
The worst sub‑I mistake is simple: stacking it next to the wrong rotation and showing up tired, rusty, or totally unprepared.
You’re not just picking “what sounds interesting.” You’re picking the rotation that sets up the most important audition of your M4 year.
Let me give you the answer first, then the nuance.
The Short Answer: What Should Be Right Before Your Sub‑I?
Here’s the clean, no‑nonsense hierarchy for what to schedule immediately before your sub‑I in your target specialty:
- Best choice: A lighter but clinically similar rotation that sharpens the same skills
- Example: IM sub‑I coming up → do outpatient IM, hospitalist medicine, or a “ward‑lite” IM elective.
- Second best: A directly related core clerkship you want to refresh
- Example: Surgery sub‑I coming up → do a solid general surgery or surgical subspecialty month.
- Acceptable: A non‑clinical/light rotation (research, reading elective) if you’re already sharp and you will actually prep hard.
- Worst choice: Heavy, unrelated, or night‑float‑style rotations that leave you sleep‑deprived and rusty in the skills you’ll be judged on.
That’s the principle. Now let’s walk through the actual decision‑making for the major specialties.
Step 1: Know What Your Sub‑I Is Actually Testing
Sub‑Is are not just “harder clerkships.” They test a different layer:
- Can you carry 4–6 patients like an intern?
- Can you write full, accurate notes quickly?
- Can you run a call night without falling apart?
- Can you communicate clearly with nurses, consulting teams, and families?
- Can you present on rounds without getting lost?
So the pre‑sub‑I rotation should do at least two of three things:
- Keep your clinical reasoning sharp in that domain.
- Let you practice intern‑level workflows (pre‑rounding, notes, orders).
- Preserve your sleep and energy so you can ramp up, not crawl in.
Think in those terms and the right answer becomes obvious.
Internal Medicine Sub‑I: What To Put Right Before
If you’re aiming at IM, cards, heme/onc, pulm/crit, etc., your IM sub‑I is prime real estate. You need to look like an almost‑intern.
Best rotations to put directly before:
Outpatient Internal Medicine / Primary Care Clinic
You see bread‑and‑butter IM, you practice assessment and plan, and your hours are usually humane. You walk into your sub‑I with your “IM brain” heated up but not burned out.Hospitalist / Ward Medicine Elective (non‑sub‑I)
Same environment, lower stakes. You can practice notes, managing cross‑cover issues, thinking through admissions. Just be sure it’s not a hidden sub‑I with brutal call.Cardiology, Pulm, or ID Ward Elective
Better if your sub‑I is on the same service style. For example, cards elective → cards sub‑I. You’ll feel more fluent in that service’s language and expectations.
Rotations I would not put immediately before an IM sub‑I:
Surgery, OB, or hard ICU (if they’re known for killing your sleep)
You’ll show up to IM exhausted, slightly “surgical” in your notes, and foggy on the IM workup for common issues.Unrelated heavy subspecialties such as Neuro or Ortho if they run you like a sub‑I themselves. Great for learning, bad timing right before your audition.
Surgery Sub‑I: What To Put Right Before
Surgery sub‑Is are brutal enough. You do not want to walk in with soft hands and slow notes.
Best rotations right before:
General Surgery or Surgical Subspecialty (non‑sub‑I)
Vascular, colorectal, acute care surgery. You’ll get your OR rhythm back: scrubbing, presenting, pre‑ and post‑op management. You strengthen your hands and your pre‑rounding habits.Surgical ICU (if it’s well‑run and educational)
Good if you’re going into surgery and the SICU team actually teaches. You’ll sharpen fluid management, pressors, vents. Just make sure the call schedule doesn’t destroy you.Surgical Oncology, Trauma (if moderate hours)
These can be great if they approximate intern responsibilities but don’t demand 100% of your reserves.
Rotations to avoid immediately before a surgery sub‑I:
Inpatient IM with long call right before a gen surg sub‑I
You’ll be clinically sharper, but your OR muscle memory (sterile field, basic suturing, instrument names) will be rusty.Something super light + totally non‑clinical
If you haven’t been in an OR for 6 months, jumping straight into a surg sub‑I is an avoidable pain.
| Target Sub‑I | Strong Pre‑Sub‑I Choice | Risky Pre‑Sub‑I Choice |
|---|---|---|
| IM | Outpatient IM clinic | Night float ICU |
| Surgery | Gen surg elective | Heavy inpatient psych |
| Pediatrics | Outpatient peds/clinic | Vascular surgery |
| OB/GYN | L&D elective | Research month with no call |
| EM | ICU or IM wards | Radiology with very light load |
Pediatrics, OB/GYN, EM: How To Time It
Pediatrics Sub‑I
For a peds sub‑I (wards or NICU):
Best pre‑sub‑I: Outpatient peds, peds subspecialty clinic, or peds ED
Keeps dosing, vaccine schedules, and developmental milestones fresh while protecting your energy.Second best: Adult IM wards
Less ideal but still good. Reasoning is similar; you’ll just have to recalibrate doses and age‑specific stuff the first few days.
Avoid: heavy surgical months just before. Completely different muscles.
OB/GYN Sub‑I
For OB‑heavy or Gyn‑heavy sub‑Is:
Best pre‑sub‑I: L&D elective, Gyn Onc, or REI clinic
You want to be comfortable with triaging labor patients, OB H&Ps, and postop Gyn complications. A focused exam and presenting pattern matters here.Reasonable: IM or EM if they’re not brutal
You’ll at least be fluent in vitals, differential, and acute management.
Avoid: anesthesiology with very light clinical responsibility if it dulls your floor skills entirely.
Emergency Medicine Sub‑I / Acting Internship
EM is a bit different because you need fast decision‑making and broad differential muscle.
Best rotations directly before:
ICU (MICU, SICU, or PICU) with decent teaching
You’ll see sick patients, work on airways, vents, and resuscitation logic. Perfect warm‑up.Inpatient IM or Hospitalist service
You’ll get good at admissions, cross‑cover issues, and communicating plans clearly to consultants.Urgent care / EM elective (non‑sub‑I)
You practice speed and triage without the full pressure of the audition.
Avoid:
- Back‑to‑back EM sub‑I style months
Two EM sub‑Is in a row is a burnout trap. You’ll be slower, crankier, and less sharp on the second one—usually the one that counts more.
Hidden Variable: How Rusty Are You Right Now?
Your current state matters more than ideal theory.
Ask yourself three blunt questions:
- When was the last time you were on a busy inpatient service in this specialty or nearby?
- How did you feel on your last similar rotation—overwhelmed or comfortable?
- Do you need more reps or more rest?
If you’re:
Rusty on basics (writing notes, presenting, orders):
Do a directly related core or elective right before.Clinically fine but exhausted and cynical:
Do a lighter, related elective (clinic, consult, non‑sub‑I wards) that keeps your skills warm but lets you sleep.Very confident and fresh off a related month:
You can afford a read/research/light month right before, but only if you’ll actually use that time to prepare (reading institution guidelines, reviewing common cases, etc.).

| Category | Value |
|---|---|
| Clinical Skill Match | 40 |
| Workload/Hours | 30 |
| Timing with Auditions | 15 |
| Personal Weaknesses | 15 |
What About Letters of Recommendation?
This is the part people overcomplicate.
Your pre‑sub‑I rotation can be with someone you want a letter from, but do not sacrifice:
- Similar clinical environment
- Reasonable workload
- Skill alignment
…just to chase a letter. The best letters almost always come from:
- Your sub‑I attending in your target specialty
- Another sub‑I or audition in that field
- A mentor who’s seen you over time (research, longitudinal clinic)
If aligning your pre‑sub‑I with a letter writer also gives you the right kind of experience, great. If not, pick the better prep rotation and find a letter elsewhere during the year.
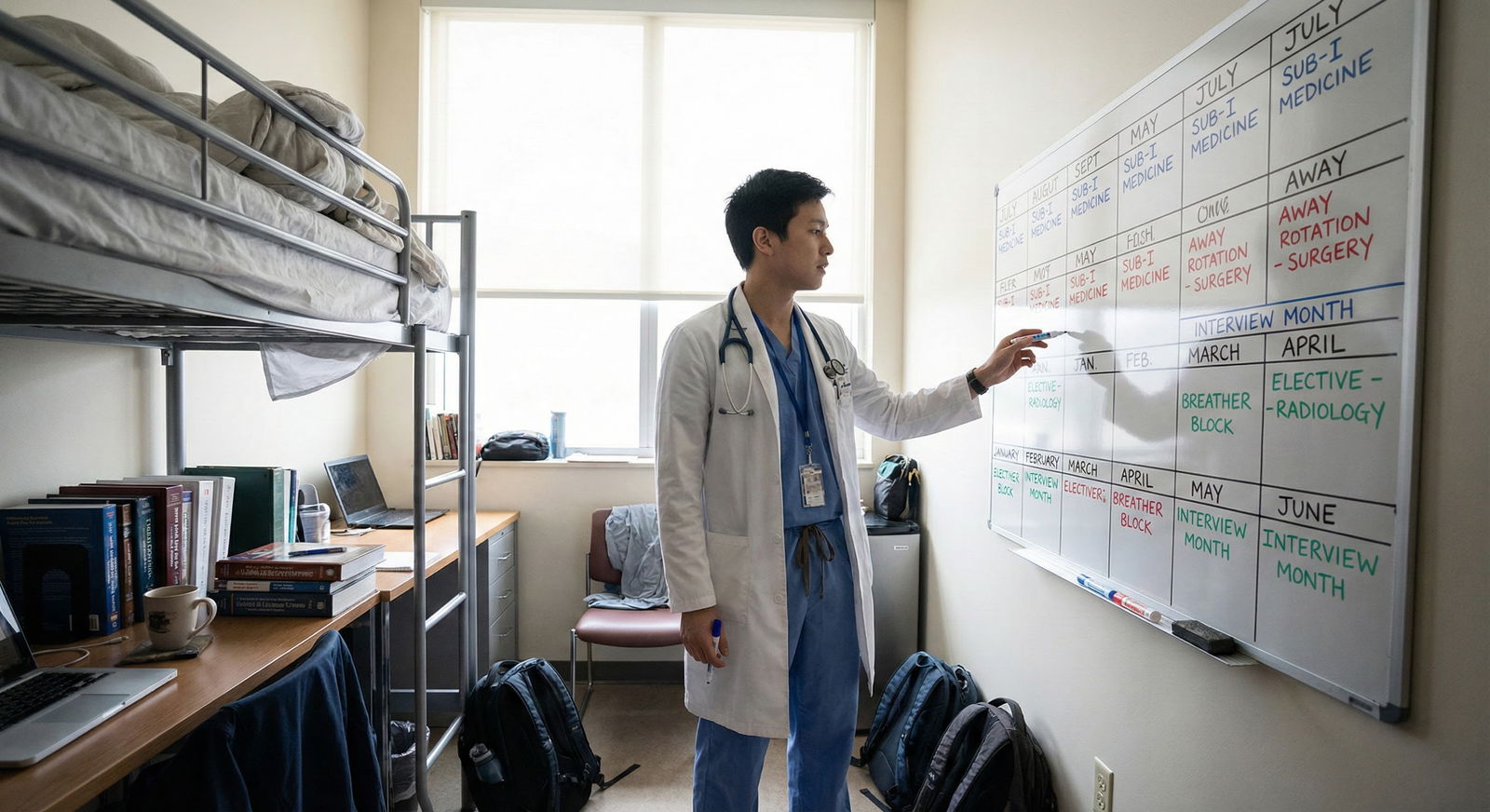
How To Sequence Multiple Sub‑Is And Pre‑Sub‑Is
The messier scenario: you’re doing 2–3 sub‑Is and trying to stack them intelligently with ERAS and interview season.
General sequencing rules:
- Do your most important sub‑I early enough for letters (June–September for most fields).
- Do its “prep” rotation immediately before, not 3 blocks earlier.
- Don’t do back‑to‑back high‑intensity inpatient months more than twice. Burnout will show in your evaluations.
A very common, actually workable pattern for IM‑bound students:
- Block 1: Outpatient IM (prep)
- Block 2: IM sub‑I at home
- Block 3: ICU elective (letter #2 source)
- Block 4: Away rotation / audition (if needed)
For surgery‑bound:
- Block 1: General surg elective (prep)
- Block 2: Surgery sub‑I at home
- Block 3: SICU or trauma (letter #2)
- Block 4: Away rotation in target program

Common Dumb Mistakes To Avoid
I’ve watched people tank their best chance at a strong sub‑I by:
- Doing night float ICU immediately before a heavy ward sub‑I. They showed up destroyed.
- Taking a 3‑month research block then walking straight into a surgery sub‑I. Their first week was just relearning how to pre‑round.
- Stacking three “auditions” in a row (Sub‑I → Away → Another Away). By the third, their speed and attitude nosedived.
- Picking a totally unrelated “fun” elective—then cramming like crazy the weekend before because they realized how rusty they were.
You do not get extra points for suffering. You get points for being sharp, reliable, and pleasant to work with.
How To Decide If You’re Stuck Between Two Options
If you’re down to two realistic pre‑sub‑I choices, run this quick tiebreaker:
- Which rotation will give you more practice with the exact patients and notes you’ll see on sub‑I?
- Which rotation has more humane hours so you won’t start sub‑I at 30% battery?
- Which attending/team is more likely to teach and give feedback, not just use you as free labor?
If one wins on at least 2 out of 3, pick it. Stop overthinking.

| Category | Value |
|---|---|
| Clinical Similarity | 90 |
| Hours/Workload | 70 |
| Teaching Quality | 80 |
Quick Specialty‑By‑Specialty Cheatsheet
Not universal, but this works for most programs.
Planning an IM Sub‑I:
Best pre‑sub‑I = outpatient IM or non‑sub‑I ward/hospitalist month.Planning a Surgery Sub‑I:
Best pre‑sub‑I = general surgery elective or moderate‑intensity surgical service.Planning a Peds Sub‑I:
Best pre‑sub‑I = outpatient peds or peds subspecialty clinic.Planning an OB/GYN Sub‑I:
Best pre‑sub‑I = L&D or Gyn service with good exposure to triage and postop care.Planning an EM Sub‑I:
Best pre‑sub‑I = ICU or inpatient IM with active cross‑cover and admissions.
FAQs
1. Should I schedule a vacation or non‑clinical month right before my sub‑I?
If you’re already clinically sharp in that field, a light month before can help you rest and prep. But be honest: if you’ve been off the wards for a while, it’s risky. A better compromise is a lighter related elective—clinic or consult—so you maintain clinical rhythm while avoiding burnout.
2. Is it bad to do my sub‑I right after a Step 2 study period?
Not automatically, but you’ll be mentally tired and clinically rusty. If that’s your situation, front‑load 3–5 days of “clinical boot camp” reading—guidelines, sample notes, common presentations—so you’re not relearning everything on day one. If you can wedge in a short related elective between Step 2 and the sub‑I, even better.
3. Can I use the pre‑sub‑I month to get a letter of recommendation too?
Yes, but do it only if that rotation still fits the three priorities: similar clinical environment, manageable workload, and actual teaching. A lukewarm letter from a random subspecialty because you looked exhausted is worse than no letter from that person.
4. What if my school’s scheduling system forces a terrible rotation right before my sub‑I?
Then you mitigate. Protect your sleep as much as possible, front‑load some review reading, and try to give yourself at least a weekend buffer before the sub‑I starts. Also, tell your sub‑I senior honestly on day one: “I just came off a brutal month but I’m ready to work; if you see gaps, I’d appreciate direct feedback.” That humility + effort combination helps.
5. Does it actually matter if the pre‑sub‑I is in the same specialty, or just inpatient vs outpatient?
For most people, same specialty helps more than inpatient/outpatient category. An outpatient IM month before an IM wards sub‑I is usually more useful than inpatient neuro, even though both are “inpatient.” The clinical reasoning and language alignment matter more than the physical location.
6. How many sub‑Is should I do total for residency applications?
Most competitive applicants do 2–3 real sub‑Is: one home in their target specialty, sometimes one away in that specialty, and one more in a closely related area (ICU for EM, IM for cards, etc.). Do not fill your entire year with sub‑Is. Two high‑quality, well‑timed sub‑Is where you perform at your best are more valuable than four where you’re exhausted and mediocre.
Key takeaways:
- The best rotation right before your sub‑I is light‑to‑moderate intensity, in or very near the same specialty, and lets you sharpen exactly the skills you’ll be evaluated on.
- Avoid walking into a sub‑I straight from an unrelated or brutally exhausting month; your evaluations will quietly reflect that.
- Sequence your pre‑sub‑I with one simple goal: show up to that audition month rested, clinically fluent, and ready to work like an intern.






















