
Why Case Volume Matters So Much for US Citizen IMGs
For a US citizen IMG or American studying abroad, choosing the right residency program is not just about matching anywhere—you’re building the foundation for an independent, confident clinical career. Case volume, surgical volume, and procedure numbers are central to that foundation, especially in procedural or surgical specialties.
Unlike applicants from US MD schools who often have strong built‑in networks and advisors, a US citizen IMG frequently has:
- Less direct access to US clinical training environments
- Fewer home-program advocates in competitive specialties
- More pressure to “prove” readiness for hands-on work
That makes residency case volume and quality of experience even more critical. A high-volume program that lets you actually do the work (not just observe) can:
- Compensate for a weaker clinical network
- Accelerate your technical and decision-making skills
- Make you more competitive for fellowships or jobs after graduation
At the same time, more is not always better. An extremely high surgical volume with poor supervision or chaotic systems can burn you out or leave you repeating low-level tasks. The key is learning how to evaluate case volume intelligently—beyond brochure numbers and glossy websites.
This article breaks down practical, step-by-step strategies for US citizen IMGs to assess residency case volume, interpret numbers realistically, and ask programs the questions that matter.
Understanding Case Volume: What Actually Counts?
Before you compare programs, you need clarity on what “volume” really means and what it doesn’t.
1. Core Definitions
Case volume (overall):
How many total patients or procedures are handled by the service or department (e.g., “20,000 ED visits per year” or “9,000 surgical cases per year”).Surgical volume / procedural volume:
The number of operative or interventional procedures performed (e.g., laparoscopic cholecystectomies, colonoscopies, C-sections, central lines, cardiac caths).Resident case numbers:
The number of cases/procedures each resident actually participates in and logs—this is what truly matters to you.Index/major cases vs. minor cases:
- Index/major – Core, complex, or defining procedures for a specialty (e.g., colectomies for general surgery, arthroscopy for orthopedics, PCI for cardiology fellows).
- Minor – Routine or lower-complexity cases (e.g., wart removal, simple I&D, dressing changes, basic suturing).
High program-level numbers don’t guarantee high resident numbers. You need to separate:
“How many cases does the hospital do?”
vs.
“How many cases does each resident complete as primary surgeon/operator?”
2. Volume vs. Variety vs. Responsibility
Case volume alone isn’t enough. Evaluate three dimensions together:
- Volume – How many cases.
- Variety – How many types of cases and pathologies (bread-and-butter vs. rarities).
- Responsibility – How much of the case you’re allowed to do (assistant vs. primary operator).
For a US citizen IMG, programs that offer progressive responsibility are especially valuable—places where you clearly move from:
- Observing → assisting → doing parts of the case → running full cases under supervision.
3. Minimum Requirements vs. Strong Training
Most specialties have minimum case numbers defined by the ACGME or specialty boards. For example (illustrative, not exhaustive):
- General Surgery: Specific numbers for hernia repairs, colectomies, endoscopies, etc.
- OB/GYN: Minimum vaginal deliveries, C-sections, hysterectomies.
- Internal Medicine: Procedure expectations for lines, paracentesis, thoracentesis (though more variable across programs).
Meeting the minimum is not the goal. You want a program where graduates consistently exceed those minima comfortably, without needing to scramble in their final year to fill gaps.
Where to Find Case Volume Data (and How to Read It)
Most programs will not post full resident case logs publicly, but there are many ways to approximate and cross-check surgical volume and procedure numbers.

1. Official Program and Hospital Websites
Look for:
- “By the numbers” sections
- Annual reports for the department (especially surgery, OB/GYN, EM, anesthesia)
- Clinical volume stats:
- OR cases per year
- Deliveries per year
- ED visits per year
- Outpatient visits per year
- ICU beds and admissions
Interpretation tips:
- A hospital with 10,000+ OR cases/year and a moderate program size (e.g., 3–5 residents per class in general surgery) usually indicates good surgical exposure.
- A center with high birth numbers (e.g., 3,000–5,000+ deliveries/year) and a medium-sized OB/GYN residency suggests strong obstetric volume.
- Very large resident classes with modest hospital numbers may mean diluted individual experience.
2. ACGME and Specialty Board Requirements
Check:
- ACGME specialty program requirements (publicly available).
- Any published “case minimums” or log benchmarks.
Then, during interviews or correspondence, you can ask how the program’s median graduate compares to those minima.
Example question:
“For your graduating residents, how do their typical case logs compare to the ACGME minimums—roughly what percentage above the minimum are they in core index categories?”
3. Program-Specific Presentations and Open Houses
In recent years, many programs have created:
- Virtual open house slides
- Webinar Q&A sessions
- PDF “Resident Life” or “Our Program by the Numbers” brochures
Often these will contain:
- Average procedures per resident in key categories
- Percent of residents meeting case numbers early vs. late in training
- Case volume by PGY year
As a US citizen IMG, prioritize attending these sessions and screenshot/record key data where allowed.
4. Talking to Current and Recent Residents
This is your single most reliable source of real information.
Ask targeted questions such as:
- “For your graduating class, what were your typical case numbers in [key procedures]?”
- “Did anyone struggle to meet minimum case numbers or need to add extra rotations?”
- “By what point in residency were you comfortable doing [core procedure] independently?”
- “Do juniors regularly get OR time, or is it heavily senior-driven?”
Red flags in responses:
- Vague answers: “I’m not really sure what my numbers are.”
- “We have enough cases, but staff or fellows usually do most of them.”
- “We all had to scramble in our last year to meet [particular category].”
5. Fellowship Match Lists and Alumni Careers
High-volume, high-quality training often shows up in fellowship and job outcomes:
- Graduates consistently matching strong fellowships (e.g., surgical oncology, MFM, interventional cardiology).
- Alumni working comfortably in independent practice in community settings.
If graduates are routinely sought after, it often correlates with robust training—including strong procedural experience.
Interpreting Numbers: What’s “High Volume” vs. “Just Busy”?
Not every program will give you exact numbers, but many will provide ranges or statements like “high surgical volume” or “busy trauma center.” Learn to translate that into meaningful expectations.
1. High Volume Hospital ≠ High Volume Residency
A major pitfall for US citizen IMGs is assuming that a big, famous, or “Level 1” center is automatically best for hands-on experience. Large tertiary centers often have:
- Multiple residency programs
- Numerous fellows
- Strong faculty who may do complex portions themselves
In some settings, this results in:
- Residents observing complex cases without doing much
- Fellows taking the key parts of cases
- Residents rotating on many services but doing fewer cases per block
Smaller or mid-size community-based or hybrid academic programs can sometimes provide much higher individual case numbers, especially for bread-and-butter index cases.
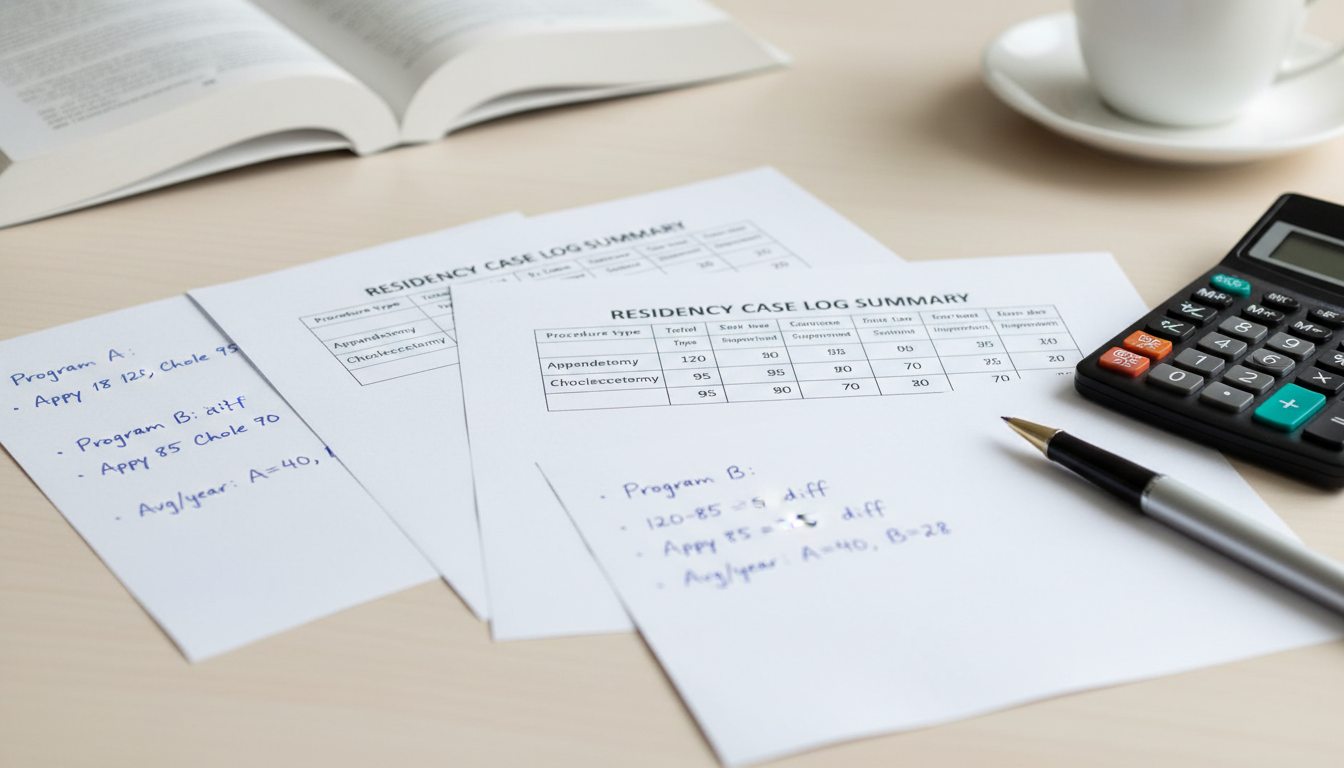
2. Watch the Ratio: Volume per Resident
When possible, estimate:
Approx. relevant cases per year ÷ number of residents on that service
Example (hypothetical):
- Hospital A: 10,000 OR cases/year, 7 residents per PGY class = 28 residents total in core general surgery.
- Hospital B: 5,000 OR cases/year, 3 residents per PGY class = 12 residents total.
Raw volume is higher at Hospital A, but Hospital B may offer more cases per resident and earlier opportunities to operate.
3. Procedural Bread-and-Butter vs. Rare Tertiary Cases
Ask about the mix of cases, not just totals:
- Are you getting a strong base in common procedures you’ll do in practice?
- Or is most of the volume highly specialized, with limited hands-on role for residents?
Examples:
- General Surgery: Are residents doing many laparoscopic cholecystectomies, hernias, appendectomies, colectomies—not just assisting on multi-visceral transplants or rare complex oncology?
- OB/GYN: Are residents routinely primary surgeon for C-sections and vaginal deliveries, not just watching complex MFM cases or fertility procedures?
4. Progressive Autonomy: When Do You Actually Get to Do Cases?
High surgical volume is only useful if you’re allowed to progress in your role:
- PGY-1/2: Suturing, basic procedures, simple cases as primary surgeon with supervision.
- PGY-3/4: Running more complex cases, leading teams, increasing independence.
- PGY-5 (for 5-year programs): Functioning almost like a junior attending under indirect supervision.
Questions to ask residents:
- “By the end of PGY-1, what procedures were you mostly comfortable doing?”
- “When did you first act as primary surgeon for [core procedure]?”
- “How are responsibilities divided between juniors, seniors, and fellows in the OR?”
If juniors are mainly retractors and seniors rarely get to operate because fellows dominate, that “high-volume” program may not translate into high resident procedural numbers.
Case Volume Strategies by Specialty (US Citizen IMG Focus)
Different specialties require different approaches to interpreting residency case volume, surgical volume, and procedure numbers. Here are strategy highlights for common IMG-friendly and IMG-challenging fields.
1. Internal Medicine
While not traditionally “surgical,” internal medicine still has important procedural skills:
- Central venous lines
- Arterial lines
- Paracentesis and thoracentesis
- Lumbar punctures (depending on practice)
- Joint aspirations/injections
What to look for:
- Presence of procedure services or ultrasound-guided procedure teams that residents staff.
- ICU structure: Are IM residents primary in the MICU, or do fellows/other services dominate?
- Simulation labs and structured procedural curricula.
Key questions:
- “Approximately how many central lines / paracenteses does a typical resident perform by graduation?”
- “Are procedures concentrated among a few residents, or fairly distributed?”
- “Who usually performs bedside procedures—residents, fellows, advanced practice providers?”
For US citizen IMGs, programs where residents perform a substantial share of these procedures build strong confidence and employability, especially if you consider hospitalist or critical-care-oriented careers.
2. General Surgery
This is where residency case volume and surgical volume are absolutely central.
Priorities:
- Total cases logged per graduating resident, especially as primary surgeon
- Case numbers in core ACGME-defined categories
- Early exposure to OR as a junior resident
- Bread-and-butter case numbers (hernia, chole, appy, breast, colon, basic vascular, endoscopy)
Key questions:
- “What is the average total number of logged cases per graduating resident?”
- “How do your residents’ case numbers compare to ACGME minimums in index categories?”
- “Do fellows ever limit resident case access? In which subspecialties?”
- “By PGY-3, what cases are residents typically running from start to finish?”
As a US citizen IMG, don’t dismiss strong community or university-affiliated community programs. These often have:
- Less competition from fellows
- High operative autonomy
- Excellent procedure numbers that surpass bigger-name centers.
3. OB/GYN
OB/GYN is highly procedure driven, both in the OR and on labor and delivery.
Key volumes to investigate:
- Annual deliveries (and C-section rate)
- Resident primary C-sections per year
- Vaginal deliveries managed per resident
- Hysterectomies (open, laparoscopic, vaginal) per resident
Ask:
- “Roughly how many C-sections does a typical graduate perform as primary surgeon?”
- “Do residents consistently exceed case minimums in hysterectomy and other core procedures?”
- “On busy nights, do residents or attendings primarily handle deliveries and cesareans?”
High delivery numbers with structured resident involvement are a strong sign of good procedural training.
4. Emergency Medicine
Emergency medicine volume is more about patient encounters and procedures in the ED:
- Annual ED visits (e.g., >70,000 often considered busy, depending on number of residents)
- Mix of trauma vs. medical vs. pediatric cases
- Procedural exposure: intubations, central lines, chest tubes, reductions, laceration repairs, pelvic exams, bedside ultrasound.
Ask residents:
- “How many intubations, chest tubes, and central lines did you log by graduation?”
- “Do you feel you had enough critical care resuscitations before finishing?”
- “Are there any procedural categories where people struggle to get numbers?”
For US citizen IMGs, EM programs with robust ultrasound training and strong trauma exposure are especially valuable for long-term versatility.
5. Anesthesiology, Radiology, and Other Procedural Fields
For anesthesiology:
- Number of intubations and airway managements
- Central and arterial line placements
- Regional blocks and neuraxial anesthesia numbers
For interventional-heavy fields (radiology, cardiology fellowship later):
- Access to interventional rotations and hands-on experience
- Balance between scanning/reading and performing procedures
Again, your main focus: Do residents get enough independent, hands-on procedural exposure before graduation?
How US Citizen IMGs Can Use Case Volume Strategically in Applications
You not only need to evaluate case volume; you should also signal to programs that you understand its importance and are actively seeking robust training.
1. Reflect Volume Priorities in Your Personal Statement
Without sounding fixated on “numbers,” you can write:
- That you value high-quality, hands-on clinical training
- That you are seeking programs where residents carry meaningful responsibility and develop procedural competence
- That your experience as an American studying abroad has shown you the importance of actively seeking opportunities to build skills
Example line:
“As a US citizen IMG, I have learned to be intentional about my training environment. I am specifically drawn to programs where resident case volume and procedural responsibility are structured to build early competence and progressive autonomy.”
2. Ask Smart, Non-Aggressive Questions on Interview Day
Good questions (adapt them to your style):
- “How does the program ensure all residents reach and exceed case minimums in key operative categories?”
- “What mechanisms do you have to identify early if a resident is falling behind in case exposure?”
- “Could you describe how operative or procedural responsibility typically changes from junior to senior years?”
These show you are serious about your training without sounding like you’re treating residency as a numbers game.
3. Use Case Volume as a Major Factor in Your Rank List
As you build your rank list, create a simple rubric that includes:
- Approximate case volume per resident (based on what you learned)
- Resident perceptions of procedural autonomy
- Balance of complexity vs. bread-and-butter cases
- Degree of competition with fellows
- Fit with your goals (community vs. academic, fellowship aspirations, lifestyle priorities)
Your final list should favor programs where you will become:
- Technically competent
- Confident managing emergencies
- Comfortable practicing independently within your specialty’s scope
This is especially crucial for US citizen IMGs who may practice in more resource-limited or community environments early in their careers.
Frequently Asked Questions (FAQ)
1. As a US citizen IMG, should I always choose the program with the highest surgical volume?
Not necessarily. Extremely high surgical volume can be a double-edged sword:
- Pros: More opportunities for repetitions, faster skill acquisition, better comfort in busy settings.
- Cons: Risk of being overworked with less structured teaching, potential for burnout, or competition with fellows limiting your role.
Your goal is not just “maximum volume” but high volume with structured teaching, progressive autonomy, and sufficient support. A mid-volume program with excellent hands-on exposure and strong mentorship may be better than a “super busy” but chaotic environment.
2. How can I compare residency case volume if programs don’t give specific numbers?
Use triangulation:
- Review hospital-level data (annual surgeries, deliveries, ED visits) and estimate per-resident volume.
- Ask residents directly about their typical case logs in key procedure categories.
- Inquire how well graduates exceed ACGME minimums.
- Look at fellowship match success and alumni comfort in independent practice.
You’ll rarely have perfect numbers, but consistent responses from multiple residents plus hospital metrics will give you a reliable picture.
3. Do community programs offer enough case volume for strong training?
Often, yes—and sometimes more than big-name academic centers. Community and hybrid programs may:
- Have high surgical or procedural volumes
- Have fewer or no fellows competing for cases
- Provide earlier autonomy, especially for bread-and-butter operations
As a US citizen IMG, do not underestimate these programs. Many produce exceptionally well-trained clinicians with excellent residency case volume and procedure numbers. Evaluate them based on actual training quality, not just prestige.
4. How should I discuss case volume concerns without offending programs?
Keep your tone focused on education and growth, not on criticizing:
- Use phrases like “training exposure,” “procedural competence,” “progressive autonomy,” and “preparing for independent practice.”
- Ask open-ended questions rather than demanding specific numbers:
- “How do you ensure residents get sufficient exposure to [procedure]?”
- “Could you describe how case assignments are structured for juniors vs. seniors?”
Most faculty respect applicants who think carefully about their education—especially when you frame it around becoming a safe, competent, and confident future physician.
By approaching residency case volume with a clear strategy—understanding what counts, where to find data, how to interpret it, and how to ask the right questions—you, as a US citizen IMG or American studying abroad, can deliberately choose programs that will truly prepare you for independent practice. Your goal is not just to match, but to train in an environment where the numbers, the teaching, and the responsibility align to build the physician you want to become.




















