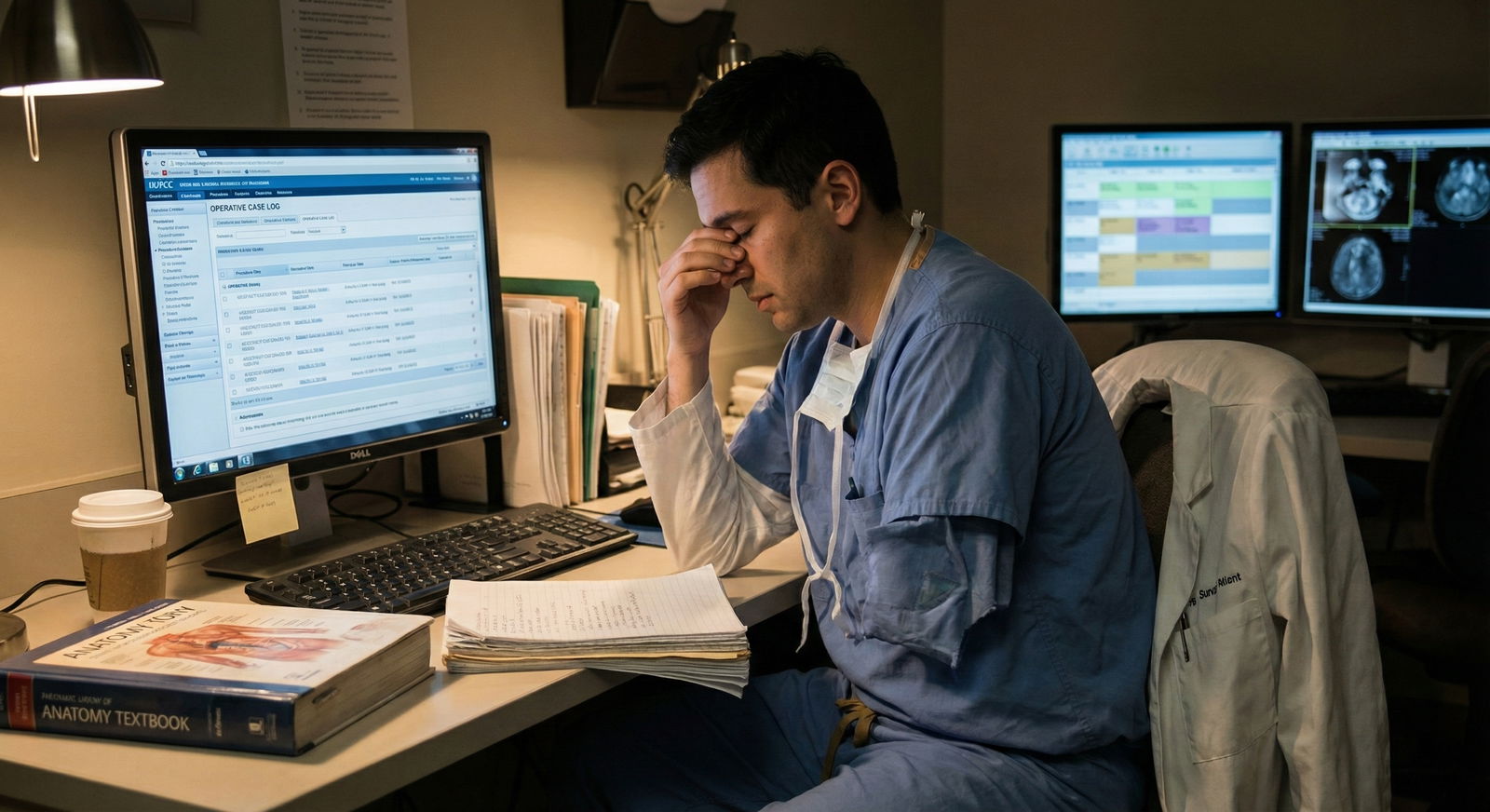
The residents who miss out on fellowships are usually not the ones with “bad hands.” They are the ones with bad documentation.
You can be technically gifted, hard‑working, and beloved on the wards—and still get quietly filtered out because your case log is incomplete, inconsistent, or obviously reconstructed at the last minute. Fellowship committees will never meet you if your numbers do not add up. That is how brutal and bureaucratic this part of the process is.
Let me be very clear: not tracking your cases from day one is a self‑inflicted wound. And it can absolutely wreck your fellowship application.
The Hidden Gatekeeper: Case Volume and Documentation
Programs do not just care that you operated. They care that they can prove you operated.
They use three things, in combination, as a gatekeeper for interviews:
- Total case numbers
- Case mix (complexity, index cases, diversity)
- How clean and consistent your documentation looks
If your logs look like they were created during a single caffeine‑fueled weekend in March of your chief year, you have already thrown away credibility.
I have watched this play out in real time:
- An applicant with “700+ major cases” but obvious bulk entry dates gets quietly pushed down the pile.
- Another with “average” but well‑documented, believable case logs, plus strong letters, gets the interview.
Nobody on a serious committee believes that you “forgot to enter cases for 18 months and then remembered all of them.” They assume something worse: exaggeration, sloppiness, or both.

| Category | Value |
|---|---|
| Bulk entries | 80 |
| Impossible volumes | 65 |
| Wrong roles | 55 |
| Missing index cases | 50 |
Those “red flag” patterns show up more often than you think. And most come from one root problem: residents did not start tracking their cases early and accurately.
Mistake #1: Assuming ACGME or Your EMR Will Save You
The laziest and most dangerous assumption is this: “I do not need to track anything; ACGME/OPLOG/EPIC has everything.”
No. It does not. And here is where residents get burned.
The fantasy: “The system logs all my cases automatically.”
The reality:
- Wrong attending assigned
- Your role mis‑labeled (assistant vs primary vs teaching)
- Cases missing because of billing or scheduling glitches
- Combined procedures misclassified or under‑captured
- Robotic/endo portions not coded in the way fellowships expect
I have seen residents in their PGY‑5 year run their ACGME report for the first time and realize half their early trauma call nights are not there. That big colectomy where they did everything? Logged as “assistant.” The complex redo case? Billed as something generic, so it does not show up in the index category they were counting on.
By the time you discover that in your chief year, you are out of runway. You cannot go back and fix two or three years of sloppy or missing entries in a credible way.
What happens when you trust “the system”?
You end up with:
- Case totals that look average on paper even if your real experience was strong
- Index case categories that fall below fellowship expectations
- No way to reconstruct specifics for your personal statement or interviews
And yes, reviewers can tell when your story (“I love complex foregut and have done a ton”) does not match your case log (“foregut volume below program mean, mostly assistant”).
That disconnect does not just hurt you. It makes people actively distrust your application.
Mistake #2: Reconstructing Logs from Memory in Your Chief Year
This is the most common disaster pattern: ignoring case logs for years, then trying to salvage everything in a last‑minute panic.
The email often looks like this:
“Hey, do you remember that Whipple we did in April of my PGY‑3 year? I’m trying to enter it now and do not remember the exact date…”
If you are sending that email, you are already in trouble.
Why “catch‑up logging” fails
Reconstructing two or three years of cases from memory has three predictable outcomes:
You miss a huge number of cases.
You remember big Whipples and ruptured AAAs. You forget the dozens of bread‑and‑butter cases that actually build volume: hernias, cholecystectomies, appendectomies, scopes. Those bread‑and‑butter numbers matter for both ACGME minimums and fellowship expectations.Your dates and details look fake.
Bulk case entry with identical dates, approximate months, or suspicious patterns (suddenly 25 cases from the same week) stand out. These logs get flagged informally with comments like “clearly reconstructed.”You mis‑code roles and case types.
When you are guessing after the fact, you will over‑assign yourself as primary or misclassify the procedure type. That is when people start throwing around words like “dishonest,” not just “disorganized.”

Here is the part nobody tells you: fellowship directors talk. If your log looks obviously reconstructed, someone will mention it in a group text or at a conference. You do not just hurt yourself at one program; you poison your reputation across several.
Mistake #3: Ignoring Case Mix Until It Is Too Late
Residents obsess about total numbers and forget something more important: the pattern of what you actually did.
For fellowships—especially competitive ones like surgical oncology, colorectal, MIS/bariatrics, vascular, and transplant—the mix is what tells your story.
If you only focus on “I need X total cases” without tracking early, you run straight into two problems:
- You discover in PGY‑4 that you are weak in the exact category your desired fellowship cares about.
- You have no documentation to prove the niche experience you are trying to sell in your personal statement.
Example: The “late‑deciding” MIS applicant
I watched a resident decide, in late PGY‑4, that they wanted an MIS fellowship. Strong technically, respected by faculty. But when we pulled their logs:
- Very high trauma and bread‑and‑butter general surgery volume
- Minimal foregut, bariatric, or advanced laparoscopy documented
- Robotic cases scattered, with unclear role documentation
Had they tracked and reviewed their case mix every 6 months, they would have seen the gap in PGY‑2 or PGY‑3 and advocated for more MIS time. But by PGY‑4, the schedule was mostly fixed, and other residents were already invested in those rotations.
The fellowship director did not reject them because they were “bad.” They passed because there were other applicants with equal references and a proven, well‑documented track record in MIS cases. Data wins.
| Category | Applicant A (Tracked Early) | Applicant B (Late Logger) |
|---|---|---|
| Total Major Cases | 850 | 820 |
| Advanced Lap Cases | 220 | 95 |
| Foregut Procedures | 140 | 45 |
| Bariatric Cases | 80 | 18 |
| Robot Cases (Primary) | 60 | 12 |
Applicant B is not obviously “worse” by total case volume. But the mix is a clear mismatch for what MIS programs want. That mismatch is avoidable if you review your data early and often.
Mistake #4: Sloppy Role Documentation (Assistant vs Primary)
Fellowships care deeply about what you actually did in the OR. Not just that you were standing in the room.
If your logs show you as “assistant” on most complex cases—even when you remember driving most of the operation—you lose ground quickly.
The common failure pattern: leaving role selection on autopilot or letting default EMR settings decide for you. Residents then discover too late that:
- Many of their complex cases are logged as assistant
- They cannot credibly “fix” hundreds of entries at once
- Their logs look like they never progressed to real operative independence

| Category | Primary | Assistant | Teaching |
|---|---|---|---|
| Strong Applicant | 65 | 25 | 10 |
| Weak Applicant | 35 | 45 | 20 |
I have seen fellowship committees go straight to role distribution before even reading letters. A resident with 700 cases but a low percentage as primary on key operations looks less mature than one with fewer cases but a stronger independence profile.
If you fail to track and correct these role assignments in real time, you are stuck with an unfixable story. And it is the wrong story.
Mistake #5: No Personal Tracking System Outside the Official Log
Relying solely on the official ACGME or institutional log is another subtle mistake. You need your own parallel system.
Not for cheating or inflating numbers. For context.
The most prepared fellowship applicants I have seen all did some version of this:
- A simple spreadsheet or note where they recorded:
- Date, attending, procedure, role
- Key technical steps they performed
- Complications or interesting learning points
- Any case that could become an interview talking point
When you skip this, three bad things happen:
Your interviews sound generic.
You cannot recall specific cases in detail, so you speak in vague terms: “I have done a lot of…” instead of “On my PGY‑3 MIS rotation, I led a challenging paraesophageal hernia repair on a frail patient with…” Fellowship directors notice the difference.You cannot prove growth.
You may have a sense that you have improved technically, but you cannot point to a pattern—“early in residency I was assisting on X; by PGY‑4 I was primary on Y and teaching juniors.”You lose powerful letter content.
When you remind attendings of specific cases you did together, their letters become detailed and compelling. If you do not track those cases, they default to the same bland, boilerplate praise.

Your personal system does not need to be beautiful. It just needs to exist, and you need to use it early.
Mistake #6: Waiting Until You “Know” Your Fellowship Field
Many residents tell themselves a comforting lie: “I’ll start tracking my subspecialty cases once I know what I want to do.”
By the time they “know,” they have already missed:
- Early but important exposure cases
- The chance to build a longitudinal story with one or two mentors
- The opportunity to adjust rotations to fill gaps in their desired field
If you decide in PGY‑4 that you want vascular, and then realize you barely logged your PGY‑2 vascular month, you cannot meaningfully repair that hole.
The smart move is to assume your future self will care about:
- Any advanced laparoscopy
- Any complex vascular, transplant, or oncologic case
- Any rare or unusual scenario that stands out in your memory
You do not have to decide your entire career on day one. But you do have to protect optionality. Not tracking early is how you quietly delete options before you even know you want them.
Mistake #7: Underestimating How Fast Committees Screen You
Here is the part applicants misunderstand: your case log is often scanned, not read.
On high‑volume fellowships, reviewers may have 100+ applications for a handful of spots. No one has the time to lovingly study your entire CV. They look for quick reasons to move on.
Case logs provide those reasons in under 60 seconds:
- Total volume below their informal cutoff
- Weak index case numbers compared with their other applicants
- Messy, bulk‑entry dates suggesting reconstruction
- Role distribution that looks too passive for your PGY level

| Category | Value |
|---|---|
| CV | 90 |
| Letters | 120 |
| Case Log | 60 |
| Personal Statement | 45 |
I have sat in meetings where someone says, “Case mix is thin and log looks late—pass,” and that is the end of the discussion. No one reads the personal statement. No one debates your potential.
You never want your case log to be the easiest reason to reject you. Yet that is exactly what you create if you wait years to track your cases properly.
How To Not Make These Mistakes (Without Becoming a Spreadsheet Zombie)
Let me be practical. You do not need an elaborate, color‑coded monstrosity. You need a minimal, reliable system and the discipline to use it from the start.
1. Weekly (not yearly) logging
Once a week—pick a consistent day—you:
- Enter all cases into the official system
- Cross‑check your personal log with your OR schedule
- Correct roles (primary vs assistant) while you still remember what you actually did
This takes 10–20 minutes if you keep up with it. It takes entire weekends if you postpone it for months.
2. Quick case notes, not essays
For personally important or unusual cases, in your private log, jot:
- “PGY‑2, first time running camera on complex lap colectomy.”
- “PGY‑3, primary on open AAA under Dr. X, did anastomosis.”
- “Complication: postop bleed after redo hernia, key learning about hemostasis.”
These become gold for:
- Personal statements
- Interview stories
- Reminding attendings of your growth when they write letters
3. Early pattern checks
Every 6 months, pull your ACGME report:
- Look at total case numbers compared to your class
- Look at distribution: trauma, MIS, onc, vascular, endoscopy, etc.
- Identify categories where you are clearly thin for someone interested in a given field
Then actually do something about it. Talk to your program director, chiefs, and rotation coordinators. Swaps and adjustments are much easier in PGY‑2 than in PGY‑5.

4. Guard your integrity
Never, ever “pad” your logs:
- Do not enter cases you did not scrub into.
- Do not upgrade yourself from assistant to primary if you really were not.
- Do not copy another resident’s log structure as your own story.
Fellowship directors can smell dishonesty. And nothing kills an application faster than distrust.
Consistency, completeness, and believable growth over time are what they want to see. That only comes from early, honest tracking.
The Future: Data Will Matter Even More, Not Less
You might hope this will all relax with time. It will not.
If anything, the trend is moving toward:
- More granular operative data
- Benchmarking residents across programs by case mix and independence
- Automated cross‑checks between billing, EMR, and case logs
The residents who treat case tracking as a bureaucratic afterthought will fall further behind. The ones who treat it as part of their professional identity—as surgeons who own their outcomes and experiences—will be the ones who stand out.

| Step | Description |
|---|---|
| Step 1 | Case Performed |
| Step 2 | EMR and Billing Entry |
| Step 3 | Resident Logs Case |
| Step 4 | Program Verifies Logs |
| Step 5 | ACGME Case Report |
| Step 6 | Fellowship Application |
| Step 7 | Fellowship Committee Review |
You cannot stop that pipeline. You can only decide whether you are in control of your side of it—or whether you let the system tell a distorted version of your career.
If You Remember Nothing Else
Three points.
Start tracking from day one.
Do not wait until you “care about fellowship.” Your future options depend on data you are generating right now.Review patterns early and often.
Total volume is not enough. Case mix, role distribution, and clean, timely documentation are what make your log believable and competitive.Never rely blindly on “the system.”
EMR and ACGME logs are tools, not safety nets. Maintain your own parallel record and protect your integrity. Your fellowship application is only as strong as the story your data can actually prove.




















