78% of program directors admit they have never once clicked through the USMLE “content area” breakdown on an applicant’s Step 2 CK score report.
They still judge you by subsections. Just not the way you probably think.
Let me walk through how Step 2 CK subsections actually get used in residency selection, what triggers red flags, and where the supposed “weakness” you are obsessing over does not matter at all.
1. How PDs Actually See (and Use) Your Step 2 CK Report
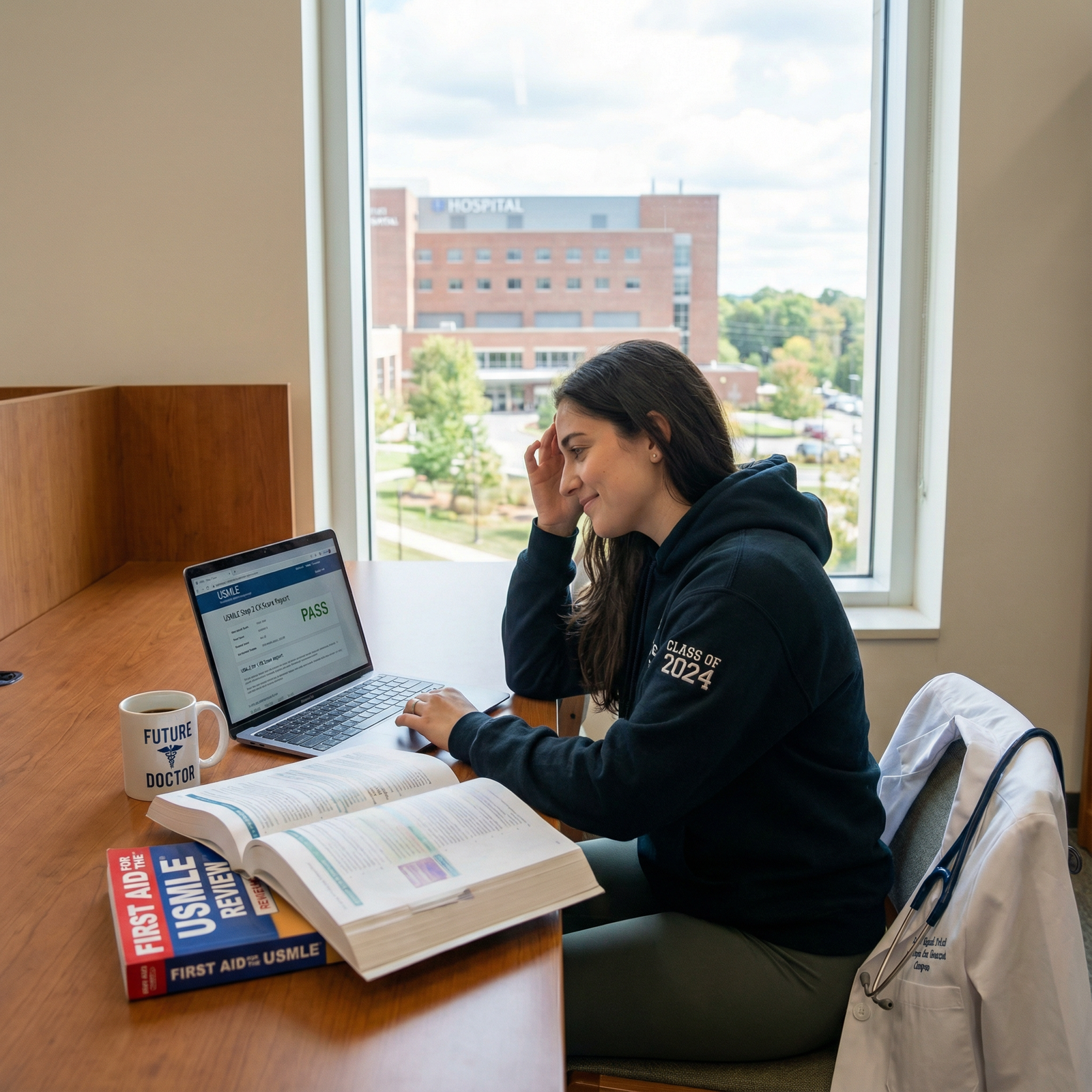
First reality check: most PDs are not sitting with the PDF of your official score report open on a big screen, zooming in on every bar graph.
Here is what usually happens in real life:
- The ERAS “USMLE transcript” shows your numeric Step 2 CK score and pass/fail.
- If anything looks off (low score, fail, big discrepancy vs Step 1, strange narrative in your personal statement), that is when someone might request or open the full official report with content areas.
At many programs, initial filters are completely blunt:
- Minimum Step 2 CK cut-off for auto-screening.
- Sometimes a higher internal threshold for interview offers than for just not rejecting.
Subscores come in later, and only when needed. Common scenarios where PDs or selection committee members actually look at subsections:
- Borderline applicant they are arguing about.
- Applicant with a fail or near-fail.
- Drastic Step 1 → Step 2 CK jump or drop.
- Someone trying to match a high-cognitive specialty with a mediocre total score.
- Concern from letters: “below expected knowledge level,” “needs closer supervision on the wards,” etc.
So your first mental correction: subsections are not part of an automated rubric. They are part of the “let me see what is going on here” deep dive.
2. What Subsections Exist – And Which Ones PDs Actually Care About
The Step 2 CK score report chunks performance into several types of breakdowns:
- Systems (cardiovascular, GI, neuro, etc.)
- Physician tasks (diagnosis, management, prognosis, health maintenance)
- Safety & professionalism style domains (often bundled together)
- Overall performance vs examinees (bars vs mean)
The shorthand interpretation PDs use is much simpler: “Can this person safely manage patients on day one, or am I taking a risk?”
So let me break down how they map these subsections to that question.

| Category | Value |
|---|---|
| Overall score | 100 |
| Diagnosis/Management | 85 |
| Systems (IM-heavy) | 70 |
| Professionalism/Safety | 60 |
| Minor systems | 35 |
| Random fine-grain bars | 10 |
Roughly speaking, that is the hierarchy. They live and die by the total score. They use subsections to confirm or challenge their gut.
2.1 Systems-Based Subscores: Internal Medicine Dominates
Let’s be honest: for most specialties, “how are they with adult medicine?” is the unspoken clinical baseline.
On the Step 2 CK report, the systems that get skimmed carefully are:
- Cardiovascular
- Pulmonary
- Renal/acid-base
- Gastrointestinal
- Endocrine
- Infectious disease
- Neurology (to a slightly lesser extent but still important)
These are seen as:
- Core physiology + pathophysiology knowledge.
- Bread-and-butter inpatient medicine.
- Real-life mortality drivers.
If you want to know what quietly reassures a PD: strong or at least solid bars in these domains, even if your overall score is just average.
Where systems matter less:
- Dermatology subscore is weak but everything else is solid? No one loses sleep.
- Musculoskeletal a bit low for someone going into psychiatry? Nobody cares.
- Reproductive / OB a bit lower for future radiology or anesthesia? Not ideal, but rarely decisive.
But if you are applying:
- IM, Cards, GI → they expect these systems to be your strength.
- EM, Anesthesia, ICU-heavy fields → cardio/pulm/renal matter a lot.
- Surgery → GI, fluids/electrolytes, perioperative medicine–related subscores matter more than random neuro minutiae.
A PD will not usually say this out loud, but several times I have seen: “Cardio and renal are both weak. I do not want this person managing pressors at 2 AM.”
That is where subscores bite you.
2.2 Task-Based Subscores: Diagnosis vs Management
This is the breakdown a lot of students misinterpret.
Those bars:
- Diagnosis
- Management
- Prognosis/Outcome
- Health maintenance/disease prevention
- Systems-based practice / patient safety
PDs mentally collapse them into two questions:
- Can this person figure out what is going on?
- Can this person do something reasonably correct once they know?
If your overall score is high (let’s say 250+), no one is panicking about a slightly lower “prognosis” bar. That is trivia compared to the core.
However, there are some patterns that do trigger discussion.
Pattern A: Diagnosis OK, Management Weak
Example: mid-230s score, diagnosis at/above mean, management well below mean.
What PDs say:
- “Good test taker but may be less decisive on the wards.”
- “Probably recognizes disease but uncertain about next steps. Might need more supervision as an intern.”
- “Will they waffle on starting antibiotics, fluids, anticoagulation?”
Programs that are high-acuity (EM, surgery, ICU-heavy IM) pay much more attention to this pattern than, say, psych.
Pattern B: Management Strong, Diagnosis Weak
Less common. But I have seen it in people who memorized guidelines and protocols.
Interpretation:
- “Probably drilled Anki and UWorld management, but misses subtle presentations.”
- “Might be fine at following standard pathways but could miss zebras and atypical cases.”
For general IM or EM, this still raises questions, but it is less damning than the reverse. You can train someone to broaden differential thinking more easily than you can teach them to actually pull the trigger on treatment decisions.
Pattern C: Both Diagnosis and Management Weak, Score Just Above Pass
Here, subsections are used to decide whether you are:
- A shaky but salvageable intern with strong work ethic and support.
- A real patient safety liability.
If both are low and there are concerning comments in MSPE, many PDs will quietly drop you down the rank list.
3. Specialty-Specific Lenses: How Different PDs Read the Same Bars
Here is where nuance matters. A neurology PD does not read your report the same way a family medicine PD does.
| Specialty | Systems Emphasized | Task Domains Emphasized |
|---|---|---|
| Internal Med | Cardio, Pulm, Renal, Endo | Diagnosis & Management |
| EM | Cardio, Pulm, ID, Trauma-ish | Rapid Diagnosis, Initial Mx |
| Surgery | GI, Renal, Fluids/Electrolytes | Periop Mx, Complications |
| Psych | Neuro, Psych domains | Diagnosis, Safety |
| Pediatrics | ID, Pulm, Development | Prevention, Management |
3.1 Internal Medicine, Cards, GI
These PDs basically live in the Step 2 CK world. They see it as “the exam that actually tests what we do.”
High attention to:
- Cardio, pulm, renal, endocrine, GI.
- Diagnosis and management. Especially management.
If you have:
- A 240+ with strong IM-relevant subscores → they are happy.
- A ~220 with weak cardio/renal and weak management → they get nervous.
Example conversation I have heard, almost verbatim:
“Her score is 225, that is fine. But cardio and renal are both way below mean, and management is low. She is going to struggle on the night float service.”
3.2 EM and Critical Care–Adjacent Fields
EM PDs love Step 2 CK more than Step 1, because it mirrors undifferentiated patients and acute decisions.
They focus on:
- Cardio, pulm, ID, trauma-relevant content.
- Rapid diagnosis, initial stabilization, and management decisions.
They do not care about your derm subscore. They care about whether you:
- Recognize sepsis.
- Know when to intubate.
- Understand DKA management.
If your management bar is low and your ID/cardio subscores are weak, they see that as “this person might not recognize or treat sick patients quickly enough.”
3.3 Surgery
Surgery PDs know Step 2 CK is not a surgery exam. But they look at it as a safety and resilience test.
They care about:
- GI, fluids/electrolytes, renal, perioperative medicine.
- Management of post-op complications.
A low total score with weak fluid/electrolyte and renal bars screams “trouble with postoperative patients.” That raises concern.
They do not obsess over psych or OB subscores. They care about whether you can:
- Manage shock.
- Correct sodium issues.
- Recognize ischemic bowel.
3.4 Psychiatry, Neurology
Psych PDs do not need you to be a nephrology wizard, but they look for:
- Reasonable neurology and psychiatric domains.
- No catastrophic weakness in basic medical management (because their patients still have diabetes, CAD, etc.).
A psych applicant with:
- Solid neuro/psych subscores and borderline renal? Usually fine.
- Weak across the board, including safety/ethics? Problem.
Neuro PDs will look a bit more closely at neuro subscores, but again, no one is using a formal equation. It is pattern recognition and gestalt: “Do these bars line up with someone I trust?”
3.5 Primary Care (FM, Peds)
Family medicine:
- Looks for reasonably balanced performance.
- Likes good health maintenance / prevention subscores.
- Worried by dramatically low management or safety bars, because they know you will be making decisions alone quickly.
Pediatrics:
- Likes strong ID, pulmonary, and developmental pediatrics.
- Does not want someone who bombs prevention/health maintenance. Vaccines, growth, development are core.
4. Red Flags vs Harmless Imperfections
Most students misclassify their own “problems.” Let’s separate signal from noise.
4.1 Things PDs Actually Worry About
I have seen these trigger real concern:
Overall Step 2 CK close to the passing line
And multiple subsections below or well below the mean in core domains (diagnosis, management, cardio, pulm, renal).Large mismatch with performance narrative
Example: stellar clinical comments, “top 10% of class,” but Step 2 CK subscores show consistent weakness everywhere. PDs question reliability of the school’s evaluations or worry about test-taking under pressure.Safety / Professionalism domain very low
When combined with concerning MSPE language (“documentation errors,” “medication errors,” “unprofessional behavior”), this is lethal. If MSPE is clean, many PDs shrug and assume test noise. But if both line up, your rank drops.Pattern of weakness matching specialty
- An EM applicant weak in cardio, pulm, ID, and management.
- A surgery applicant weak in GI, fluids, renal, and post-op–type content.
- An IM applicant weak across core medical systems and management.
This is where subtlety disappears and PDs say: “Wrong fit.”
4.2 Things Applicants Obsess Over That PDs IgnorE
Yes, ignore with a capital E.
One or two systems slightly below mean with an overall strong score.
Everyone has weak areas. No one cares that your endocrine bar was a hair lower than pulm.Slightly lower prognosis/“next best step in longitudinal care” when everything else is strong.
That domain is noisy and often driven by nuance-y questions.Minor mismatch between Step 1 organ-specific strengths and Step 2 CK subscores.
PDs typically do not cross-compare CK vs Step 1 subscores. They check total scores and maybe trends.“But dermatology is low and I am applying derm.”
Derm PDs care more about your global cognitive ability, Step scores, research, and letters. They are not combing through your Step 2 CK dermatology bar.
5. Subsections and the Story You Tell in Your Application
Where subsections actually matter for you strategically is not only how PDs read them, but how you preempt questions.
5.1 When to Proactively Address Subscore Weakness
You generally do not write, “My Step 2 CK renal subscore was low” in your personal statement. That reads as neurotic.
You do, however, consider addressing patterns when:
- You had a fail on Step 1 or Step 2 CK and then a pass with improved relevant subsections.
- A specific domain was historically weak but you built a track record of improvement (specific clerkship, shelf, or rotation feedback).
For example:
- Step 1 barely passed, low physiology/IM-related performance.
- On Step 2 CK, still not stellar overall, but IM-related subscores much improved.
- Strong IM shelf score, strong IM clerkship comments.
You can frame this as:
You recognized early knowledge gaps in core medical pathophysiology, sought structured remediation, and by the time of your IM clerkship you were consistently performing at or above your peers. That is how a PD uses subsections: as supporting evidence for your story.
5.2 Letters and Subscores: Hidden Cross-Check
Letters do not quote your Step subscores. But faculty will sometimes indirectly reference them.
Two situations I have personally seen:
Faculty on CCC/selection committee have seen your detailed Step reports internally.
They say in your letter: “Despite an early struggle with standardized exams, [Name] has demonstrated strong clinical reasoning and safe independent management on the wards.”PDs on the receiving end read that, then glance at your Step 2 CK task bars.
If diagnosis and management are at or above mean, the letter feels credible. If they are way below, the PD wonders if the letter writer is just being kind.
Your goal: align your narrative, your letters, and your subscores into a coherent picture. Not perfect, just coherent.
6. How to Use Subsections to Reassure PDs (Instead of Panicking About Them)
Let me be blunt: you cannot “spin” subsections into something they are not. But you can use them to support a credible trajectory.
6.1 If Your Total Score Is Strong But a Few Bars Are Low
Do nothing. Really.
A 250 with below-mean GI and health maintenance bars is not an issue. Programs are not reading Step 2 CK like a board certification psychometrician. They are reading for gross red flags.
If someone asks about it in an interview (rare, but it happens), a simple, confident response works:
- “I noticed that too. On practice exams my GI performance fluctuated more than other systems. I focused my third-year electives and reading on strengthening that area, especially on my IM and GI rotations.”
Short, direct, not defensive. Then move on.
6.2 If Your Total Score Is Middle-of-the-Road With Clear Strengths
Here is where you can subtly leverage subscores in interviews or PD emails.
Example: You have a 230 applying IM. Report shows:
- Above-mean cardiology, pulm, renal, ID.
- Roughly mean everywhere else.
That profile reassures PDs that, although you are not a superstar test taker, your strengths are exactly in the zones that matter for their day-to-day work. If an interviewer asks:
“How do you see your academic strengths?”
You answer:
“I am strongest in core internal medicine—particularly cardiology, pulmonary, and nephrology. That lines up with my Step 2 CK performance and the feedback I received on my IM rotation, where I was most comfortable managing complex inpatients.”
You just connected your subscores to your clinical narrative. That is exactly how PDs think, whether they phrase it this way or not.
6.3 If Your Total Score Is Borderline and Subscores Are Patchy
This is the hard zone.
You do three things:
Identify whether any pattern is clearly relevant to your chosen specialty.
Example: you are applying surgery and GI/renal/management are all low. That is a problem.Counterbalance that pattern with real-world performance.
Strong comments and concrete examples from surgery rotations, ICU, or sub-internships help. “Handled complex post-op patients independently by end of rotation.”Avoid over-explaining.
A quick, honest line if asked: “I underperformed on my Step 2 CK relative to my clinical performance. Since then, I have emphasized building reliable clinical routines and double-checking management decisions, especially in post-op care.”
PDs are not expecting you to psychoanalyze your subscores. They want to know whether you learned from a weakness or you are still in denial.
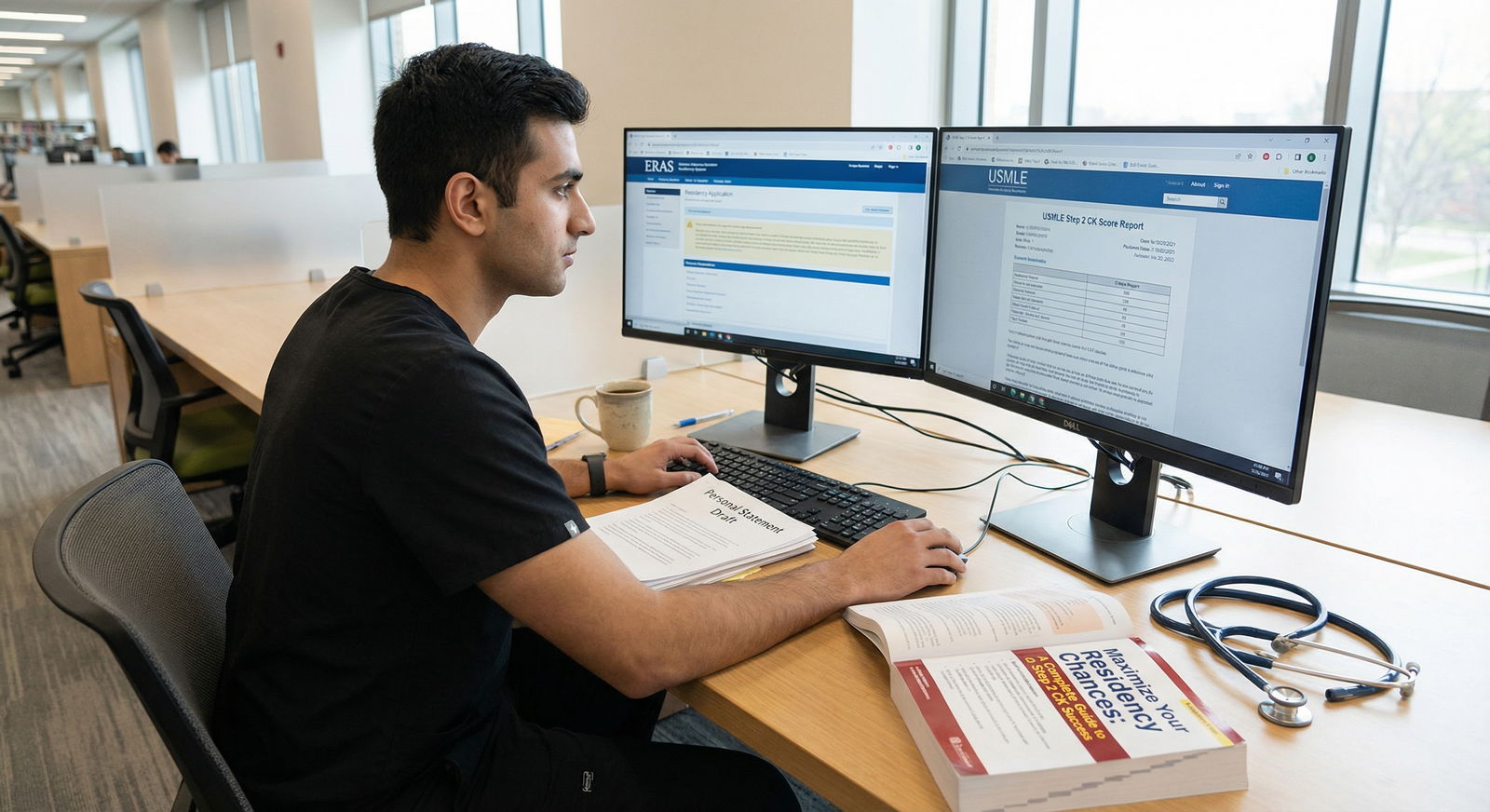
7. The Post–Step 1 Pass/Fail Era: Why Step 2 CK Subsections Matter More Now
With Step 1 now pass/fail, Step 2 CK has become the main numeric screen. That part you already know.
What is changing subtly is how much some PDs are willing to squeeze extra signal from the Step 2 CK report.

| Category | Step 1 Numeric Emphasis | Step 2 CK Emphasis |
|---|---|---|
| 2018 | 90 | 40 |
| 2019 | 92 | 45 |
| 2020 | 93 | 55 |
| 2021 | 70 | 70 |
| 2022 | 10 | 85 |
| 2023 | 5 | 90 |
A few trends I have seen in PD discussions and program meetings:
- More programs requiring Step 2 CK score before ranking, not just before starting.
- More PDs using Step 2 CK to differentiate among students from non-home or lesser-known schools.
- A bit more conversation about patterns like “good diagnosis, weak management” when they are choosing between borderline candidates.
However, even in this era, subsections are still secondary to:
- Total score.
- MSPE narrative.
- Clinical letters.
- Fit with the specialty and the program.
Subscores are used like a tiebreaker or a microscope, not like a primary filter.
8. Practical Takeaways While You Are Still a Student
You cannot retroactively change your subscores. But you can:
- Use them to direct your M3/M4 learning.
- Understand how PDs read your application.
- Decide what to emphasize in interviews, and what to leave alone.
A few very tactical uses:
You are M3, early on practice exams, and your management performance is consistently low.
Fix it now. Do targeted practice on next-step questions, guidelines, and common inpatient protocols. On the wards, force yourself to say, “My plan is…” not just “My impression is…”You are considering EM or critical care and your cardio/pulm/renal blocks are weak.
Double down there. Ask for extra time on those rotations. Show improvement feedback in your MSPE and letters.Your Step 2 CK is done, and your subsections are lopsided.
Use rotations, sub-internships, and honest conversations with attendings to build real clinical strength where the exam said you were weak. Then let your letters tell that story.

| Step | Description |
|---|---|
| Step 1 | ERAS Application Received |
| Step 2 | Hold or Reject |
| Step 3 | Check Total Score |
| Step 4 | Reject |
| Step 5 | Review MSPE and Letters |
| Step 6 | Invite to Interview |
| Step 7 | Deep Dive into Subscores |
| Step 8 | Lower Rank or Reject |
| Step 9 | Step 2 CK Available |
| Step 10 | Above Internal Cutoff |
| Step 11 | Any Red Flags |
| Step 12 | Subscores Reassuring |
That is the actual flow. Subscores get pulled when something already made someone uneasy.
9. Quick Reality Check: What To Stop Worrying About Tonight
Three things to mentally drop:
The idea that PDs have a rigid rubric for each Step 2 CK bar.
They do not. They use them qualitatively, not mathematically.The belief that one weak subsection cancels an otherwise strong application.
It rarely does. Patterns matter, not single bars.The habit of reading your subscores more obsessively than PDs do.
You have stared at your report for hours. Most PDs look for about 30 seconds, and only when there is already a question in their mind.

| Category | Value |
|---|---|
| Fail on Step 2 CK | 90 |
| Borderline overall score | 80 |
| Big Step 1 to Step 2 jump/drop | 70 |
| Concerning MSPE comments | 65 |
| Disagreement between letters and scores | 50 |
| Routine for all applicants | 15 |

Bottom Line: How To Think About Your Step 2 CK Subsections
Three core points, stripped of the noise:
PDs care 90% about your total Step 2 CK score and 10% about subsections. Subscores are a diagnostic tool for them, not the main decision driver.
The subsections that actually matter are those that map to core clinical tasks in your chosen specialty: diagnosis and management in the systems that define that field’s day-to-day work.
Use subsections to understand and improve your clinical trajectory, and to support a coherent story in your application. Do not build your anxiety around a single low bar that no one but you will ever stare at for more than a few seconds.




















