
Understanding Case Volume in Plastic Surgery Residency
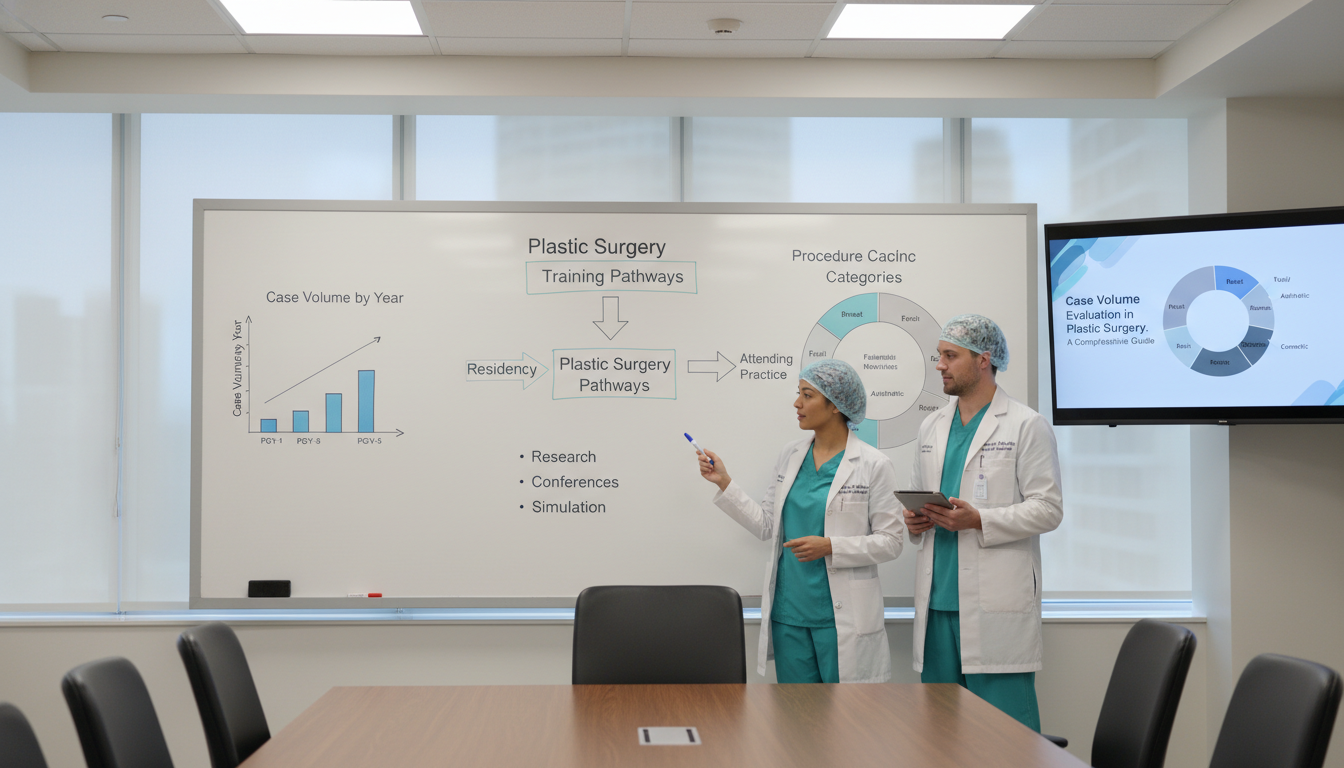
Evaluating case volume is one of the most important—and most misunderstood—parts of assessing plastic surgery residency programs. For applicants targeting an integrated plastics match, terms like “surgical volume,” “case logs,” and “procedure numbers” show up on nearly every interview day and program website. Yet few people explain how to interpret those numbers meaningfully.
This guide breaks down what case volume really means in plastic surgery residency, how it affects your training, and how to critically compare programs beyond the simple “high volume vs. low volume” label.
You’ll learn:
- What residency case volume actually measures
- How the ACGME shapes minimum procedure numbers
- Why distribution and role level matter more than raw totals
- How to ask programs the right questions during interviews and visits
- How to assess whether a program’s surgical volume fits your learning style and career goals
1. What “Case Volume” Really Means in Plastic Surgery
1.1 Basic Definitions
In the context of plastic surgery residency, case volume generally refers to:
- Number of operative cases: How many procedures you participate in as a surgeon during residency.
- Surgical volume per resident: How that total is distributed across residents, PGY levels, and rotations.
- Procedure numbers by category: How many cases you log in each required area (hand, craniofacial, microsurgery, cosmetic, etc.).
- Case complexity and role: Whether you are primary surgeon vs. first assist vs. observer, and the technical complexity of cases.
Programs may quote:
- Annual program case volume – total cases done by all residents and faculty in a year.
- Average graduating resident case volume – the typical case log for a finishing chief resident.
- Per-rotation case numbers – how many operative days/cases residents see in specific blocks (e.g., hand, craniofacial).
When you read or hear “we’re a high-volume program,” always ask: High volume for whom, and in what?
1.2 Why Case Volume Matters in Plastic Surgery
Plastic surgery is a highly technical field with a broad scope. To develop competence, you need:
- Repetition: Performing key steps of common procedures many times under supervision.
- Exposure: Seeing the range of conditions and reconstructive options in each subspecialty.
- Progression: Moving from assisting to performing as primary surgeon in a graded, stepwise fashion.
Adequate surgical volume supports:
- Strong technical skills (tissue handling, suturing, dissection, microsurgery)
- Comfort in the operating room environment and workflow
- Confidence in managing complications and unexpected findings
- A competitive portfolio for fellowships or practice
On the flip side, pure volume without structure can be problematic—if you are stuck retracting in 1,500 cases but rarely performing critical steps, your technical development may lag behind someone with fewer, better-supervised primary surgeon experiences.
2. ACGME Requirements and How They Shape Case Logs
2.1 ACGME Minimums: The Floor, Not the Ceiling
The ACGME (Accreditation Council for Graduate Medical Education) sets minimum case requirements for plastic surgery residency. These define the baseline operative exposure that every resident must achieve to graduate.
Categories typically include:
- Craniofacial (cleft lip/palate, craniosynostosis, cranial reconstruction)
- Hand and upper extremity
- Breast reconstruction and aesthetics
- Trunk and lower extremity reconstruction
- Head and neck reconstruction
- Microsurgery (free flaps, replantations, microvascular repairs)
- Aesthetic (cosmetic) procedures (face, breast, body)
Key points:
- ACGME minimums ensure breadth, not excellence. They are thresholds for adequacy, not necessarily mastery.
- Many strong plastic surgery residency programs will graduate residents well above the minimum in multiple categories.
- Meeting minimums too closely in multiple core categories can be a red flag that case volume or distribution is tight.
When evaluating a program, ask about average ACGME case numbers for recent graduates. Look for consistency—not just a single superstar graduating with huge logs.
2.2 Integrated vs. Independent Pathways and Case Volume
In the current U.S. landscape, integrated plastic surgery residency has become the dominant pathway, with independent programs (after general surgery or related training) less common.
This affects case volume trajectories:
Integrated programs:
- Early years (PGY1–2) often include general surgery, ENT, neurosurgery, orthopedic, and ICU rotations.
- Plastic surgery exposure increases progressively from PGY2–3 onward, with heavier case volume typically in PGY4–6.
- Programs vary widely in how early you get into the plastics OR.
Independent programs:
- Residents come in with prior operative experience (e.g., general surgery), and often progress faster to primary surgeon roles in plastics.
- Case logs over the plastic surgery years may be intense, but earlier foundational skills were built elsewhere.
For the integrated plastics match, pay close attention to:
- When you start logging plastic surgery cases meaningfully
- How much of your early residency is spent on non-plastics services
- Whether you get early clinic and OR exposure to build context before high-volume years

3. Beyond the Numbers: Quality, Distribution, and Role
3.1 High Volume vs. Meaningful Volume
A plastic surgery residency program that advertises “we do 2,500 cases per year” may sound appealing, but raw numbers can mask critical differences:
Questions you should be asking:
What is the average graduating resident’s total case volume?
- This is more important than the total institutional volume.
- Try to see a breakdown (or at least hear ranges) by subspecialty.
How are cases distributed between residents?
- Is there a steep hierarchy where chiefs get everything and juniors retract?
- Do mid-level residents get meaningful primary surgeon experience?
- Is there competition between residents or fellows for the “good” cases?
What is your role in the case?
- Are you usually performing the critical steps (e.g., anastomosis in a free flap, cartilage carving in rhinoplasty, tendon repair in hand trauma)?
- Or are you largely assisting while attendings or fellows do the key parts?
Example scenario:
- Program A: 1,900 logged cases per grad; strong distribution across categories; PGY-4 and PGY-5 regularly perform as primary surgeon on core reconstructive procedures and select aesthetic cases.
- Program B: 2,400 logged cases per grad, but most key portions are done by attendings or fellows until late PGY-6; juniors primarily retract and close skin.
Despite lower raw numbers, Program A may produce better-prepared independent surgeons.
3.2 Case Mix: Reconstructive vs. Aesthetic vs. Subspecialties
Plastic surgery is not a monolith. Case volume should be analyzed in terms of case mix:
Reconstructive volume:
- Trauma (hand, facial fractures, soft tissue)
- Oncologic reconstruction (breast, head and neck, sarcoma, melanoma)
- Pressure sore and wound coverage
- Microsurgery (free flaps, limb salvage)
Aesthetic volume:
- Rhinoplasty, facelift, blepharoplasty
- Breast augmentation, mastopexy, reduction
- Body contouring (abdominoplasty, liposuction, post-bariatric cases)
- Non-surgical aesthetics (injectables, lasers) – not always logged in operative case numbers but critical in practice
Subspecialty focus:
- Craniofacial (cleft, craniosynostosis)
- Hand and peripheral nerve
- Microsurgery-heavy programs (complex reconstruction, oncoplastic, lymphedema surgery)
- Burn and acute wound care
Ask programs:
- “What is the balance between reconstructive and aesthetic cases for a typical graduate?”
- “Do residents consistently meet or exceed ACGME minimums in all key subspecialties?”
- “Are there any categories where residents routinely have to work to barely meet minimums?”
3.3 Role Progression Across PGY Levels
Healthy training progression in plastic surgery residency typically looks like:
PGY-1–2:
- Foundational surgical skills (general surgery, critical care, emergency management)
- Introduction to plastic surgery: clinic, minor procedures, assisting in OR
- Learning pre-op planning and post-op care
PGY-3–4:
- Increasing responsibility in plastic surgery cases
- Performing portions of cases (e.g., raising flaps, harvesting grafts, managing donor sites)
- Beginning selected primary cases under close supervision
PGY-5–6 (Chief years):
- Leading operative planning and execution
- Performing as primary surgeon on a broad range of cases
- Managing junior residents in the OR and clinic
- Taking oversight role on call
When evaluating programs:
- Ask to see/how they describe graded autonomy.
- Ask specifically:
- “By PGY-4, what types of cases am I generally performing as primary surgeon?”
- “By chief year, what is the typical autonomy level on common procedures like breast reduction, carpal tunnel release, skin cancer reconstruction, and free flaps?”
A high case volume residency without deliberate progression in autonomy may leave you technically underprepared despite an impressive case log.
4. Evaluating Program Case Volume During the Integrated Plastics Match
4.1 What to Ask on Interview Day and Second Looks
You will not see official printed case logs for each resident at most interviews, but you can still gather meaningful data.
Targeted questions:
To Program Leadership:
- “What is the average total case volume of your graduating residents over the last 3–5 years?”
- “Are there any ACGME categories where residents occasionally struggle to reach minimums?”
- “How has your surgical volume changed over the past 3 years (e.g., new hospital affiliations, loss/gain of services)?”
To Current Residents:
- “Do you feel you get enough hands-on time as primary surgeon, not just first assist?”
- “Are there rotations that are consistently ‘overcrowded’ with residents or fellows?”
- “Is there intense competition for key cases (like free flaps, craniofacial, or cosmetic)?”
- “What does a typical OR week look like for a PGY-3? For a chief resident?”
About Case Mix and Exposure:
- “How strong is your aesthetic volume, and how is it structured (resident aesthetic clinic, private practice rotations, etc.)?”
- “Is there a resident-run cosmetic clinic where you function as primary surgeon?”
- “How frequently do residents participate in microsurgery and perform anastomoses by senior years?”
Listen for consistency across answers from different residents and faculty. Wide discrepancies may signal underlying issues with access to cases.
4.2 Using Program Websites and Public Data Wisely
Program websites vary widely in how transparently they report case volume. When reviewing online:
Look for:
- Mention of ACGME accreditation status and any recent changes.
- Comments like “Residents graduate with microsurgery volumes 2–3x ACGME minimums” or “Strong aesthetic exposure through resident cosmetic clinic.”
- Descriptions of clinical sites (academic hospitals, trauma centers, VA, private practices) that influence case mix.
Be cautious:
- Vague claims like “excellent surgical volume” or “robust operative experience” without numbers or examples.
- Heavy emphasis on research and lab time with minimal discussion of surgical volume may signal a less operative-heavy program (which may be fine if you’re research-focused—but you should know that going in).
Remember: websites are marketing tools. Use them to generate specific questions to clarify case volume during interviews.
4.3 Red Flags in Case Volume
While no single factor should “disqualify” a program, consider these as potential red flags worth exploring:
- Residents reporting they struggle to meet ACGME minimums in core categories.
- New or rapidly expanding programs with limited graduating cohorts and unclear volume data.
- Multiple residents mentioning that fellows frequently take the key parts of cases, leaving residents with limited primary surgeon experience.
- Heavy concentration of cases in one area (e.g., nearly all breast and very little hand or craniofacial) without options to supplement weak areas.
- Significant recent loss of hospital contracts, trauma coverage, or key faculty with subspecialty expertise.
None of these automatically rule out a program, but they should prompt deeper questions about how your case volume and procedure numbers would look over six years.
5. Matching Case Volume to Your Career Goals
5.1 Planning for Fellowship vs. Direct Practice
Your ideal case volume profile may differ depending on your long-term goals:
Planning for academic or microsurgery fellowship:
- Prioritize programs with:
- High microsurgical volume and routine free flap exposure
- Complex oncologic and trauma reconstruction
- Opportunities for microsurgical simulation and lab training
- Ask: “How many free flaps does a typical chief perform as primary surgeon?”
- Prioritize programs with:
Planning for craniofacial or hand surgery fellowship:
- Look for:
- Dedicated craniofacial/hand services with substantial resident involvement
- Adequate pediatric exposure if craniofacial-focused
- OR-th or hand call rotation structures that give residents early and repeated exposure
- Look for:
Planning to enter community or aesthetic-focused practice:
- Emphasize:
- Strong aesthetic surgical volume and non-surgical cosmetic training
- Resident aesthetic clinics where you lead cases under supervision
- Solid bread-and-butter reconstructive experience (breast reduction, skin cancer reconstruction, minor hand procedures)
- Emphasize:
High total surgical volume is helpful, but the proportion in your future practice areas is more important.
5.2 Balancing Case Volume With Other Training Components
Extremely high case volume programs may have:
- Longer OR days and call schedules
- Less protected research or academic time
- Fewer opportunities for away electives
Moderate volume programs may offer:
- More balanced clinical and research time
- Greater flexibility for targeted electives (e.g., away rotation at a high-volume microsurgery center)
- Potentially better lifestyle during residency
Consider your priorities:
- Do you want the busiest possible surgical training, accepting that research and personal time may be tighter?
- Or do you want balanced training with strong but not maximal volume, plus formal research or global surgery opportunities?
There is no single “best” case volume profile; it depends on your learning style, stamina, and long-term goals.
6. Practical Strategies to Assess and Optimize Your Case Volume
6.1 During the Application and Ranking Process
As you move through the integrated plastics match:
Make a structured comparison table for each program:
- Reconstructive vs. aesthetic emphasis
- Microsurgery volume (low / moderate / high, based on resident input)
- Presence of competing fellows in key areas
- Resident-reported autonomy level by PGY stage
- Any noted gaps in case categories
Weigh case volume alongside other factors:
- Mentorship quality
- Program culture and resident satisfaction
- Geographic needs (family, partner)
- Research interests and academic opportunities
Use post-interview communication wisely:
- You can sometimes clarify lingering questions with coordinators or chiefs.
- Be professional and concise; ask 1–2 targeted questions if absolutely necessary.
6.2 Once You Match: Maximizing Your Surgical Volume
Regardless of where you match, you can actively shape your residency case volume:
Know your ACGME requirements early:
- Familiarize yourself with category minimums.
- Track your cases proactively from PGY-1 or PGY-2 onward.
Seek feedback on your operative performance:
- Ask attendings which key steps you’re ready to take on in upcoming cases.
- Request gradually increased responsibility and let them know you welcome constructive feedback.
Be present and prepared:
- Read about cases the night before; understand the anatomy, indications, and steps.
- Show up early, help with pre-op marking or planning; this often leads to more intraoperative responsibility.
Collaborate with co-residents:
- Avoid competition that undermines learning; advocate for equitable distribution of key cases.
- Share opportunities (e.g., if you’re heavy in microsurgery, encourage a peer to take lead on some flaps and vice versa in other areas).
Identify gaps by mid-residency:
- If your procedure numbers are lagging in certain categories (e.g., craniofacial, aesthetics), discuss options:
- Elective rotations
- Away rotations
- Intensifying exposure in specific blocks during senior years
- If your procedure numbers are lagging in certain categories (e.g., craniofacial, aesthetics), discuss options:
Deliberate, proactive engagement can turn even a moderate-volume program into an excellent training experience for you personally.
FAQs: Case Volume Evaluation in Plastic Surgery Residency
1. What is a “good” total case volume for a plastic surgery resident by graduation?
There is no universal “magic number.” Many strong programs graduate residents with 1,500–2,500+ logged cases, but what matters more is:
- Meeting or exceeding ACGME minimums in all categories
- Having sufficient primary surgeon experience in core procedures
- Adequate exposure in areas aligned with your career goals (e.g., microsurgery, aesthetics, hand)
Ask programs for their average total and category-specific volumes for recent graduates rather than chasing a specific threshold.
2. How worried should I be if a program has strong reconstructive but weak aesthetic volume (or vice versa)?
You should consider:
- Your career goals: If you plan heavy aesthetic practice, limited cosmetic exposure is more concerning; similarly, if you plan academic microsurgery, low reconstructive volume is problematic.
- Whether the program:
- Has a resident cosmetic clinic
- Offers electives or outside rotations to supplement weak areas
- Has alumni who successfully entered your desired practice type or fellowship despite the imbalance
A program can still be excellent if it helps you strategically fill gaps.
3. Do plastic surgery fellows take away too much case volume from residents?
The impact of fellows varies greatly by institution. In some programs, fellows:
- Enhance volume by drawing complex referrals
- Teach residents and still leave them substantial primary surgeon opportunities
In others, fellows may:
- Perform most key portions of high-value cases
- Compete directly with residents for operative autonomy
Ask residents directly:
“Do you feel fellows enhance or limit your operative experience?” and
“On microsurgery/craniofacial rotations, who usually does the critical parts of the case?”
4. Is a very high-volume program always better than a moderate-volume program?
Not necessarily. Very high-volume programs can be fantastic for building technical skills, but they may also come with:
- Heavy call, longer hours, and risk of burnout
- Less scheduled research time
- Less flexibility for electives
A moderate-volume program with:
- Thoughtful case distribution
- Strong mentorship
- Good autonomy progression
- Tailored electives
can produce outstanding plastic surgeons. Evaluate fit, not just raw surgical volume.
By understanding how residency case volume, surgical volume distribution, and procedure numbers truly impact training, you can approach the integrated plastics match with a more critical eye—and ultimately choose a plastic surgery residency where you’ll develop into a confident, competent, and well-rounded surgeon.




















