
In a competitive and rapidly changing healthcare system, salary considerations play a real and practical role in Specialty Selection. Passion for patient care is essential, but understanding Physician Earnings across different Healthcare Professions helps you make informed decisions about training length, lifestyle, and long‑term financial health.
This expanded guide explores the most profitable Medical Careers today, what drives those incomes, and how medical students and residents can strategically position themselves—without losing sight of fit, fulfillment, and burnout risk.
Understanding How Physician Earnings Are Determined
Before comparing “highest paid specialties,” it helps to understand why some fields consistently sit at the top of salary surveys while others lag behind. Physician Earnings reflect a complex mix of market forces, training demands, and practice realities.
Key Drivers of Medical Salaries
Specialty Demand and Workforce Shortages
- High demand + limited supply = higher pay.
Fields with too few specialists to meet population needs command premium compensation. - Examples:
- Psychiatry in many regions due to mental health provider shortages
- Interventional cardiology because of aging populations and high cardiovascular disease burden
- Anesthesiology and radiology in areas with expanding surgical volumes
- In some specialties (e.g., primary care in rural areas), hospitals and health systems offer sign-on bonuses, loan repayment, and retention incentives to attract clinicians.
- High demand + limited supply = higher pay.
Geographic Variation and Market Dynamics
- Urban vs. rural:
- Urban academic centers may pay less in base salary but provide prestige, research opportunity, and strong benefits.
- Rural or underserved areas often offer significantly higher salaries, relocation incentives, and leadership roles—especially in procedural specialties and emergency medicine.
- Regional cost of living:
- A $450,000 salary in a low-cost state may go further than $550,000 in a high-cost coastal city.
- Residents should research regional compensation data (e.g., MGMA, Doximity, Medscape) when considering job offers.
- Urban vs. rural:
Experience and Career Stage
- Early-career physicians (years 1–3 in practice) often:
- Start below the average salary
- Have productivity guarantees or RVU-based compensation with a ramp‑up period
- Mid-career and senior physicians often:
- Negotiate improved contracts
- Build referral bases, reputations, or niche expertise
- Add administrative or leadership stipends (e.g., medical director roles)
- Early-career physicians (years 1–3 in practice) often:
Workload, Call, and Procedure Intensity
- Specialties with:
- Frequent night/weekend call
- Long and unpredictable hours
- High procedural volume or emergency cases
…often have higher compensation to reflect that intensity.
- Examples: trauma surgery, interventional cardiology, neurosurgery, emergency medicine.
- In contrast, specialties with more predictable hours (e.g., dermatology, some radiology models) may offer slightly lower average pay but strong lifestyle benefits.
- Specialties with:
Practice Type and Compensation Model
- Employed model (hospital/health system):
- Steady salary and benefits
- Potential RVU or quality bonuses
- Less financial risk, less autonomy over business decisions
- Private practice or group practice:
- Higher earning potential via ownership and profit sharing
- Responsibility for overhead, staffing, billing, and business development
- Hybrid models:
- Academic physicians with side income from consulting, speaking, or private practice work
- Locum tenens with flexible, often high hourly rates but fewer long‑term benefits
- Employed model (hospital/health system):
Fellowships and Subspecialization: The Pathway to Higher Income
Many of the highest-paying specialties are not just residencies—they are fellowship-trained subspecialties.
- Why fellowships increase Physician Earnings:
- Enhanced procedural skills (e.g., interventional cardiology, GI advanced endoscopy, interventional radiology)
- Scarcer, highly specialized expertise
- Ability to bill for complex, high-RVU procedures
- Trade-offs:
- Additional 1–3+ years of training
- Delayed attending-level salary
- Potential for more intense or irregular hours
For students and residents interested in top-tier earning potential, understanding the landscape of subspecialty fellowships is crucial during Specialty Selection.
The Most Profitable Medical Specialties Today
Compensation varies year to year and by data source, but the specialties below consistently appear among the highest paid in national physician compensation surveys. Figures given are approximate U.S. averages and can vary substantially by region, practice type, and experience.

1. Orthopedic Surgery
Approximate Average Salary: ~$650,000+
Orthopedic surgery frequently tops the list of highest-paying Healthcare Professions. Orthopedists diagnose and treat musculoskeletal conditions ranging from trauma to sports injuries to degenerative joint disease.
Why earnings are high:
- High volume of procedures (joint replacements, arthroscopies, fracture repairs)
- Aging population with rising rates of osteoarthritis and fractures
- Elective surgeries can be scheduled efficiently and are well-reimbursed
- Opportunities for subspecialization (e.g., spine, sports medicine, hand surgery) at even higher earning tiers
Lifestyle and practice considerations:
- Pros:
- Technically engaging, procedure-heavy work
- Clear, often rapid functional outcomes for patients
- High income ceiling, particularly in private practice or group practice
- Challenges:
- Long years of training and physically demanding work
- Frequent call for trauma and emergencies
- Risk of musculoskeletal strain and operating-room fatigue over time
For residents, early exposure to orthopedic surgery, strong Step/COMLEX scores, and high clinical performance are key to matching into this competitive field.
2. Cardiology
Approximate Average Salary: ~$600,000 (often higher for interventional cardiology)
Cardiology remains one of the most sought-after high-paying specialties due to the prevalence and severity of cardiovascular disease.
Subspecialty tracks include:
- Interventional cardiology – catheter-based interventions (e.g., PCI, stenting)
- Electrophysiology – arrhythmia management and device implantation
- Advanced heart failure/transplant cardiology
- Non-invasive cardiology – imaging, stress testing, preventive care
Why earnings are high:
- Cardiovascular disease is a leading cause of morbidity and mortality
- High reimbursement for invasive procedures and device implantation
- Heavy demand in both urban and rural settings
Case Snapshot: Dr. Smith’s Cardiology Career Path (Expanded)
Dr. Smith completed an internal medicine residency followed by a 3-year general cardiology fellowship and an additional year in interventional cardiology. Practicing in a large metropolitan hospital system:
- She performs complex catheter-based interventions most days of the week
- Has a mix of high-acuity inpatient work and longitudinal outpatient follow-up
- Earns a salary well above the national cardiology average, with significant productivity bonuses tied to procedural volume
- Balances this with shared call schedules and cath lab emergencies, which can be intense but are offset by hospitalist and APP support
For residents, success in cardiology requires strong internal medicine performance, research, and letters of recommendation—especially for competitive interventional spots.
3. Dermatology
Approximate Average Salary: ~$500,000 (higher in procedural/cosmetic-heavy practices)
Dermatology combines medical, surgical, and cosmetic care focused on skin, hair, and nail diseases.
Why earnings are high:
- Efficient clinic-based procedures (biopsies, excisions, laser treatments)
- High patient demand for both medical and elective cosmetic services
- Flexibility to incorporate cash-pay cosmetic services (e.g., Botox, fillers, laser resurfacing)
Lifestyle profile:
- Often predictable daytime hours
- Limited overnight emergencies and hospital call in many practice models
- High patient volume with relatively short visits
For competitive dermatology spots, medical students typically need strong academic records, high board scores, and meaningful research or publications.
4. Gastroenterology
Approximate Average Salary: ~$575,000
Gastroenterologists manage digestive system disorders and perform endoscopic procedures such as colonoscopies and upper endoscopies.
Income drivers:
- High volume of reimbursable procedures
- Growing screening needs (e.g., colorectal cancer screening)
- Increasing prevalence of GI diseases in aging populations
Subspecialties with additional earning potential:
- Advanced endoscopy (ERCP, EUS)
- Hepatology and transplant hepatology
The combination of cognitive and procedural work makes gastroenterology attractive to many internal medicine residents considering both earnings and variety.
5. Anesthesiology
Approximate Average Salary: ~$450,000 (can be higher for certain subspecialties and call-heavy roles)
Anesthesiologists are essential in perioperative care, providing anesthesia, pain control, and critical care support.
Why anesthesiology remains lucrative:
- Critical role in nearly all surgical procedures
- Ability to work across multiple settings: OR, ICU, procedural suites, pain clinics
- High demand in systems with growing surgical volumes and outpatient surgery centers
Subspecialty options:
- Cardiac anesthesia
- Pediatric anesthesia
- Critical care
- Pain medicine (often with high outpatient procedure income)
Contracts can vary widely—from academic departments with moderate salaries and teaching duties to private groups staffing multiple hospitals and ASCs with high earning potential.
6. Radiology
Approximate Average Salary: ~$400,000+
Radiologists interpret imaging studies and guide minimally invasive procedures.
Why radiology pays well:
- Imaging is central to modern diagnosis in nearly every specialty
- High volumes of CT, MRI, ultrasound, and nuclear studies
- Subspecialties (e.g., interventional radiology, neuroradiology, MSK radiology) often earn more than general diagnostic radiology
Lifestyle considerations:
- Opportunities for remote/tele-radiology work
- Mix of daytime and nighttime shifts depending on practice model
- Less direct patient interaction in some roles, which some physicians consider a benefit, others a drawback
Interventional Radiology (IR) in particular blends high procedural volume with strong compensation, but requires highly competitive residency or integrated IR pathways.
7. Urology
Approximate Average Salary: ~$425,000
Urologists manage urinary tract and male reproductive system disorders, combining clinic, OR, and procedural suites.
Income factors:
- Regular schedule of elective procedures (e.g., TURPs, stone management, prostate surgery)
- Aging population with rising BPH and urologic malignancies
- Mix of surgical and longitudinal care
Subspecialties (e.g., urologic oncology, reconstructive urology, female pelvic medicine) can lead to additional income and niche reputations.
8. Emergency Medicine
Approximate Average Salary: ~$350,000 (high hourly rates, often with shift differentials)
Emergency physicians deliver acute care across all ages and conditions, often as the front door of the healthcare system.
Why EM can be financially attractive:
- Competitive hourly pay, especially nights, holidays, and high-volume EDs
- Flexible scheduling (e.g., block shifts, part-time or per‑diem opportunities)
- Locum tenens roles with premium rates
Lifestyle trade-offs:
- Irregular hours, nights, weekends, and holidays
- High burnout risk due to intensity, volume, and administrative burden
- Rewarding for those who thrive in fast-paced, acute care settings
9. Plastic Surgery
Approximate Average Salary: ~$500,000+ (especially high in cosmetic-focused practices)
Plastic surgeons perform both reconstructive and cosmetic procedures, from trauma and burn reconstruction to aesthetic surgery.
Financial drivers:
- Elective cosmetic procedures—often cash-pay—can dramatically increase earnings
- Reconstructive work after cancer, trauma, and congenital deformities is highly reimbursed and in consistent demand
- Ability to develop a niche practice (e.g., breast reconstruction, facial aesthetics, hand surgery)
Many plastic surgeons start with hospital-based reconstructive work, then gradually transition to more outpatient cosmetic practice as reputation grows.
10. Oncology (Medical Oncology and Hematology-Oncology)
Approximate Average Salary: ~$400,000
Oncologists manage cancer care, often in collaboration with surgeons and radiation oncologists.
Why oncology remains well-compensated:
- Growing cancer incidence with an aging population
- Complex, longitudinal care involving chemotherapy, immunotherapy, and targeted agents
- Integration with infusion centers, clinical trials, and multidisciplinary tumor boards
Practice types:
- Academic cancer centers (strong research focus; salary sometimes lower but with academic benefits)
- Community practices or large groups (often higher base salary and productivity bonuses)
The emotional intensity of oncology is balanced for many by strong patient relationships and the intellectual challenge of evolving therapies.
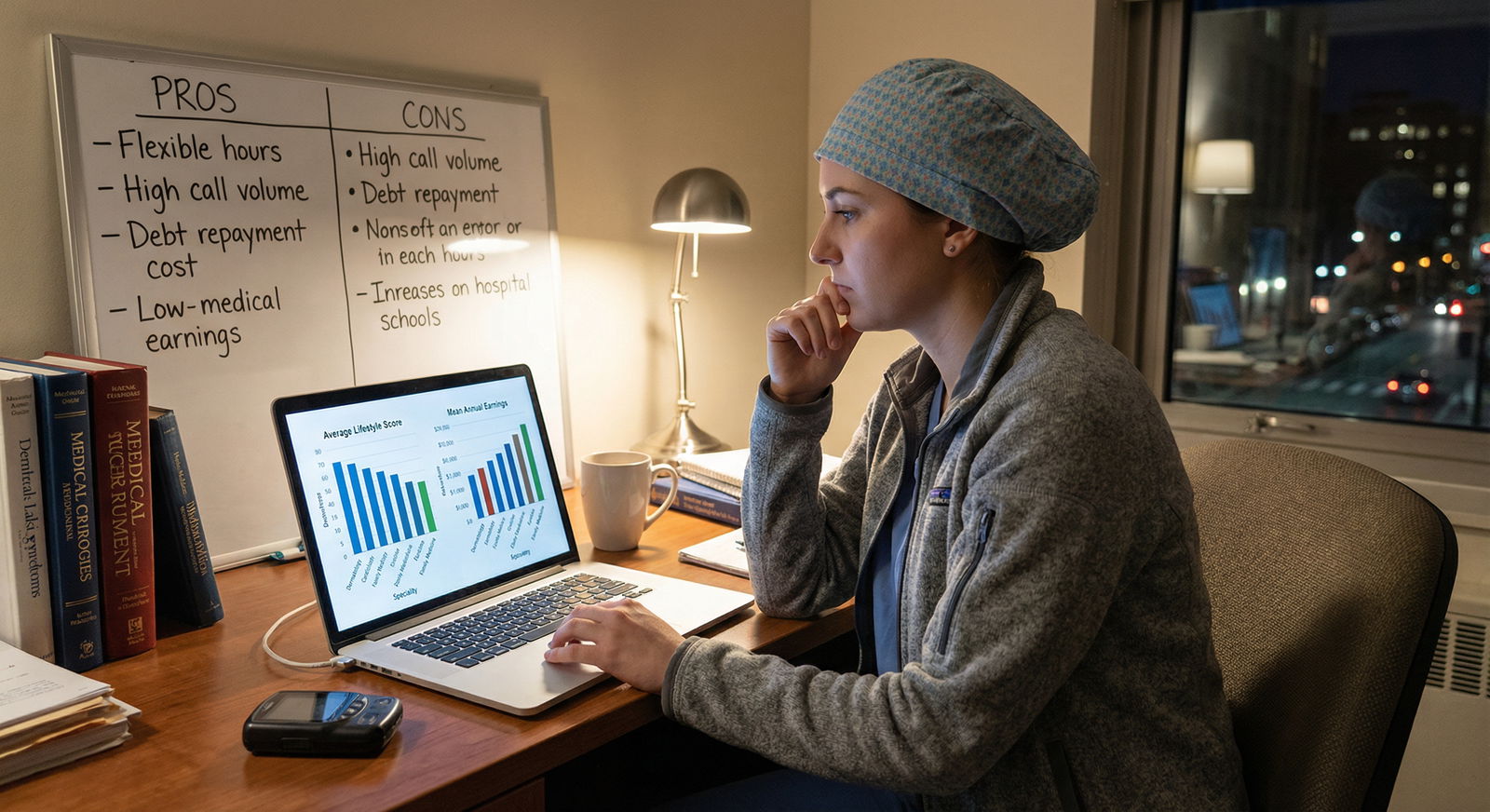
Lifestyle, Burnout, and Non-Financial Considerations
High compensation alone doesn’t guarantee a sustainable or satisfying Medical Career. When evaluating Healthcare Professions, consider:
Work-Life Balance and Burnout Risk
- More controllable lifestyles:
- Dermatology, some outpatient radiology models, certain outpatient subspecialties
- More demanding lifestyles:
- Surgical specialties with frequent call (orthopedic surgery, neurosurgery, trauma)
- Procedural subspecialties with emergencies (interventional cardiology, EM)
- Burnout risk is not purely workload-related—factors like autonomy, team culture, administrative burden, and alignment with personal values are crucial.
Physical Demands and Career Longevity
- Surgical fields and interventional specialties can be physically taxing (long time standing in OR/angio suite, lead apron use, repetitive movements).
- Some physicians transition later in career to:
- Administrative roles (medical director, department chair)
- Telemedicine or consult-heavy practices
- Less physically demanding subspecialty niches
Professional Satisfaction and Fit
Ask yourself:
- Do you enjoy procedures and working with your hands, or primarily cognitive/diagnostic work?
- Do you prefer long-term patient relationships or episodic, high-intensity care?
- How comfortable are you with uncertainty, emergencies, and high-acuity situations?
Students should seek broad exposure through rotations, shadowing, and electives before locking in a specialty based solely on income.
Strategies to Position Yourself for High-Earning Specialties
Earning potential should be one factor—never the only one—in your Specialty Selection. If you’re interested in the highest-paid specialties, you can take concrete steps during medical school and residency.
1. Be Strategic and Informed Early
- Research residency competitiveness and required board scores.
- Seek early mentorship from faculty and residents in your target fields.
- Use your clinical rotations to confirm genuine interest in the day-to-day reality of the specialty.
2. Build a Strong Academic and Clinical Profile
- Aim for solid board exam performance (USMLE/COMLEX).
- Prioritize strong clinical evaluations, especially on core clerkships related to your desired field.
- Get involved in research and quality improvement projects within the specialty; publications and presentations help for competitive matches.
3. Consider High-Value Fellowships and Subspecialization
- Within internal medicine, fields like cardiology and gastroenterology are high-paying, but require strong IM performance and competitive fellowship applications.
- Surgical residents can aim for lucrative fellowships (e.g., spine surgery for orthopedics, complex GI, vascular surgery).
- Evaluate the ROI of extra training: additional years vs. long-term earnings and fit.
4. Understand Geographic and Practice Setting Leverage
- Be open to different locations:
- Rural or midsize markets often offer higher compensation and leadership opportunities.
- High-cost urban or coastal areas may trade income for lifestyle, academic prestige, or family considerations.
- Compare:
- Academic vs. community vs. private practice
- Hospital-employed vs. independent group vs. corporate/PE-backed groups
5. Learn to Negotiate Contracts and Understand Compensation Models
- Before signing, understand:
- Base salary and duration of any guarantee period
- RVU or productivity expectations
- Call schedule and associated stipends
- Non-salary benefits: malpractice coverage (claims-made vs. occurrence), tail coverage, CME funds, retirement matching, parental leave
- Consider consulting:
- A physician-focused contract attorney
- Senior physicians in your network who have negotiated similar contracts
6. Plan for Long-Term Financial Health
High Physician Earnings do not automatically translate into long-term wealth. Build good habits early:
- Create a realistic budget and maintain an emergency fund.
- Aggressively tackle high-interest student loans, using refinancing or loan forgiveness programs when appropriate.
- Take advantage of retirement accounts (401(k), 403(b), 457(b), Roth IRA).
- Consider disability and life insurance tailored to physicians.
Frequently Asked Questions About High-Paying Medical Specialties
1. What is currently the highest paying medical specialty?
Orthopedic surgery is consistently at or near the top of the list of highest paying medical specialties, with average Physician Earnings often around or above $650,000 in the U.S., depending on region and practice type. Within orthopedics, subspecialties like spine surgery can command even higher compensation. Other top earners typically include cardiology (particularly interventional), gastroenterology, dermatology (especially cosmetic-heavy practices), and plastic surgery.
2. Should salary be the main factor in choosing a medical specialty?
Salary should be one factor, but not the primary one. Choosing a specialty solely for income can lead to dissatisfaction and burnout if the daily work does not align with your interests, personality, and values. Consider:
- Your preference for procedures vs. cognitive work
- Desire for long-term patient relationships vs. acute episodic care
- Tolerance for irregular hours, call, and emergencies A moderately lower-paying specialty that fits you well often leads to a more sustainable, enjoyable career and, over time, can still provide excellent financial stability.
3. Are higher-paying specialties always more demanding in terms of hours and call?
Not always—but many are. Surgical fields, interventional specialties, and emergency care often require:
- Early mornings and long OR days
- Frequent night and weekend call
- Unpredictable schedules However, some high-paying fields, such as dermatology or certain radiology and anesthesia practice models, offer relatively more controllable hours. The relationship between income and lifestyle depends heavily on specific practice settings, group culture, and how you structure your career.
4. How can medical students and residents prepare for a lucrative specialty?
Key steps include:
- Early exposure and mentorship in high-earning specialties to ensure genuine interest
- Strong academic performance (board scores, clerkship grades)
- Involvement in research and specialty-specific projects
- Strategic residency and fellowship choices aligned with market demand
- Willingness to consider geographic flexibility and learn basic contract negotiation skills Equally important is developing resilience, time management, and financial literacy to sustain both income and well-being over the long term.
5. Do patient demand and healthcare trends affect specialty salaries over time?
Yes. Salary trends shift with:
- Demographic changes (e.g., aging populations increasing demand for cardiology, orthopedics, oncology, GI)
- Policy changes and reimbursement updates from Medicare and private insurers
- Technological shifts (e.g., telemedicine, AI in radiology, new procedural techniques)
- Workforce supply (e.g., increased residency positions or new training programs) Staying informed about national trends and regional needs—through specialty societies, salary surveys, and mentors—helps you anticipate how compensation might evolve over your career.
Choosing a specialty is one of the most important decisions in your medical journey. Understanding the landscape of the highest paying medical specialties, along with lifestyle implications and market forces, allows you to align passion, purpose, and financial security in a thoughtful way. Use salary insights as a tool—not a dictator—as you shape a fulfilling and sustainable medical career.

















