You’re halfway through third year, building your schedule for fourth year. You’re staring at that ICU elective option and asking yourself: “I’m not going into critical care. Do I actually need this, or is it just pain for no reason?”
Let me be direct: an ICU rotation is not mandatory for everyone. But for some specialties, it’s close to essential. For others, it’s nice but optional. And for a few, it’s basically low-yield unless you personally want the experience.
Here’s how to decide which group you’re in, and how much this actually matters for residency applications and the match.
1. The Short Answer: Who Really Needs an ICU Rotation?
If you want the TL;DR before the nuance, here it is.
If you’re applying to:
- Internal Medicine
- Emergency Medicine
- Anesthesiology
- General Surgery (and most surgical subspecialties)
- Neurology (especially if thinking stroke/neuro ICU)
…an ICU rotation is either very helpful or borderline expected at stronger programs.
If you’re applying to:
- Family Medicine
- Pediatrics
- OB/GYN
- Psychiatry
- Radiology, Pathology, Dermatology, PM&R
…it can still be useful, but it’s not a core requirement for most programs.
| Specialty Group | ICU Rotation Priority |
|---|---|
| IM, EM, Anesthesia | High |
| Gen Surg & Subspecialties | High |
| Neurology | Moderate–High |
| Pediatrics, OB/GYN | Moderate |
| FM, Psych, Radiology | Low–Moderate |
| Derm, Path, PM&R | Low |
Now let’s unpack why.
2. What ICU Rotations Actually Signal to Programs
Residency programs are not just asking: “Did you do ICU?” They’re reading between the lines. An ICU rotation on your transcript says a few specific things:
- You’ve seen truly sick patients.
- You’ve had to think in physiology, not just “order this test.”
- You can function (or at least survive) in a high-acuity, team-based environment.
- You’re not terrified of lines, vents, and pressors.
Those signals carry very different weight depending on your field.
For Internal Medicine
If you’re going into IM, especially at academic or tertiary-care programs, ICU experience is almost a cheat code.
Why? Because a big chunk of your residency life is either:
- Directly in the ICU, or
- Taking care of patients who are one step away from it.
Programs know PGY-1s can drown during their first ICU month. If they see an ICU elective and a strong letter from an intensivist or ICU hospitalist, that’s a plus. It says: this person has at least some idea what shock, ARDS, and multi-organ failure look like in real life.
For IM-bound students, I’d call an ICU rotation:
- Very helpful for most
- Borderline essential if you’re aiming at competitive academic IM, pulm/crit, or cards later
For Emergency Medicine
ED and ICU are cousins. Different culture, similar patients.
EM programs like applicants who know:
- How to recognize a crashing patient
- Basic vent settings and what they actually mean
- When to intubate, central line, start pressors, escalate
I’ve seen EM PDs specifically mention ICU rotations as solid prep. If you have the choice between, say, extra outpatient clinic versus ICU before an EM application cycle, pick ICU.
For Anesthesia
If you’re applying anesthesia and have zero critical care exposure, that’s a gap. Not fatal, but a gap.
You’ll eventually be managing:
- Post-op hypotension
- Vented patients in PACU/ICU
- Hemodynamics in real time
ICU gives you reps with that physiology-heavy thinking. It’s also a subtle signal that you’re not just in anesthesia for “nice lifestyle and procedures.”
For Surgery and Surgical Subspecialties
Surgeons live in the ICU more than they admit. Trauma, complex post-op, transplant, vascular — all ICU-heavy.
Surgical programs like to see that you:
- Can handle overnight calls with very sick post-ops
- Aren’t thrown by vasopressors, arterial lines, or sudden decompensation
- Know how to follow a patient after the OR, not just in the OR
If you’re pushing for competitive surgical subs (ortho, neurosurg, vascular, ENT, plastics), an ICU month somewhere in your fourth year is a strong choice.
3. When an ICU Rotation Is “Nice but Not Essential”
Now the other half of the story.
There are fields where ICU experience helps you be a better doctor, but it’s not a make-or-break for your match.
Family Medicine
Family med absolutely sees sick patients. But your core selling points as an FM applicant are:
- Breadth of care
- Continuity
- Communication and outpatient management
ICU can still help, especially if you’ll practice inpatient adult medicine or work in rural settings. But from a pure match standpoint:
- ICU is “good to have” but not necessary
- A strong sub-I in FM or IM often matters more than an ICU month
If you love acuity and want to do FM hospitalist work or work where you run codes alone at 2 a.m., then yes — do ICU. It’ll make you better. Just don’t sacrifice your key FM sub-Is for it.
Pediatrics
Peds ICU (PICU) or NICU can be amazing for those going into peds. But not every peds applicant needs it on the transcript.
Where PICU/NICU helps:
- If you’re interested in hospitalist peds, critical care, neonatology, heme/onc
- If you want a standout letter from a peds intensivist at a strong children’s hospital
But for a general peds match, it’s more “strong elective” than “requirement.” Solid inpatient peds, a peds sub-I, and continuity clinic matter more.
OB/GYN
OB does see critically ill patients: massive hemorrhage, preeclampsia with severe features, septic post-op, etc. But most OB programs aren’t scanning for “ICU rotation” as a checkbox.
What might be higher yield:
- OB/GYN sub-I at a place you want to match
- MFM or gyn onc elective
If you have room, an MICU or SICU month can help with your comfort in managing very sick peripartum patients. It’s just not the main currency of your application.
Psychiatry, Radiology, Pathology, Derm, PM&R
Let’s be blunt: for these fields, an ICU rotation is not high-yield from a match perspective.
Can it still make you a more complete physician? Sure.
Will a derm PD care that you managed refractory septic shock? Not really.
For these specialties, the opportunity cost matters more: you’re often better off doing:
- Psych: strong psych sub-Is, CL psych, addictions
- Radiology: advanced imaging, IR exposure
- Path: surgical path, autopsy path
- Derm: dermatopathology, outpatient derm electives
- PM&R: inpatient rehab, sports, pain
You won’t be penalized for having ICU, but it won’t move the needle as much as a targeted elective in your field.
4. How Programs Actually View ICU in the Application
Let’s talk practical match impact. No theory.
Programs mainly notice ICU in three ways:
- It shows up as an elective on your transcript.
- It generates a letter of recommendation.
- You talk about it meaningfully in your personal statement or interviews.
If all you did was show up, pre-round, copy notes, and avoid procedures, it’s just another line item. Neutral impact.
If you:
- Took responsibility for a few complex patients
- Presented confidently
- Showed up early, owned data, followed up plans
- Asked smart questions instead of hiding
…then ICU can turn into one of your strongest letters.
Letters from ICU Attendings
For IM, EM, anesthesia, and surgery, a strong ICU letter can be gold. Why?
Because these attendings can say very specific things:
- “Handled high-acuity patients with maturity.”
- “Functioned at or above intern level by end of rotation.”
- “Strong grasp of hemodynamics and ventilator management for a medical student.”
Those lines land well with PDs who know how rough ICU can be. If you’re going into a field where this matters, think strategically: do ICU early enough that you can request a letter for ERAS.
5. Choosing Between ICU and Other Electives
You’re not deciding in a vacuum. You’ve got limited fourth-year slots. So you’re often choosing:
- ICU vs. a sub-I
- ICU vs. a home/away elective in your specialty
- ICU vs. something that gives you lifestyle/sanity before residency
Here’s a simple decision view.
| Situation | Better Choice (Usually) |
|---|---|
| Need a strong letter in your specialty | Sub-I in that specialty |
| Already have 2 strong specialty letters | ICU or high-yield elective |
| Applying IM/EM/Anesthesia/Surgery | ICU strongly recommended |
| Burned out heading into apps | Lighter but still relevant elective |
| Weak inpatient confidence | ICU or inpatient sub-I |
6. What You Actually Learn On ICU That Helps Anywhere
Even if you never set foot in an ICU again, the skills you pick up are not niche.
You’ll get:
- A deeper sense of physiology: fluids, shock, acid-base, respiratory failure.
- Better comfort with sick patients and end-of-life conversations.
- Hands-on practice with structured presentations and daily planning.
Those things translate into:
- Stronger performance on medicine/surgery sub-Is
- More convincing interview stories (“Tell me about a challenging clinical situation…”)
- Less terror on your first intern night float
This is why I still think an ICU month is underrated even for people not doing critical care. Not mandatory, but underrated.
7. A Simple Framework: Should You Do an ICU Rotation?
Use this quick mental flow (and be honest):

| Step | Description |
|---|---|
| Step 1 | Choose ICU? |
| Step 2 | ICU strongly recommended |
| Step 3 | Do targeted elective first |
| Step 4 | ICU is good choice |
| Step 5 | Choose lighter or interest elective |
| Step 6 | Field uses high acuity often |
| Step 7 | Need targeted elective for match |
| Step 8 | Want ICU skills/experience |
If your future day-to-day will regularly involve:
- Unstable vitals
- Pressors, vents, codes
- Post-op management
Then yes, you should do ICU, even if you’ll never formally be a “critical care doctor.”
If not, ask yourself two questions:
- Will ICU boost my application more than a focused specialty elective?
- Do I actually want the experience, or am I just doing it because I feel guilty if I don’t?
If the answer to both is “no,” you’re not committing a career crime by skipping ICU.
8. Timing: When to Schedule ICU Relative to ERAS
If you’re going to do it, timing matters.
- Ideal for letters: Late MS3 or early MS4 (before ERAS opens).
- Ideal for skills/confidence: Before your heavy sub-I’s or acting internships.
- Avoid if you’re on fumes: Right next to Step 2 or peak interview season.
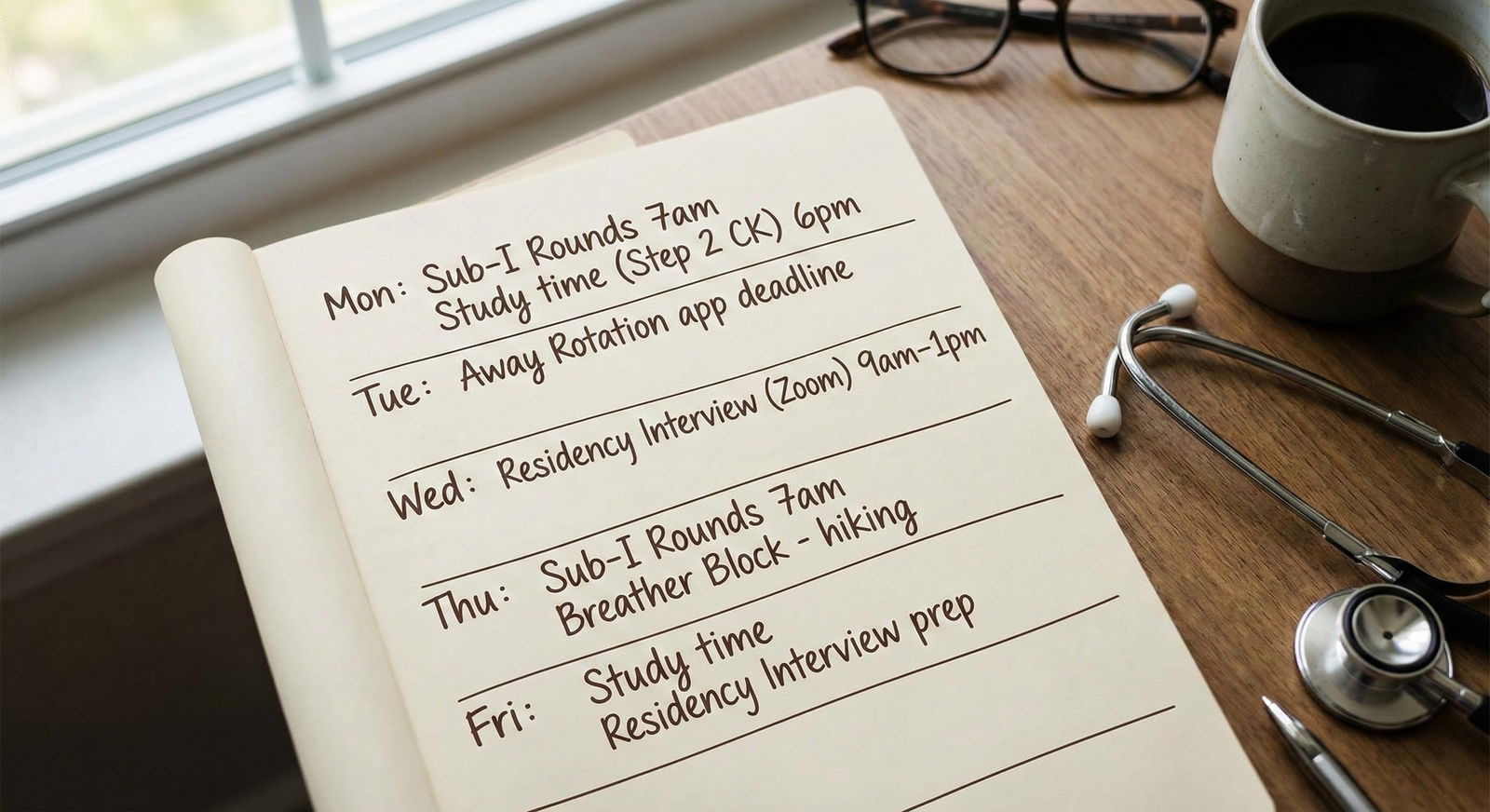
Here’s a rough sketch of how some students plan it out:

| Task | Details |
|---|---|
| Early MS4: ICU Rotation | a1, 2025-07, 4w |
| Early MS4: IM Sub-I | a2, 2025-08, 4w |
| Application Time: ERAS Submission | milestone, 2025-09-01, 1d |
| Application Time: Specialty Elective | a3, 2025-09, 4w |
| Later MS4: Interviews | a4, 2025-11, 8w |
If you can line it up so you finish ICU, get a strong letter, and roll that momentum into your sub-I and ERAS, that’s ideal.
9. Common Mistakes Students Make With ICU
I’ve watched a lot of students fumble this rotation. A few patterns:
- Treating ICU as pure shadowing. If you hide behind residents, nobody remembers you enough to write a useful letter.
- Going in completely unprepared. You do not need to be an expert, but at least skim shock, vent basics, and sepsis before day one.
- Doing ICU too late. A November ICU rotation is great prep for residency, but useless for your ERAS letters.
- Taking ICU instead of a crucial sub-I. If you’re missing a home sub-I in your chosen specialty, that’s almost always higher priority.

| Category | Value |
|---|---|
| IM/EM/Anes/Surg | 90 |
| Neuro/Peds/OB | 70 |
| FM/Psych/PMR | 50 |
| Derm/Rad/Path | 30 |
10. Bottom Line: How Important Is ICU If You’re Not Doing Critical Care?
Important for many. Required for some. Optional for others.
The better question is:
“How much will this specific ICU rotation improve my skills, confidence, and application compared to the other ways I could spend that month?”
If you’re headed into a high-acuity field — IM, EM, anesthesia, surgery — the answer leans strongly toward: “A lot.”
If you’re headed into lower-acuity or highly specialized fields, it’s more about personal growth than match necessity.
FAQs
1. Will not doing an ICU rotation hurt my chances for Internal Medicine?
If you have strong IM sub-I evaluations and letters, skipping ICU will not automatically sink you. But at more academic or critical care–heavy programs, an ICU month is a noticeable plus. If you’re choosing between random outpatient electives and ICU, pick ICU.
2. Is SICU better than MICU for residency applications?
For surgery-bound students, SICU or trauma ICU can be slightly more aligned. For IM/EM/anesthesia, MICU is perfectly fine and often more representative of what you’ll see. Program directors are not splitting hairs here; they just want to see high-acuity exposure somewhere.
3. Can I get a strong letter from an ICU rotation as a student?
Yes, if you act like part of the team instead of a visitor. Take ownership of a small number of patients, know their data cold, follow through on tasks, and show up consistently. Then ask a faculty member who has actually seen you work to write the letter before the rotation fades from memory.
4. How tough is an ICU month compared to other electives?
It’s usually one of the more demanding rotations: earlier starts, more complex patients, emotionally heavy cases, and less downtime. It’s not a “coast before graduation” month. Plan your schedule so you’re not stacking ICU right after Step 2 or right before interview season if you’re already exhausted.
5. If I’m going into Family Medicine, is inpatient medicine enough or should I add ICU too?
If you can only choose one, do an inpatient IM sub-I. That’s higher yield for FM. If you have room, adding ICU on top of that is excellent prep, especially if you want to do hospitalist work or rural FM where you’ll see sicker patients more often.
6. Does an ICU rotation help with Step 2 or just real-world practice?
It helps more with real-world practice and clinical reasoning than the exam itself. You’ll solidify concepts around shock, respiratory failure, sepsis, and acid-base that do show up on Step 2, but the main benefit is comfort with complexity, not raw test scores.
7. What should I read before starting an ICU rotation?
Keep it simple and focused. A pocket ICU handbook, quick reviews on shock, sepsis, ventilator basics, and electrolyte/acid-base management. Skim those before day one and then keep reading about your own patients each night. That patient-centered reading is what actually sticks.
Key points:
- ICU is high-yield for IM, EM, anesthesia, and surgery; helpful but not mandatory for most other fields.
- Its value depends less on the name of the rotation and more on what you do with it — responsibility, performance, and the letter it generates.
- Do not sacrifice a crucial sub-I in your chosen specialty for ICU, but if you can fit both, ICU will make you a stronger, more confident intern.






















