
Understanding Case Volume in Interventional Radiology for IMGs
For an international medical graduate (IMG) interested in interventional radiology (IR), understanding case volume is not just a numbers exercise—it is central to selecting the right residency, demonstrating your readiness, and planning a sustainable career. In IR, where training is built around procedures, residency case volume, surgical volume, and procedure numbers directly influence your technical confidence, clinical breadth, and fellowship/job competitiveness.
This IMG residency guide focuses on case volume evaluation for those targeting an interventional radiology residency (US-style Integrated or ESIR-eligible Diagnostic Radiology pathway, and similar structures in other countries). You will learn how to interpret and compare case numbers, assess program quality beyond raw counts, and present your own experience convincingly in the IR match.
1. Why Case Volume Matters So Much in Interventional Radiology
Case volume has special importance in IR compared with many non-procedural specialties. As an IMG, you may compete with applicants who trained in systems where IR is deeply integrated and standardized. Understanding how volume interacts with training quality will help you close that gap.
1.1 What “case volume” really means in IR
In IR, “case volume” usually refers to:
- Total number of procedures performed by residents/fellows during training
- Number of specific procedure types, for example:
- Vascular access (tunneled lines, ports, PICCs)
- Embolization (GI bleed, trauma, uterine fibroid embolization, PAE)
- Oncologic interventions (TACE, Y-90, ablations)
- Venous interventions (DVT/PE, IVC filters, venous stenting)
- Peripheral arterial disease interventions
- Biliary and GU interventions (nephrostomies, ureteral stents, biliary drains)
- Interventional oncology biopsies and drainages
- Responsibility level:
- Primary operator
- Assistant
- Observer
When evaluating an IR residency, think in terms of procedure numbers per resident, not just “our department does 8,000 cases per year.”
For your own experience, program directors care more about what you did and how often you did it than a big total case number with unclear role.
1.2 Why volume is especially critical for IMGs
As an international medical graduate, case volume impacts you in several ways:
Bridging training differences
IMGs come from diverse systems—some with strong IR exposure, others where IR is minimal. Demonstrated procedure numbers help program directors interpret your background.Showing procedural aptitude
Documented hands-on experience counters bias that “IMGs may have weaker procedural skills” due to system differences.Competing for interventional radiology residency spots
In a specialty with limited positions, clear evidence of procedural commitment and familiarity can differentiate you in the IR match.Smoother transition to US-style training
Prior case exposure (even if not IR-specific) can make you safer and faster in learning IR workflows, sterile technique, and imaging-guided procedures.
2. Standards, Benchmarks, and How Programs Think About Volume
To evaluate case volume intelligently, you need to know how US and similar systems define adequate experience and what accrediting bodies expect.
2.1 Regulatory and accreditation expectations
While details evolve, several concepts frame case expectations:
- ACGME (US) for IR/DR and independent IR:
- Sets minimum procedure categories and broad thresholds by graduation.
- Emphasizes breadth of exposure, not just high numbers in one category.
- Society of Interventional Radiology (SIR) and similar bodies:
- Issue practice recommendations, common graduation targets, and competencies.
- Hospitals/health systems:
- May have their own internal benchmarks for granting IR privileges post-residency, often citing a minimum number of certain case categories.
For IMGs applying to US IR residencies, you don’t need to know every number, but you should recognize that programs think in terms of meeting and exceeding minimums while ensuring well-rounded exposure.
2.2 Typical IR case exposure ranges
These are illustrative ballpark ranges, not official requirements, but they can help you evaluate program claims and your own exposure:
Overall US IR resident graduation range (integrated pathway, per resident):
- Often 1,200–2,000+ IR procedures, with:
- A large proportion of vascular access, drainages, and biopsies
- Meaningful exposure to embolization and complex interventions
- Often 1,200–2,000+ IR procedures, with:
Per-year ranges during dedicated IR years:
- 300–600+ procedures/year per resident in active programs
For IMGs comparing programs:
- A program where residents graduate with < 800 total IR cases may raise concern unless there is clear explanation (e.g., heavily subspecialized rotation structure with strong independent IR fellowship afterward).
- A program boasting extremely high numbers (2,500–3,000+ cases) could be excellent—or could indicate:
- Heavy emphasis on low-complexity, repetitive cases
- Minimal time for teaching and reflection
- Fatigue and limited case ownership
Your goal: target a balanced, high-quality case volume, not just the highest number.
2.3 Categories that matter more than raw totals
Programs and credentialing bodies particularly scrutinize:
- Angiography and embolization
- Endovascular interventions (arterial and venous)
- Non-vascular interventions (biliary, GU, GI)
- Interventional oncology (ablations, intra-arterial therapies)
- Image-guided biopsies and drainages
A strong IR program ensures:
- Exposure to all core categories, and
- Opportunity to progress from assistant to primary operator in each area.

3. Evaluating Program Case Volume as an IMG Applicant
When reading program websites or talking to residents, you must translate vague claims (“high volume center”) into concrete, comparable information. This is where a structured IMG residency guide mindset is powerful.
3.1 Key questions to ask about residency case volume
Use these during virtual sessions, interviews, or email exchanges with current residents and faculty:
Total and per-resident volume
- “Approximately how many IR procedures does each resident perform by graduation?”
- “What is the typical annual procedure number per resident during the dedicated IR years?”
Distribution by procedure type
- “Can you give a rough breakdown of your case mix—what percentage is vascular access, embolization, interventional oncology, venous work, etc.?”
- “Do residents get hands-on experience with TACE/Y-90, ablations, and complex PAD cases regularly?”
Level of responsibility
- “At what PGY level do residents usually become primary operator for common cases like tunneled lines, drainages, or biopsies?”
- “By graduation, are residents typically leading complex procedures (e.g., embolization) under supervision?”
Competition for cases
- “Is there any competition with fellows, advanced practice providers, or multiple residency programs for IR cases?”
- “Are there enough complex cases for every resident to do them multiple times, not just observe once?”
Call and after-hours exposure
- “What kind of emergent IR call do residents take? Do they get hands-on experience with trauma, stroke, and GI bleed interventions?”
Tracking and feedback
- “Does the program formally track procedure numbers and review them with residents regularly?”
- “How does the program intervene if someone’s case numbers fall behind?”
Note the specificity of these questions. Strong programs will answer confidently with approximate numbers and examples. Vague, evasive responses (“We do plenty of cases, don’t worry”) are a red flag.
3.2 Reading between the lines of program descriptions
Common phrases and how to interpret them:
“High-volume tertiary care center”
- Could be good, but ask: How is that volume distributed across residents? Is most of it done by attendings or fellows?
“Strong interventional oncology program”
- Ask: Do residents actually get to perform IO procedures, or mostly observe? How many Y-90/TACE/ablation cases per resident?
“Residents get early hands-on experience”
- Clarify: What does ‘early’ and ‘hands-on’ mean? Primary operator or only basic tasks?
“We share cases with the independent IR fellows”
- This can be beneficial (extra teaching) or detrimental (case dilution). Ask how it’s structured.
As an IMG, your goal is not to find a program that simply “sounds good,” but one where procedure numbers per resident, across key categories, and at increasing levels of responsibility are clearly articulated.
3.3 Special considerations for community vs academic programs
Large academic centers
- Pros: Typically high total volume, complex referrals, exposure to cutting-edge techniques.
- Cons: Fellows may take some advanced cases; residents may see more complex but fewer bread-and-butter cases.
High-volume community programs
- Pros: Often excellent hands-on exposure, residents as primary operators, less competition with fellows.
- Cons: Case mix may be skewed toward bread-and-butter; fewer rare or complex IO cases.
For IR, an ideal training trajectory often combines academic exposure to complexity with community-style volume and autonomy—sometimes through away rotations or electives.
4. Evaluating and Presenting Your Own Case Volume as an IMG
Beyond choosing the right residency, you must understand and communicate your own procedure numbers effectively in the IR match or similar systems.
4.1 Types of procedural experience that count
While US IR programs won’t expect you to have performed hundreds of IR-specific procedures before residency, they do value:
Direct IR experience
- IR electives or observerships
- Hands-on roles in IR procedures in your home country (if allowed)
- Documented participation in angiography, drains, biopsies, ablations, etc.
Related procedural specialties
- General surgery, vascular surgery, cardiology cath lab, endoscopy
- Central line placement, chest tubes, paracentesis, thoracentesis
- Ultrasound-guided procedures in emergency medicine, anesthesiology, or ICU
Simulation and workshops
- IR simulation labs
- Vascular access workshops
- Ultrasound-guided procedure courses
When building your narrative as an IMG, make sure you connect any procedural background to your potential to excel in IR.
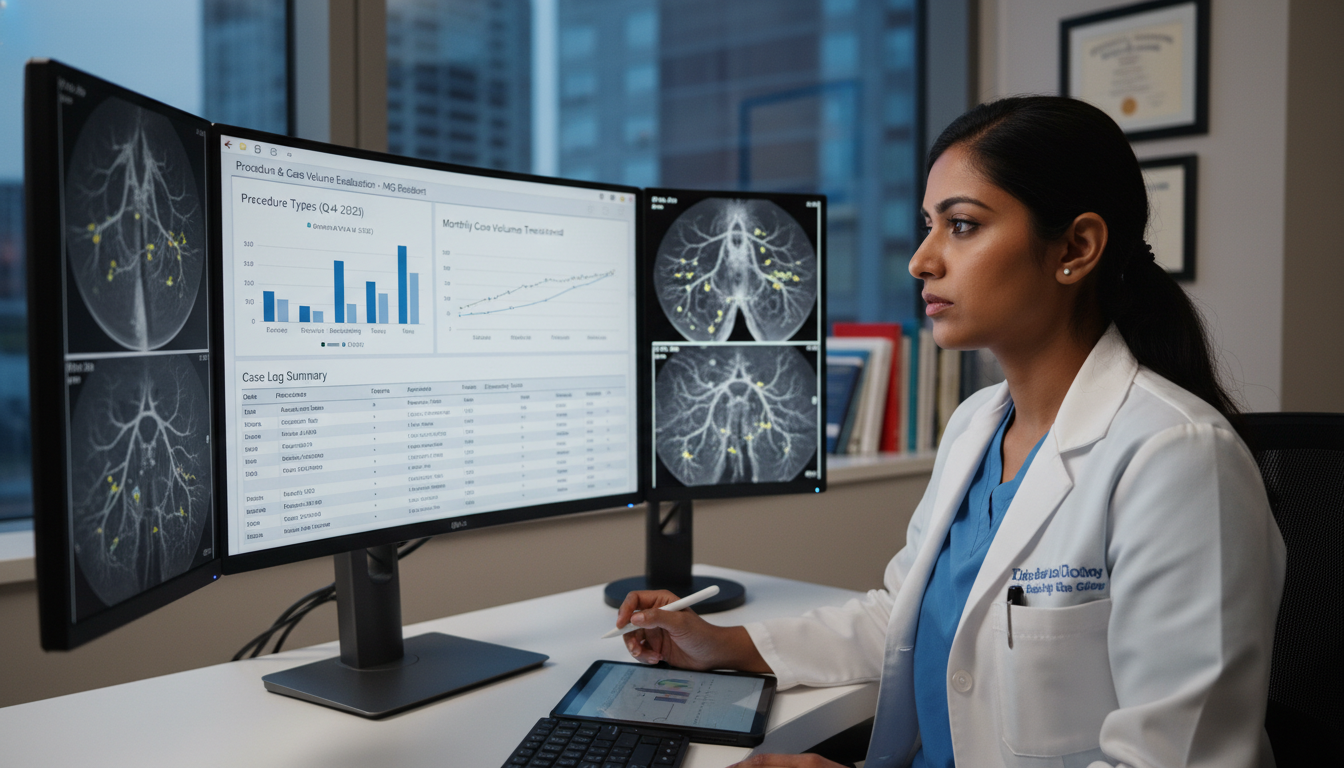
4.2 How to document your procedure numbers
A structured approach makes you more credible and allows program directors to quickly understand your experience:
Maintain a personal case log
- Use a spreadsheet or app with fields like:
- Date
- Procedure type
- Your role (observer / assistant / primary operator)
- Setting (IR, surgery, ICU, etc.)
- Complications (if known)
- Even if your home institution doesn’t require this, start retrospectively and then keep it updated.
- Use a spreadsheet or app with fields like:
Organize by category For example:
- Vascular access: central lines, dialysis catheters, ports
- Drainages: paracentesis, thoracentesis, abscess drains
- Biopsies: US/CT-guided where applicable
- Other: chest tubes, lumbar punctures, etc.
Quantify and summarize In your CV or personal statement, instead of:
- “Did many central lines and paracenteses” Use:
- “Performed approximately 90 central venous catheter placements and 60 ultrasound-guided paracenteses as primary operator during my internal medicine and ICU rotations.”
Align terminology with IR practice Where appropriate, use terms familiar to IR attendings:
- “Ultrasound-guided vascular access”
- “Image-guided fluid drainage”
- “Fluoroscopy-assisted procedures”
4.3 How to present your case volume in your application
In the IR match or any residency application process, focus on three aspects:
Competence
- Show you know sterile technique, ultrasound basics, catheter/wire fundamentals, and peri-procedural care.
- Use specific examples:
“In our ICU, I routinely used ultrasound for internal jugular and femoral central access, managing real-time needle visualization and wire advancement.”
Growth trajectory
- Describe how your responsibilities increased over time.
- For example:
- Early: observing IR procedures
- Later: scrubbing in, handling catheters, controlling the C-arm, assisting with embolization.
Insight and reflection
- Highlight what high or low procedural exposure taught you:
- Patient selection
- Radiation safety
- Complication recognition and management
- This shows maturity beyond “I just want to do a lot of cases.”
- Highlight what high or low procedural exposure taught you:
5. Balancing Quantity, Quality, and Wellness in Case Volume
High case volume is attractive, but without the right structure, it can become counterproductive. As an IMG, you should assess programs for sustainable, educationally rich volume, not “maximum throughput at all costs.”
5.1 Signs of healthy volume
Look for these indicators when speaking with residents and faculty:
Structured progression
- Junior residents start with simpler procedures (lines, paracenteses, basic drainages).
- Senior residents lead complex embolizations, oncologic interventions, and venous/arterial work.
Attending supervision with teaching
- Attendings scrub in and actively teach, not just step in when things go wrong.
- Case load allows for case review and feedback, not just rushing from case to case.
Protected didactics
- Despite high volume, residents regularly attend conferences, M&M, tumor boards, and IR-specific teaching sessions.
Diversity of case mix
- No single category dominates; you see oncologic, vascular, non-vascular, emergent, and elective procedures.
5.2 Warning signs of problematic volume
Red flags include:
Case overload without autonomy
- Residents report 10–15 cases per day but are mostly retractors or table-side assistants with limited hands-on catheter work.
Burnout signals
- Residents mention consistently late finishes, no breaks, no time for reading or research.
- High turnover or residents discouraging you from ranking the program.
Narrow procedural focus
- 70–80% of cases are ports and basic drains with minimal complex work.
- Emergent or complex cases mostly handled by attendings or fellows, not residents.
Poor tracking
- No formal case log review or remediation plan for low numbers.
- Residents are uncertain about how many cases they have done in each category.
As an IMG, protecting your own wellness and learning environment is critical—especially if you are also navigating immigration, cultural, and linguistic transitions.
5.3 Case volume and career pathways
Case volume during residency influences:
- Confidence entering independent practice or fellowship
- Eligibility for subspecialized IR fellowships (in systems that still use them)
- Scope of practice you feel comfortable offering:
- Some low-volume programs may graduate residents who primarily offer bread-and-butter IR.
- High-quality balanced volume programs enable broader IR practice: complex arterial, advanced IO, venous recanalization, etc.
When you consider future careers—academic vs community, high-end IO vs broad-based IR—ask whether the program’s case volume and mix align with your long-term goals.
6. Practical Action Plan for IMGs Targeting IR and Evaluating Case Volume
To turn these concepts into action, follow a stepwise strategy tailored to IMGs focused on interventional radiology residency.
6.1 Before applying
Clarify your IR interest level
- Are you committed to IR as a career, or exploring? Your case volume strategy (electives, observerships, research) depends on this.
Build a basic procedural foundation
- Seek rotations that allow ultrasound-guided procedures, central lines, chest tubes, and drains.
- Log your procedures meticulously from day one.
Pursue IR exposure
- IR electives or observerships in your home country or abroad.
- Even if you can’t scrub in (observer status), learn procedural steps, devices, indications, and complications.
Create a preliminary case volume summary
- Even if small, quantify:
- “5 IR procedures observed”
- “30 central lines, 20 paracenteses, 10 thoracenteses as primary operator”
- This gives you a baseline and shows seriousness.
- Even if small, quantify:
6.2 During application preparation
Target programs realistically
- Use this IR-focused IMG residency guide logic:
- Research which programs are known for strong IR and procedural training.
- Pay attention to whether they welcome IMGs based on historical match lists.
- Use this IR-focused IMG residency guide logic:
Refine your documentation
- Integrate case numbers into:
- ERAS CV (or equivalent)
- Personal statement (briefly, not as a list)
- Letters of recommendation (ask mentors to mention your procedural competence if appropriate)
- Integrate case numbers into:
Prepare focused questions about case volume
- Use the question list from Section 3.1.
- Practice asking them clearly and concisely in conversations.
6.3 During interviews and open houses
Ask current residents for numbers
- “Roughly how many IR procedures have you logged so far, and what PGY level are you?”
- “How many times have you personally done common things like TACE, UFE, or DVT thrombectomy?”
Probe for autonomy and supervision
- “Do you feel comfortable doing [procedure] independently as you approach graduation?”
- “How do attendings balance letting you work with ensuring patient safety?”
Observe culture around volume
- Are residents proud of their experience yet realistic about workload?
- Do they describe supportive attendings, or just volume and exhaustion?
6.4 Creating your rank list / final decisions
Weigh case volume with other factors
- Balance:
- Case volume and mix
- Learning environment
- Geography and support systems (important for IMGs)
- Visa and institutional support
- Balance:
Prioritize balanced, well-documented volume
- A program with:
- Moderate-to-high well-distributed volume
- Strong teaching
- Healthy culture
Will usually provide better training than a hyper-volume program with minimal mentorship.
- A program with:
Think long-term
- Visualize the cases you want to be comfortable with 5–10 years into practice.
- Choose a residency that will logically get you there through its procedure numbers and case diversity.
Frequently Asked Questions (FAQ)
1. As an IMG, do I need prior IR procedures to match into an interventional radiology residency?
No. Programs understand that many IMGs come from systems with limited IR access. You are not expected to have performed IR procedures independently. However, any documented procedural experience (central lines, paracenteses, thoracenteses, biopsies) and exposure to IR (observerships, electives, research) will strongly support your application and demonstrate your fit for a procedural specialty.
2. How many procedures should I aim to log before applying to IR as an IMG?
There is no official minimum, but as a rough guide, having:
- Dozens of basic procedures (e.g., 30–100+ central lines and other ultrasound-guided access or drainages)
- Several IR observations or assisting experiences, if possible
shows credible interest and skill. Focus less on hitting a magic number and more on documenting carefully, reflecting thoughtfully, and connecting your experience to IR.
3. When programs report “high case volume,” what should I ask to clarify if it’s really good for trainees?
Ask:
- “Approximately how many IR procedures does a typical resident log by graduation?”
- “What is the balance between simple and complex procedures?”
- “How often are residents primary operator on cases like embolizations, IO procedures, and venous/arterial interventions?”
- “Is there competition with fellows or other services for these cases?”
Their answers will help you distinguish true high-yield training from high throughput with limited resident benefit.
4. How can I compare case volume between programs if they don’t publish numbers?
Most programs don’t list specific procedure numbers online. Use:
- Conversations with current residents (ask them to approximate their logs)
- Questions about case mix and autonomy
- Informal reputation and match outcomes (do graduates go into strong IR jobs/fellowships?)
If a program consistently avoids giving any sense of per-resident procedure numbers or responsibility levels, treat this as a caution sign and consider other programs that are more transparent.
By understanding case volume deeply—how to evaluate programs and how to present your own experience—you, as an international medical graduate, can navigate the IR match more strategically and position yourself for a strong, sustainable career in interventional radiology.



















