
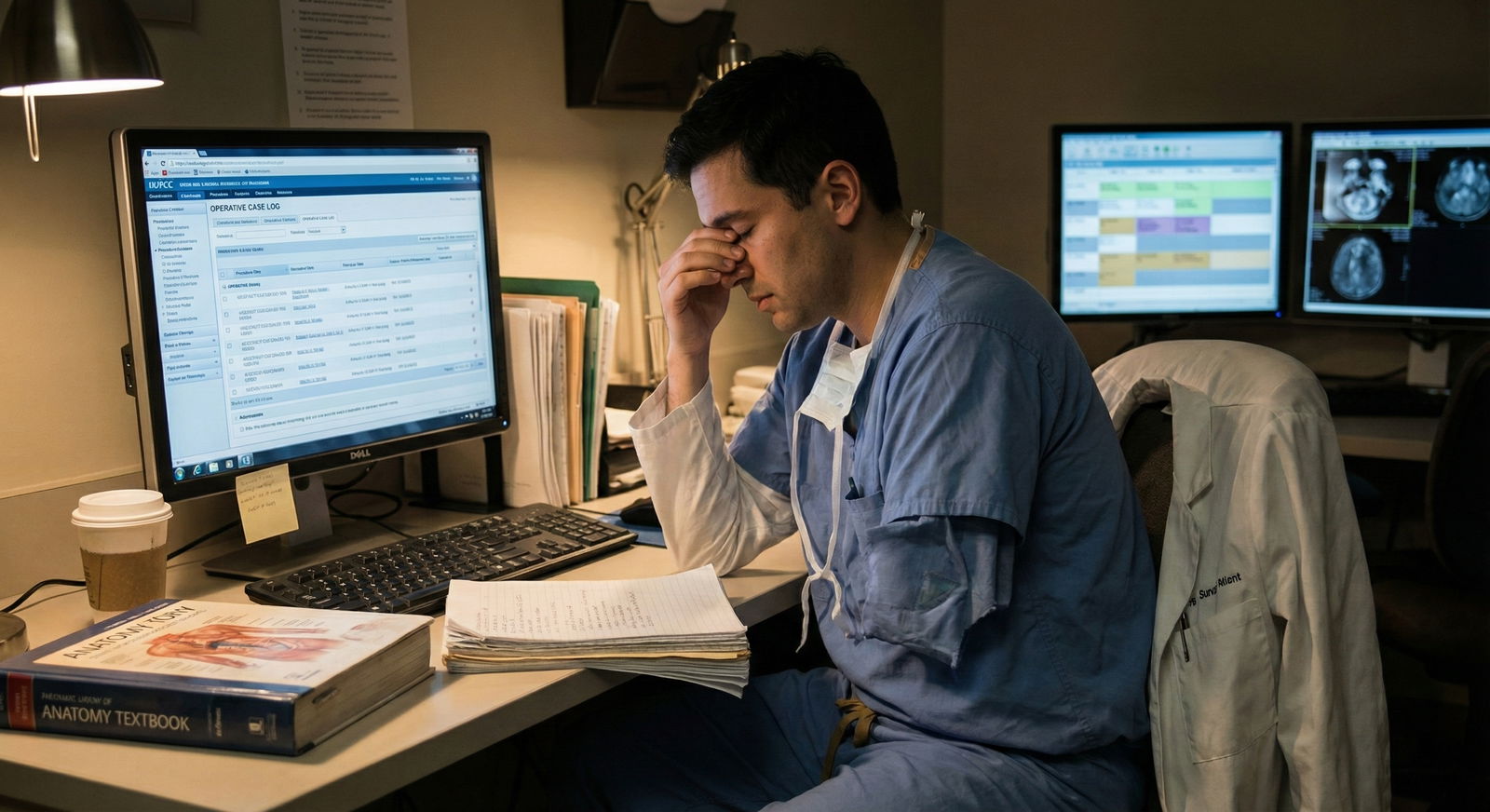
The obsession with surgical case numbers is quietly ruining a lot of surgeons’ futures.
The Case Volume Trap: What Everyone Gets Wrong
You’ve been sold a very narrow definition of “good training”: more cases, bigger cases, earlier autonomy. And yes, case volume matters. A lot.
But here’s the problem: plenty of residents chase numbers so aggressively that they essentially abandon clinic. They trade clinic half-days for extra OR time, skip follow-ups, ghost multidisciplinary visits, or treat clinic as a punishment instead of part of their education.
That’s not just a minor gap. It’s a career-limiting mistake.
Because the surgeon who only knows the OR and ignores clinic becomes:
- Bad at indications
- Bad at longitudinal decision making
- Bad at recognizing complications early
- Bad at building a practice that actually fills an OR schedule
And then, a few years later, they’re shocked when their case volume in practice stalls. Or when they’re miserable because every day in clinic feels like a foreign language exam.
Let me be blunt: if you sacrifice clinic for case volume during training, you’re mortgaging your future for a short-term ego boost.

| Category | Value |
|---|---|
| OR | 45 |
| Clinic | 20 |
| Inpatient/Call | 25 |
| Admin/Education | 10 |
Why Ignoring Clinic Quietly Destroys Your Future Practice
Surgery isn’t just cutting. It’s deciding who to cut, when to cut, and whether to cut at all. All of that is clinic.
Residents who duck clinic consistently make the same five mistakes.
1. You never really learn indications
You can memorize guidelines. You can quote trials. That’s not the same as actually developing judgment.
Real-world indications live in clinic:
- The obese diabetic with claudication and “maybe” rest pain
- The 82-year-old with early colon cancer and borderline functional status
- The 40-year-old with biliary colic and vague RUQ pain three times a year
- The breast mass that might be benign but is freaking out the patient
In the OR, everything is already decided. Consents signed, workup done, decision made. You scrub in, you execute, you leave. You almost never hear the messy pre-op thought process that led to being on that table.
Skip that long enough, and you end up as the “technician surgeon”:
- Fantastic hands
- Mediocre judgment
- Overly aggressive or overly timid, because you never saw enough gray-zone clinic decisions
I’ve heard attendings quietly say about a new partner, “Great in the OR. I just don’t trust their indications yet.” That comment never comes from lack of suturing reps. It comes from someone who clearly missed the clinic part of their training.
2. You don’t learn how volume is actually built
Residents often think case volume just appears if you’re technically good. That’s fantasy.
In real life, surgical case volume is built in three main ways:
- Direct patient referrals from clinic
- Referrals from other physicians who trust your clinic judgment
- Longitudinal follow-up that creates repeat and word-of-mouth referrals
All three are clinic-dependent.
If you’re never in clinic, you don’t learn how to:
- Structure a new patient visit so they leave understanding and trusting you
- Close the loop with referring physicians so they keep sending patients
- Identify which “low probability” patients still need safety-net follow up
- Convert an anxious, skeptical patient into someone willing to consent to surgery
You can do 120 colectomies or 300 laparoscopic cholecystectomies in residency. If you don’t know how to manage a half-day clinic efficiently and convincingly, your future schedule is going to have big, ugly gaps.
3. You miss complication recognition in real time
Complications don’t just show up in the OR. They show up in clinic and on the phone:
- The “just not right” feeling 10 days after a big abdominal surgery
- The mild but persistent wound erythema that’s the first hint of a deeper problem
- The vague shoulder pain post lap chole that’s actually a bile leak
- The early neuropathic symptoms after limb surgery you can still intervene on
Residents who blow off clinic miss a subtle but crucial skill: recognizing trouble early in a patient who looks “mostly fine” and isn’t yet septic or crashing.
Instead, they meet complications when they’ve already exploded. In the ED. At 2 AM. When options are fewer and morbidity is higher.
You want to be the surgeon who catches the leak before the patient is in multi-organ failure. That pattern recognition is built in clinic, not in the trauma bay.
4. You never get comfortable with “no surgery” decisions
Ask any senior surgeon: a huge part of your future clinic is saying “no” or “not yet” to surgery.
Patients who:
- Want a hernia fixed that doesn’t need it
- Demand spine surgery for non-surgical back pain
- Insist on mastectomy for low-risk lesions despite evidence
- Refuse surgery when it’s clearly indicated
If you avoid clinic as a resident, you never get enough reps learning how to:
- Say “no” clearly without being dismissive
- Document “no surgery” decisions properly and defensively
- Educate without lecturing
- Negotiate care plans when patients have unrealistic expectations
Then you graduate, join a practice, and suddenly every single “no surgery” conversation is draining, risky, and stressful. A lot of surgeons start caving and doing borderline-indicated surgeries just because they’re uncomfortable with conflict.
You can avoid that trap. But not if you never practice those conversations in clinic while you still have an attending backing you up.
5. You become dependent on someone else’s clinic judgment
The hidden danger: if all you know is “show up and cut,” you’re functionally dependent forever on someone upstream who decides what’s reasonable to book.
That’s fine as a resident. That’s job-ending as an attending.
In practice, you will:
- Be the only surgeon in a community
- Cover call without subspecialty backup
- Be asked to clear borderline cases for surgery
- Be asked to weigh in on complex multi-morbidity patients that anesthesia is worried about
If your instinct is always, “I wish someone would just tell me what to do,” that’s a training failure. And it’s almost always traceable back to poor clinic exposure.

How Residents Actually Fall Into the Case Volume Trap
Nobody wakes up and says, “I’d like to be bad at clinic.” The trap is subtler.
Here’s how it usually happens.
The culture problem
You hear things like:
- “Clinic is a waste of time, go to the OR instead.”
- “If you’re serious about fellowship, you should be in the room, not clinic.”
- “You can learn clinic later, you can’t learn Whipples later.”
And it’s not always wrong in the moment. Occasionally skipping a redundant clinic to do a rare case can be smart.
The mistake is turning that into a lifestyle. Months or years of systematically:
- Signing out clinic to juniors or PAs
- Showing up late to clinic because you “got stuck” in the OR (every single time)
- Leaving as soon as your attending lets you, without seeing follow-ups
- Treating clinic as optional “filler” time
Programs sometimes enable this because they’re chasing their own numbers for ACGME accreditation, marketing, or fellowship brag sheets.
The fellowship application panic
Around PGY-3 or PGY-4, if you’re fellowship-bound, the fear sets in:
- “Do I have enough major cases?”
- “The other applicant logged more pancreatectomies than I did.”
- “That person has 100+ carotids and I don’t.”
So you sprint for volume.
You beg to scrub in on every big case. You trade clinic for the OR every chance you get. You stop caring about post-op follow-up unless something spectacular is happening.
You get the numbers.
But you pay quietly in the background: your capacity to function as an independent surgical clinician never matures.
The “clinic will be easy later” myth
The most dangerous lie: “Clinic is common sense. I’ll figure it out when I’m an attending.”
No, you will not.
When you’re an attending you lose:
- Protected time to be wrong with supervision
- The buffer of “it’s the resident’s note”
- The ability to say “let me ask my attending” while you stall
- The freedom to learn without every decision creating medico-legal risk
Clinic is not just pattern recognition. It’s:
- Legal documentation
- Communication strategy
- Time management under constant interruption
- Prioritization when everything is overbooked
Those are not skills you casually acquire when you’re suddenly responsible for 30 patients in a morning and 4 rooms of OR in the afternoon.
| Focus Area | Short-Term Reward (Residency) | Long-Term Impact (Practice) |
|---|---|---|
| OR Volume | Strong fellowship application | Limited if clinic is weak |
| Clinic Time | Feels low-yield day to day | Drives future case volume |
| Call/ICU | Acute management skills | Essential but episodic |
| Conferences | Exam scores, research talks | Reputation, some referrals |
What You Actually Learn In Clinic (That You Won’t Get In The OR)
Let’s be very concrete. If you engage fully in clinic, here’s what you come out with that the pure-OR resident doesn’t.
1. Pre-op optimization that isn’t cookbook
Anyone can follow “stop smoking 4 weeks before surgery” and “optimize A1c.” That’s a brochure.
Clinic teaches you the messy part:
- The patient with an A1c of 9.5 and unstable housing who needs cancer resection
- The vascular patient who “can’t” stop smoking because of home stressors
- The anticoagulated atrial fibrillation patient needing spine surgery on a tight timeline
Attendings think out loud in these visits. You hear the real calculations:
- “I’ll accept higher risk because their disease is more dangerous than surgery.”
- “I’m not operating until cardiology signs off, period.”
- “We delay 3 months, optimize, and re-visit.”
That risk calculus is the heart of good surgery. You won’t learn it staring at a laparoscope.
2. Longitudinal outcome sense
In the OR, almost everyone looks fine at the end of the case. You close, you leave, you chart “patient tolerated procedure well.”
In clinic, you see:
- The patient 6 months out who’s still in pain after what you thought was a perfect case
- The one who had a minor intra-op complication but is thriving years later
- The subtle functional deficits you completely missed post-op on the ward
Over time, your internal compass shifts. You stop thinking “that was a cool case” and start thinking “that operation reliably produces good outcomes in this kind of patient.”
That’s the shift from trainee mindset to surgeon mindset.
3. Practice mechanics that nobody teaches formally
Future of medicine talk: private practice is under pressure, academic centers are consolidating, RVU models are changing. Through all of this, one thing stays constant: your clinic is your engine.
In clinic, you learn:
- How scheduling templates affect your day and your RVUs
- How new patient vs follow-up ratios impact future OR time
- How procedure-only clinics (endoscopy, minor procedures) can stabilize your revenue
- How team structure (NP/PA vs resident vs scribe) changes your throughput
You will not get a lecture titled “How to Build a Sustainable Surgical Practice.” You learn it by watching how your attendings run (or mismanage) their clinics.
If you’re never there, you’ll graduate with great hands and zero business sense in a system that’s increasingly hostile to surgeons with no efficiency.

| Category | Strong Clinic Training | Weak Clinic Training |
|---|---|---|
| Year 1 | 150 | 90 |
| Year 2 | 220 | 130 |
| Year 3 | 280 | 160 |
How To Chase Case Volume Without Sacrificing Clinic
You don’t have to pick one. Saying “clinic matters” doesn’t mean you sit out the interesting cases.
The mistake to avoid is mindless OR chasing. Here’s how you can be deliberate instead.
1. Protect at least one real clinic block per week
For most residents, one fully engaged half-day or full-day clinic per week, consistently over years, will give you enough exposure.
Key word: engaged.
That means:
- You show up on time, every time
- You see new patients and follow-ups, not just bounce between rooms aimlessly
- You write your own notes and think through the plan before the attending walks in
- You ask, “Can we talk through why you did X instead of Y for this patient?”
If your schedule is chaos, have a direct conversation with your program director: “I want to make sure I’m getting real clinic training. Where can I protect a consistent block?”
Residents almost never do this. The ones who do stand out later.
2. Be strategic about which clinics you prioritize
Not all clinics are equal for your learning.
High-yield clinics:
- New patient heavy general surgery or subspecialty clinics
- Post-op follow-up clinics for complex cases (vascular, oncologic, colorectal, spine)
- Multi-disciplinary tumor boards with same-day clinic visits
Lower-yield (but still important):
- Highly protocolized follow-up (e.g., simple wound checks only)
- Massive overbooking mill clinics where you’re just data entry
Do not make the mistake of thinking you have to attend every possible clinic. But don’t blow off the ones where actual decision making happens.
3. Tie your OR and clinic experiences together
One of the smartest habits you can build:
- See the patient in clinic pre-op
- Scrub their case
- See them post-op in clinic
Full arc. Indication → execution → outcome.
This is where you imprint patterns:
- “Ah, this was the frail lady with COPD I wasn’t sure about. How did she do?”
- “This was that borderline limb salvage we debated. Was it worth it?”
If you’re only ever involved in the “execution” piece, you’ll overestimate how good some operations really are, because you never see the real cost.
4. Learn to say “yes” and “no” to OR swaps intelligently
You will be tempted with “Come to this big case instead of clinic.”
Sometimes, the right answer is yes. Often, it’s no.
Useful mental checklist:
Say YES when:
- It’s a rare case you may never see again
- You’ve already been consistent with clinic that month
- Your presence will actually involve meaningful participation, not just standing in the corner
Say NO when:
- It’s the fourth similar case this month and you’ve barely done clinic
- You’re the primary resident for clinic and bailing dumps work on others
- You’re already weak on outpatient decision making and you know it
This is where you separate yourself from the volume addicts. You’re not just collecting numbers; you’re building a complete surgeon.
5. Treat clinic skills as part of your “competency portfolio”
Residents obsess over their technical skill curve. Fine. Do the same thing for clinic.
By the time you graduate, you should be able to independently:
- Run a new patient consult for a common problem (hernia, gallbladder disease, vascular stenosis, spine degenerative disease)
- Explain risks/benefits/alternatives of the operation clearly and honestly
- Document a defensible plan whether the answer is “operate” or “no operation”
- Handle a typical post-op visit efficiently: wound check, med adjustment, activity guidance, red flag education
If you can’t do that confidently, I don’t care how many big cases you logged — there’s a gaping hole in your training.
The Future of Surgery: Clinic Will Matter Even More
With telemedicine, value-based care, and increasingly data-driven outcomes, ignoring clinic is going to age poorly.
Trends you can’t ignore:
- More complex patients staying out of hospitals longer ⇒ more management happens in clinic
- Bundled payments and quality metrics ⇒ avoidable complications hammer your group financially
- Telehealth follow-ups ⇒ you must be able to recognize subtle problems through a screen and a conversation
The surgeons who thrive in that world will be:
- Technically excellent
- Efficient in clinic
- Brilliant at risk stratification and communication
The technician who only trained in the OR is going to feel increasingly out of step. Worse, they’ll be the one showing up in M&M again and again with “late presentation” complications everyone else would’ve caught earlier.

| Step | Description |
|---|---|
| Step 1 | PGY1-2 |
| Step 2 | Develop Judgment |
| Step 3 | Chase OR Volume Only |
| Step 4 | Balanced Skill Set |
| Step 5 | High Technical Skill Only |
| Step 6 | Stronger Practice and Outcomes |
| Step 7 | Lower Future Case Volume |
| Step 8 | Clinic Engaged? |
FAQs (Exactly 5)
1. My attending keeps telling me to skip clinic for the OR. Am I supposed to ignore them?
You don’t ignore them, but you also don’t blindly comply every time. Have an adult conversation: “I really value OR time, but I also want to make sure I’m getting enough clinic to develop my outpatient judgment. Can we plan which days make most sense for me to be in clinic vs the OR?” Attendings who respect trainees will respect that. If none of them do, escalate to your program leadership and frame it as a training completeness issue, not a complaint.
2. I’m going into a super-technical fellowship (e.g., HPB, complex spine). Doesn’t that justify prioritizing OR over clinic?
No. It just raises the stakes. The more complex and risky your operations, the more crucial your selection and follow-up skills become. HPB disasters and spine complications often declare themselves in clinic first. Being technically elite without outpatient judgment is exactly how catastrophic complications sneak up on you. You need both, not one.
3. Our clinic is disorganized and feels like a waste. Should I still bother?
Yes, but be smart. If the clinic is pure chaos, use that as a lab: How would you structure it better? What’s slowing things down? Watch how your attending still makes decisions despite the mess. If there is truly zero teaching, ask to rotate through a better-run clinic with a different attending. Do not use “bad clinic” as an excuse to ditch clinic entirely. Learn from what’s broken too.
4. Will fellowship directors actually care that I did clinic, or just about my case numbers?
Most will not explicitly ask, “How was your clinic experience?” But seasoned program directors can smell a technician with weak judgment from your letters, your interview answers, and how you talk through cases. The letter that says, “This resident understands indications and follow-up extraordinarily well” carries more weight than, “They did 50 more major cases than average.” They want people who will not embarrass them later with reckless decisions.
5. I’m already a senior and feel weak in clinic. Is it too late to fix this?
It’s late, but not too late. Stop auto-prioritizing OR over clinic. For the rest of your training, deliberately choose full-arc experiences: see the consult, scrub the case, see the follow-up. Tell your attendings directly: “I want more reps running visits myself and presenting plans; please push back if my thinking is off.” And when you start as an attending, lean into clinic instead of hiding in the OR. You’ll be tired and slow at first. That’s fine. Better clumsy under your own name than dangerous and blind.
If you remember nothing else:
- OR volume without clinic judgment is a short-term flex and a long-term liability.
- Your future surgical case volume in practice will depend more on how you run clinic than how many cases you logged as a resident.




















