
Understanding Why Case Volume Matters So Much in Cardiothoracic Surgery
For a non-US citizen IMG interested in cardiothoracic surgery residency, case volume is not just a statistic—it is one of the most powerful predictors of your technical growth, confidence in the operating room, and eventual employability. Cardiothoracic surgery is a high‑risk, technically demanding field where tactile skills, pattern recognition, and intraoperative judgment are built through repetition. That repetition shows up in the numbers: residency case volume, surgical volume, and specific procedure numbers.
As a foreign national medical graduate, you often face additional obstacles—visa restrictions, perception bias, and limited networking opportunities—so choosing a training environment where you can log robust case numbers is especially critical. High volume can partially offset these barriers by giving you:
- Stronger objective credentials: case logs, case mix, and complexity
- More competitive fellowship/job applications
- Greater comfort handling complex cardiac and thoracic pathology
- A clearer story to tell in interviews: “I’ve done X CABGs, Y valve cases, and Z thoracic procedures independently by graduation.”
This article explains how to evaluate case volume in cardiothoracic surgery residency programs specifically from the perspective of a non-US citizen IMG, and what practical steps you can take to obtain the most accurate information before you commit to a program.
Core Concepts: What “Case Volume” Really Means in CT Surgery
Before comparing programs, it’s essential to understand what exactly you’re evaluating. Case volume is more nuanced than a single number.
1. Total Case Volume vs. Individual Resident Volume
Total program volume
How many cardiothoracic cases (cardiac + thoracic + congenital, where applicable) are performed at the institution annually. Example:- Program A: 2,000 adult cardiac + 800 thoracic cases per year
- Program B: 800 adult cardiac + 300 thoracic cases per year
Per-resident volume
The more meaningful metric: how many primary surgeon or first assistant cases each resident logs over the course of training. A high-volume hospital with too many trainees can dilute your operative exposure.
Action point: When you see an impressive institutional volume, always ask:
“How is that distributed among trainees, and what is the average case number per graduating resident?”
2. Case Mix and Complexity
Pure volume isn’t enough. A strong cardiothoracic surgery residency should include diversity in:
- Cardiac: CABG, isolated valve, combined valve/CABG, aortic surgery, heart failure/VAD, transplant (where available)
- Thoracic: lobectomies, pneumonectomies, minimally invasive (VATS, robotic), esophageal surgery
- Approaches: open sternotomy, minimally invasive cardiac, robotic thoracic, transcatheter procedures (TAVR, TEVAR as adjunct exposure)
For a non-US citizen IMG, having exposure to advanced or complex procedures (e.g., aortic arch surgery, transplant, minimally invasive valves) can differentiate you significantly in job or fellowship applications, especially if visa status might be perceived as a disadvantage.
3. Role in the Case: Observer vs. Operator
When evaluating case volume, distinguish between:
- Observer/scrubbed but not operating
- First assistant without primary responsibility
- Primary surgeon under direct supervision
Programs vary dramatically in how quickly they let residents “drive” the operation. For your eventual competence and confidence, primary surgeon numbers matter more than just being present in the OR.
Important nuance for IMGs: In some programs, non-US citizen IMGs may initially be given fewer opportunities to lead Cardiac cases until they have proven themselves. You need to know how quickly and reliably opportunities increase once you demonstrate competency.

Benchmarks and Numbers: What Is “Good” Case Volume?
To evaluate programs intelligently, you need a frame of reference. While requirements and averages change over time, several principles are relatively stable.
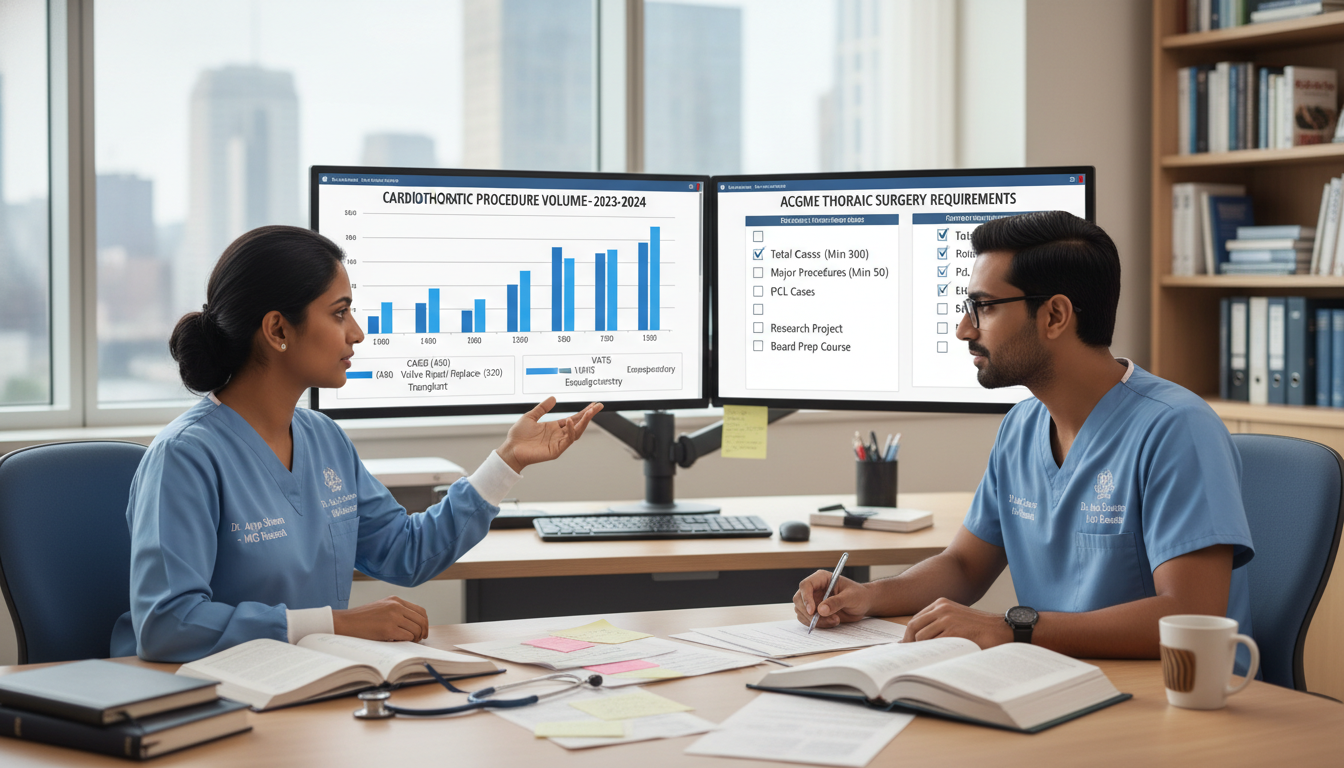
1. ACGME Minimum Requirements (Conceptual Overview)
The ACGME sets minimum case numbers for cardiothoracic surgery residents (integrated and traditional tracks). While exact numeric standards evolve, they typically include:
- A minimum number of adult cardiac operations (CABG, valves, aortic)
- A minimum number of general thoracic operations (lung resections, esophageal surgery, other thoracic procedures)
- Defined numbers where the resident acts as primary surgeon
You should look for programs where graduates far exceed the minimums—not just barely meet them. Barely meeting ACGME requirements can signal bottlenecks in operative experience.
2. What Strong Programs Commonly Produce (Approximate Ranges)
Program strength can often (though not always) be inferred from the procedure numbers logged by graduating residents. Examples of healthy ranges to look for:
Adult Cardiac (as primary surgeon by graduation)
- CABG: 100–200+
- Valves (AVR, MVR, TVR/repair): 80–150+
- Aortic procedures: 20–50+ (including ascending, root, sometimes arch)
General Thoracic
- Anatomic lung resections (lobectomy, segmentectomy, pneumonectomy): 60–100+
- Minimally invasive VATS/robotic lung resections: 30–60+
- Esophageal surgery: 15–30+
These are approximate comfort zones, not strict rules. Some high-quality programs may skew more cardiac or more thoracic, but you should be wary if the numbers are persistently close to the bare minimum.
3. Independent vs. Integrated Pathways
As a non-US citizen IMG, you may be applying to:
- Integrated (I-6) cardiothoracic surgery residency: 6-year continuous training after medical school.
- Traditional or Independent pathway: 2–3 years after general surgery training.
Case volume expectations differ:
- Integrated residents build CT experience over more years; early on, thoracic and cardiac cases are often more observational/assist roles, ramping to higher primary surgeon volume in later years.
- Independent residents must achieve high primary surgeon numbers in a shorter interval; they should have solid general surgery operative skills that transfer.
When evaluating your competitive position as a foreign national medical graduate, consider which pathway realistically offers you better access to the necessary surgical volume and autonomy given your prior training.
How Non-US Citizen IMGs Should Evaluate Case Volume Before Ranking Programs
You will rarely find a single spreadsheet online that perfectly answers your questions. Instead, you need a deliberate strategy to gather and synthesize multiple data points.
1. Use Public Data Sources as a Starting Point
Several sources provide a general sense of heart surgery training volume:
Program websites
Many cardiothoracic surgery programs list:- Annual adult cardiac and thoracic case numbers
- Clinical sites and distribution (VA, university hospital, private partners)
- Types of complex procedures performed (transplant, LVAD, aortic, robotics)
Hospital/system quality metrics
Look for:- CABG volumes
- Valve surgery volumes
- Lung cancer surgery volumes
- Transplant volumes (if applicable)
STS (Society of Thoracic Surgeons) data
STS public reporting may list institutional cardiac surgical volumes and outcomes. These don’t directly tell you resident case numbers, but a program performing only a few dozen cases a year is unlikely to support robust training.
Caution: Public data is program-level, not per-resident. You still need to confirm how those cases are allocated.
2. Ask Targeted Questions During Interviews and Virtual Sessions
This is where you, as a non-US citizen IMG, can differentiate yourself by asking focused, numeric, and CT-specific questions. Examples:
About total and per-resident volume
- “What is the average number of adult cardiac and general thoracic cases logged by recent graduates as primary surgeon?”
- “How far above the ACGME minimums do your typical residents graduate?”
- “Can you give an example of last year’s graduating chief’s cardiac and thoracic case numbers?”
About distribution over training years
- “At what PGY level do integrated residents begin performing full CABG or lobectomies as primary surgeon?”
- “How is complex aortic or transplant exposure distributed between fellows and residents?”
About autonomy and competition for cases
- “Is there competition for key index cases between fellows, residents, or APPs?”
- “How do you ensure that every trainee, including international graduates, gets adequate primary surgeon exposure?”
When you ask these questions, take note not only of the numbers, but also of the comfort and transparency of the faculty’s answers. Evasive or vague responses (“Our volume is fine, everyone meets requirements”) may be a red flag.
3. Speak Directly With Current Residents — Especially Any IMGs
Resident perspectives provide the most candid insights into actual surgical volume and autonomy:
Ask:
- “How many CABG and valve cases did you do as primary surgeon last year?”
- “Do you feel you are on track to exceed minimums comfortably?”
- “How does case allocation work between junior and senior residents?”
- “As an IMG or foreign national, did you feel you needed to ‘prove’ yourself longer before being given big cases?”
- “Are there rotations or sites where you feel underused or overused in terms of operative time?”
If there is a current or recent non-US citizen IMG in the program, prioritize their perspective. They can comment on:
- Whether they experienced any implicit bias in case assignment
- How quickly they got to lead major cardiac and thoracic cases
- How visa or employment issues affected their training or OR scheduling (usually indirectly, e.g., delayed start dates, credentialing, etc.)
Special Considerations for Non-US Citizen IMGs When Interpreting Case Volume
Even if a program has strong overall numbers, your personal experience may differ due to visa status, background, or institutional culture. Here are specific details foreign national medical graduates should analyze carefully.
1. Visa Sponsorship and Program Stability
Your immigration status should not directly determine your case volume, but realistically, instability with visas can indirectly affect your training timeline and opportunities.
Questions to clarify:
- “Do you regularly sponsor J-1, H-1B, or both for cardiothoracic residents?”
- “Have there been any recent cases where visa issues delayed a resident’s start or interrupted training?”
- “If a resident must extend training due to time lost to visa problems, how are cases handled to ensure they still achieve adequate procedure numbers?”
If a program has a history of not supporting visas robustly, or if their GME office is unfamiliar with international trainees, you risk interruptions that can shrink your effective OR exposure.
2. Transitioning From a Different Training System
Many non-US citizen IMGs come from healthcare systems with different:
- OR workflows
- Documentation expectations
- Definitions of “primary surgeon”
- Resource environments
Initially, this can affect:
- How quickly attendings trust you with the critical portions of cases
- How well you communicate in the OR
- Your perceived readiness for solo performance of procedures
Programs with structured onboarding, simulation, and mentoring for new IMGs generally help you ramp up faster and reach high case volume earlier in training. Ask:
- “What support is available for incoming residents who trained outside the US?”
- “Do you have bootcamps or simulation to help level-set operative skills?”
- “How early did the last international graduate start doing whole bypass cases or lobectomies independently?”
3. Competition With Fellows, Physician Assistants, and Advanced Practice Providers
In some systems, physician assistants (PAs) or nurse practitioners (NPs) function as first assistants on many cases, particularly in community or private-leaning environments. This can sometimes reduce the number of core cases available to residents.
Clarify:
- “In your typical CABG or valve case, who is usually first assist—resident or PA/NP?”
- “How are cases assigned when both advanced practice providers and residents are available?”
- “Do CT surgery fellows primarily handle the most complex cases, or are chiefs also primary surgeon?”
For a non-US citizen IMG, it is crucial to know that residents—not just PAs or fellows—are regularly performing full operations, especially in your senior years.
4. Balancing Service Load and Operative Time
High service obligations (notes, consults, floor work) can limit your ability to be in the OR, even when the overall surgical volume is technically high.
Ask residents:
- “How often do you miss cases because of floor or ICU responsibilities?”
- “Is there dedicated support (e.g., hospitalists, APPs) so residents can prioritize OR time?”
- “On a typical week, how many full OR days do you get?”
As a foreign national medical graduate who may have fewer local social supports, intense service burdens can also affect wellness and academic productivity. But in terms of pure heart surgery training, they can sink your operative exposure if not well-managed.
Strategizing Your Application: Matching Your Profile to the Right Volume Environment
Not all high-volume programs are ideal for every applicant. As a non-US citizen IMG, you should align your background, goals, and visa realities with the type of training environment that will maximize your residency case volume and long-term career potential.
1. Matching Prior Experience With Needed Exposure
Consider your starting point:
- If you already completed substantial general surgery training abroad, you may adapt quickly to an independent cardiothoracic pathway with intense operative expectations and shorter training time.
- If your operative experience has been limited, an integrated program with structured progressive responsibility may fit better, enabling a gradual but ultimately high-volume exposure.
In both scenarios, look for programs where graduating residents:
- Consistently exceed cardiac and thoracic case minimums
- Document strong primary surgeon numbers across key index cases
2. Thinking Ahead to Subspecialty Goals
Your targeted career (academic vs. community, cardiac vs. thoracic vs. congenital) influences how you value different aspects of case volume:
If you want adult cardiac-focused practice:
Prioritize programs with:- High CABG and valve volumes
- Regular exposure to advanced heart surgery training (aortic surgery, LVAD, transplant where available)
- High chief-level autonomy in cardiac cases
If you want thoracic or lung/esophageal-focused practice:
Emphasize:- Strong thoracic surgical volume (including cancer resections)
- High numbers of minimally invasive thoracic cases (VATS, robotic)
- Opportunities for thoracic-focused rotations and faculty mentorship
If you aim for transplant, aortic, or structural heart specialization:
Case numbers will matter, but so will:- Institutional programs in transplant and advanced heart failure
- Exposure to complex aortic work and hybrid procedures
- Research opportunities that complement your operative training
3. Using Case Volume to Compensate for IMG and Visa Barriers
Because some employers or fellowship directors may hesitate about hiring candidates who need visa sponsorship, you can increase your competitiveness by demonstrating:
- Robust procedure numbers compared to peers
- Excellent letters of recommendation from high-volume, well-known centers
- Evidence of handling complex operative responsibilities
In interviews, be ready to speak concretely:
“By graduation, I will have performed approximately 180 CABGs, 130 valve cases, and 90 thoracic resections as primary surgeon, including 40 minimally invasive or robotic procedures. My training has given me breadth and depth in both cardiac and thoracic domains, preparing me to contribute immediately to a high-volume practice.”
Specific, verifiable case volume data is especially persuasive when you are a non-US citizen IMG competing with US graduates.
Frequently Asked Questions (FAQ)
1. How many cases should I aim for by the end of cardiothoracic surgery residency to be competitive?
Exact numbers vary by institution and year, but in general, you should aim to clearly exceed ACGME minimums. For many strong programs, graduating residents log on the order of:
- ~150–200+ adult cardiac cases as primary surgeon
- ~80–120+ thoracic cases as primary surgeon
Higher numbers in your area of interest (cardiac vs. thoracic) are ideal. Above all, confirm that your case log reflects real technical responsibility, not just observational participation.
2. Are lower-volume programs always bad choices for non-US citizen IMGs?
Not necessarily. A lower-volume program with:
- Excellent case allocation to residents,
- High resident autonomy,
- A supportive culture for IMGs, and
- Strong mentorship and academic support
can sometimes be better than a famous, high-volume center where residents are overshadowed by fellows or PAs. However, truly low surgical volume inherently limits your procedure numbers, so be sure you still comfortably exceed requirements and feel technically confident.
3. Should I prioritize programs with transplant and LVAD when evaluating heart surgery training?
Transplant and LVAD exposure is valuable, especially if you want to work in advanced heart failure or academic centers. However, these are subspecialty skills built on a foundation of core cardiac surgery competence (CABG, valves, aortic work). If forced to choose, prioritize programs where you will get strong volume and autonomy in standard cardiac and thoracic cases before worrying about highly specialized procedures.
4. As a non-US citizen IMG, how can I prove that my foreign operative experience is real and relevant when programs evaluate my readiness for case volume?
Use multiple strategies:
- Maintain detailed case logs from your prior training, translated into English if necessary.
- Obtain specific letters from prior supervising surgeons describing the types and complexity of cases you performed and your role.
- Be prepared in interviews to discuss operative steps and decision-making at a detailed level.
- If possible, participate in US-based observerships, research, or simulation courses to demonstrate your familiarity with US standards.
Programs will then feel more comfortable entrusting you with early operative responsibility, which directly improves your residency case volume trajectory.
Thoughtful evaluation of surgical volume, procedure numbers, and per-resident experience is one of the most important decisions you will make as a non-US citizen IMG pursuing cardiothoracic surgery. With a structured approach—asking the right questions, validating data with current residents, and aligning programs with your background and goals—you can maximize your operative exposure and position yourself for a successful, sustainable career in heart and thoracic surgery.




















