now. These things move slowly, and positions get snatched quickly.
- Request copies of your evaluations; look at patterns.
- Draft the first version of your “I didn’t match” explanation—2–3 sentences you can use on the phone, in emails, and in interviews.
Week 3–4:
- Target electives for the rest of your prelim year that align with your new plan.
- Schedule at least one check‑in with someone outside your program (med school advisor, mentor) who isn’t politically tied to your current PD.

| Step | Description |
|---|---|
| Step 1 | Unmatched Result |
| Step 2 | Week 1: Meet PD & Attendings |
| Step 3 | Decide Primary Direction |
| Step 4 | Week 2: Contact Research/Job Leads |
| Step 5 | Review Evaluations & Patterns |
| Step 6 | Week 3: Draft Explanation & PS Outline |
| Step 7 | Week 4: Align Remaining Rotations & Mentors |
FAQ (Exactly 4 Questions)
1. Should I tell my co‑residents and attendings that I did not match, or keep it quiet?
Tell the people whose help you need; you don’t owe the whole program your story. Your PD, APD, and specific attendings you want letters from should know—and they should hear it from you, not the grapevine. For peers, share selectively with those you trust. Oversharing can invite unhelpful commentary; total secrecy cuts you off from support and opportunities.
2. Is doing a second prelim year a bad idea?
It depends. A second prelim can make sense if it clearly changes your positioning—new PD, better letters, more responsibility, stronger performance after early issues, especially for IMGs or visa holders. It’s a bad idea if it’s just “buying time” with no change in environment, mentorship, or strategy. Before agreeing, ask any prospective PD how they’ve helped previous prelims in your situation match and what they expect you to improve.
3. How do I explain being unmatched in future interviews without sounding defensive?
Keep it short, factual, and forward‑looking. For example: “I applied primarily to [specialty/program type] with a narrower strategy than I should have, and I did not match. My prelim year helped me identify [specific strengths] and also showed me that [current target specialty] is a better fit. Since then, I’ve focused on [concrete improvements], and the feedback from my current faculty has been very positive.” No blaming the system, no long story. Own your part, show insight, then pivot to what you’ve done since.
4. Does being unmatched after a prelim year permanently damage my chances?
It’s a hit, yes—but not an automatic death sentence. Programs will wonder why it happened. If you keep working clinically, get strong letters from your prelim year, and apply more strategically (often to a broader or less competitive field), many people do match on a later attempt. The ones who really struggle are those who: disappear from clinical work, don’t address the underlying issue (exam, professionalism, unrealistic specialty choice), or reapply with the same weak application. Your job is to make sure you’re not in that group.
Key takeaways:
- Do not disappear—finish your prelim year strong and cultivate PD/attending advocates now.
- Choose a realistic next step (second prelim, research/clinical job, or specialty switch) that actually changes your odds, not just burns time.
- Reapply with a different strategy, clean explanation, and demonstrable growth—or consciously pivot to an alternative medical path you can live with.






















