The highest paid specialties don’t just cost you time. They change who you are outside the hospital.
Everyone loves to whisper about the salary tables and MGMA percentiles. What almost nobody tells you as a student is what those numbers actually buy—and what they quietly take away. I’ve sat in enough fellowship interviews, resident eval meetings, and off-the-record faculty dinners to tell you this plainly: you pay for the big paycheck with currency you cannot get back—your 30s, your sleep, sometimes your marriage, often your hobbies, and occasionally your sense of self.
Let’s walk through the real tradeoffs of the big-money fields—ortho, neurosurgery, IR, cardiology (especially interventional), plastics, derm (yes, even derm), and a couple of others. Not the brochure version. What actually happens to people you’ll be working with. Or becoming.
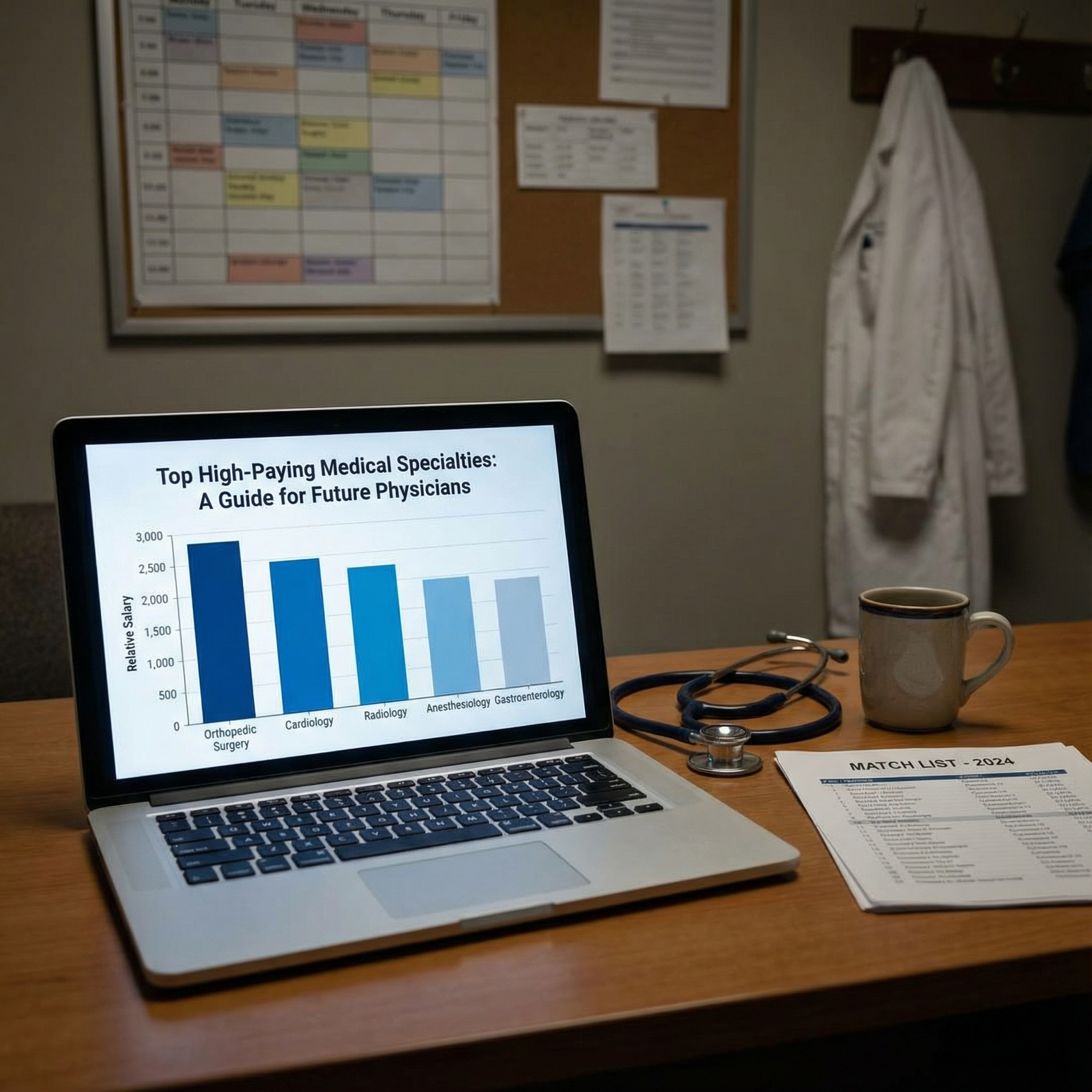
The Money vs. Life Equation: How the Top Fields Really Stack Up
Before we get into the weeds, you need a mental model.
At every program director dinner, there’s some version of this conversation: “These kids have no idea what they’re signing up for. They see the salary column and not the rest of the spreadsheet.” That “rest of the spreadsheet” is call burden, night pages, litigation risk, burnout, and whether you recognize your own kids on weekdays.
Here’s a stripped‑down comparison you will not see on official brochures.
| Specialty | Typical Call Burden | Lifestyle Control | Income Potential |
|---|---|---|---|
| Neurosurgery | Brutal | Very Low | Very High |
| Orthopedic Surgery | Heavy | Low–Medium | Very High |
| Interventional Cards | Heavy–Brutal | Low | Very High |
| Interventional Radiology | Heavy | Low–Medium | High–Very High |
| Plastic Surgery | Variable | Medium–High | High–Very High |
| Dermatology | Minimal | Very High | High |
You’re trading lifestyle control, not just hours. Two people can both work 60 hours; in one specialty that’s 7a–5p with rare weekends; in another that’s 14‑hour days plus “home call” that ruins every evening anyway.
Neurosurgery: The Poster Child of “You Don’t Own Your Life”
Neurosurgery is what happens when you give your 20s and 30s to one thing and one thing only.
Behind closed doors, neurosurgery chairs admit this openly: their best residents are those who either have no outside obligations or have a partner essentially acting as a single parent. Not because they’re bad people. Because brain bleeds don’t care that it’s your kid’s birthday.
Call is savage. Even at so‑called “cush” academic places.
A realistic flavor:
You’re post‑call, it’s 1 p.m., in theory you can go home. You have a stack of notes, a consult in the ED, and a subdural just got paged in from an OSH 45 minutes away. Your upper-level looks at you and says, “You can leave after the case.” The case starts at 3, you’re closing at 7, there’s a postop to see. Now you’re at 9 p.m.
Days like that are not outliers. They are the rhythm.

| Category | Value |
|---|---|
| Neurosurg | 80 |
| Ortho | 70 |
| Gen Surg | 65 |
| Plastics | 60 |
Lifestyle costs you won’t see in the match data:
- High divorce and delayed family formation. I’ve watched multiple neurosurgery residents quietly change their wedding dates because the chief said the original date “wasn’t great for the schedule.”
- Emotional flattening. When you watch people die routinely from catastrophic bleeds, your baseline shifts. Several neurosurgery attendings I know openly admit they don’t have close non‑doctor friends anymore. Too hard to relate.
- Chronic fatigue as a personality trait. Caffeine as a vital sign.
The upside: insane intellectual satisfaction, god‑level technical skill, enormous income at the attending level. The downside: your life is built around that role, not parallel to it.
If you’re okay with that, fine. But don’t pretend you can have neurosurgery money and dermatology lifestyle. That fantasy is how people burn out by PGY‑4.
Orthopedic Surgery: High Income, High Ego, and the Body Tax
Ortho is the classic “I want to be rich and do procedures” choice. The lifestyle story here is more complicated because it shifts dramatically over a career.
Residency: rough, but not always as apocalyptic as neurosurgery. Nights in-house, tons of consults: traumas at 2 a.m., hip fractures at all hours, mangled extremities from car wrecks. You spend years standing for long cases, retracting, reducing fractures, pushing heavy equipment around. Your own joints and back start paying rent by PGY‑3.
Private practice adult recon or sports in a good market? Now you’re talking obscene RVU potential. But here’s the catch nobody tells MS2s drooling over that $800k number:
You’re running a volume machine.
That means double‑booked ORs, clinic days with 50–70 patients, and nights buried in MyChart messages and refills because your PA can’t do all of it. You’re not doing “10 surgeries a week” because medicine loves round numbers. You’re doing however many cases it takes to keep your hospital and group happy.
Lifestyle tradeoffs:
- Your free time is chunked, never clean. There’s always one more postop you feel responsible to check, one more imaging study to review.
- Call is physically disruptive. Ortho call means going from “in bed” to “in the OR doing an ex‑fix” in under an hour. The older you get, the more that recovery lag hurts.
- You often become the “weekend dad” or “vacation dad.” I’ve seen this up close: attendings who obviously love their kids but are ghosts on weekdays.
But, unlike neurosurg, you sometimes can engineer a softer landing. Community joint replacement jobs with Q4 call, or surgery centers focused on elective sports. You will make less. You will sleep more. That’s the trade.
Interventional Cardiology: The Beeper Owns Your Nervous System
Let me be blunt: if you hate being startled awake, do not become an interventional cardiologist.
STEMI call is brutal in a very specific way. You can be at dinner, watching a movie, barely asleep—then the phone goes off and you’re in a lab guiding a wire through a coronary artery 20–40 minutes later. That’s not drama; that’s the real service level a lot of hospitals demand.
Most students see the cardiology salary ranges and think, “Okay, that’s worth it.” They don’t understand the chronic sympathetic overdrive of never really being off. I’ve heard more than one interventional attending say, “I can’t have more than one glass of wine on weekends because I’m always half-expecting a call.”
Lifestyle costs that don’t show up in any compensation survey:
- Hypervigilance. They check their phones compulsively. Even on vacations, they often feel the need to “just peek” at messages and echo results.
- Sleep fragmentation. The older they get, the harder it is to go back to bed and get real rest after a 3 a.m. STEMI.
- Personality drift. The constant “hurry up, this is life‑or‑death” pressure bleeds into how some of them relate to family. They get short, impatient, always on fast‑forward.
A lot of interventionalists try to back off after 10–15 years. They pivot to structural, imaging heavy, admin roles, or scale down their STEMI call. The unspoken reality: not every group lets you do that without a significant income hit or internal resentment.
If you’re thinking of this path, ask attendings in their 50s: “What does your call look like now compared to 10–15 years ago?” Watch their face.
Interventional Radiology: High Tech, High Pay, Hidden Lifestyle Traps
IR sells a seductive story: procedural, cutting‑edge, lots of toys, competitive salary, and—supposedly—better lifestyle than surgeons. The truth is more nuanced.
Yes, some IR groups have more controllable calls than trauma surgery. But image‑guided emergency work is not exactly 9–5. There will be nights where you’re up embolizing bleeds, dealing with septic patients and drain placements, or getting called in for massive GI bleeds when GI has tapped out.

| Category | Value |
|---|---|
| Neurosurgery | 7 |
| Interventional Cards | 6 |
| Interventional Radiology | 4 |
| Ortho | 3 |
The lifestyle tax people underestimate:
- “Home call” that isn’t really home. You’re technically not in-house, but your brain is tethered. You can’t be far, you can’t fully relax, and you learn to sleep with one ear open.
- Constant negotiation with diagnostic colleagues. Many IRs end up doing more diagnostic reads than they expected just to keep the group functional. Those extra hours don’t feel as fulfilling but they eat evening time.
- Burnout from being everyone’s last resort. When medicine, surgery, or GI has no good option, they punt to IR. That can be intellectually satisfying. It can also be emotionally exhausting when you’re getting called into messy, late, high‑risk cases with poor baseline prognosis.
The good news: there actually are IR jobs with decent boundaries—often in larger groups with separate night coverage or hospital-employed models with protected time. The bad news: those are heavily sought after, and you won’t get one just by existing. You’ll need a reputation.
Plastic Surgery: The Mirage of “Pretty Surgery, Pretty Life”
Plastics is complicated because it’s actually multiple lifestyles hiding under one name.
Academic microsurgery (free flaps, trauma recon) is very different from high‑end cosmetic cash‑pay practice. The former looks more like other big surgeries: long cases, emergent consults, late nights after sarcoma resections. The latter is what most med students fantasize about: clinic-based, elective, high‑margin procedures on private‑pay patients.
Here’s what people who live in the cosmetic world don’t post on Instagram:
- Your patients are demanding in a very different way. They’re not dying, but they are intensely invested, often with unrealistic expectations. A small asymmetry can create weeks of emails, angry calls, or threats.
- Your income is directly tied to your brand and grind. Building that takes years. Many young plastic surgeons work insane hours early on—multiple OR days, stacked clinics, endless marketing, social media, traveling to conferences to get their name out.
- The pressure to never screw up is enormous. Everyone in private plastic surgery has at least one story of a botched outcome that ended in litigation or a reputational hit that took years to scrub away.
Is there a version of plastics where you make strong money and have decent hours? Yes—regional reconstructive practices, breast recon tied to cancer centers, balanced academic jobs. But they often come with call, complex patients, and all the emotional load of oncology or trauma.
So you’re not escaping intensity. You’re just choosing your flavor: operative stress, aesthetic pressure, or a blend.
Dermatology: The “Easy” Field That Quietly Consumes Your Time Anyway
Let me shatter a myth: dermatology is not “easy.” It’s controllable. That’s different.
Derm lifestyle wins in almost every direct comparison. No overnight emergencies for most, minimal call, clinic hours that can snugly fit into a 4‑day week if you structure it right. Procedural derm (Mohs, cosmetics, lasers) can print money without hospital drama.
But here’s the part most students miss: high‑earning derm practices often maximize throughput to a degree that would make a hospital CMO blush.
You think you’ll be leisurely looking at rashes. In reality, high‑volume derm clinics run like this:
- 35–45 patients a day. Sometimes more.
- 10–15 minute slots, often double‑booked.
- Cosmetic half‑days jammed with back‑to‑back procedures.
You walk out physically less exhausted than after a 12‑hour surgery day, yes. But you can be mentally fried in a very specific way—death by 1000 follow‑ups, biopsies, and benign but anxious patients.
Tradeoffs dermatologists talk about privately:
- The monotony tax. Rashes, acne, benign nevi, repeat. The rare zebras do not show up every day.
- The subtle moral tension of cosmetics. You can make more money injecting filler than managing complex immunobullous disease. Some people lean in. Some feel gross and conflicted.
- The golden handcuffs. It’s very hard to walk away from a 4‑day, $600k life, even if part of you is bored.
Is derm the “best” lifestyle per dollar? Probably. But if you’re going to chase it, be honest: you’re choosing a high‑throughput, outpatient machine in exchange for near‑total schedule control.
The Real Hidden Cost: Your Identity Outside Medicine
Here’s the thing most premeds and early med students don’t even realize they’re wagering: who you will be when you’re not wearing a badge.
The higher‑pay, higher‑intensity specialties blur that boundary hard. You don’t just work long hours. Your brain is colonized.
A few patterns I’ve watched play out over and over:
- Personal relationships reduced to logistics. When call is that heavy, scheduling becomes the main mode of relating. “I can do dinner Thursday if I’m not on call.” “We can go away that weekend, but I might have to come back early.”
- Hobbies turning into vague nostalgia. The neurosurgery attending who used to play in a band. The interventional cardiologist who “used to run marathons.” Ask them when they last did those things seriously.
- Geographic handcuffing. High-paying subspecialties are market‑sensitive. You might have to live where the jobs are. Spouse’s career? Kids’ school district? Those become secondary to where a hospital will pay you for your procedural volume.

None of this means you should avoid high‑pay specialties. It means you need to stop pretending it’s just about loving the field or being “okay working hard.” Everyone applying to these specialties “works hard.” The differentiator is what you’re willing to bleed into the job: nights, weekends, relationships, identity.
How to Decide If the Tradeoffs Are Worth It (For You)
Here’s the behind‑the‑scenes filter faculty actually use when they talk about students going into these fields.
They ask:
- Does this person actually enjoy the work when it’s miserable? Not just the highlight reel, but the 3 a.m. consults and nightmare patients.
- Do they have a support system that can survive the training grind?
- Are they idealizing the lifestyle based on salary data more than real exposure?
And the ugly one: “Do they look like they’ll burn out and quit?”
You should be asking the same questions of yourself, ruthlessly.
| Specialty | Biggest Lifestyle Hit | Main Lifestyle Upside |
|---|---|---|
| Neurosurg | Time, sleep, autonomy | Extreme intellectual reward |
| Ortho | Physical strain, long days | Predictable elective work |
| Interv Cards | Sleep, constant vigilance | High acuity, high reward |
| IR | Tethered call, last-resort cases | Technical variety |
| Plastics | Patient expectations, brand grind | Elective cases, income |
| Derm | High volume, monotony | Control, minimal call |
You do not need a perfect answer as an MS3. But you do need to stop asking, “Which specialty is best?” and start asking, “Which set of problems am I willing to own for decades?”
Spend a full 24‑hour call with the residents in the specialty you’re eyeing. Watch them at 2 a.m. and at 4 p.m. the next day. That’s the life you’re choosing. Not the conference talk. Not the Instagram post from the OR.
FAQs
1. If I choose a high-paying specialty, can I just “fix” the lifestyle later by going part-time or concierge?
Sometimes, but it’s not a guarantee. In many procedural fields, your group or hospital expects a certain level of volume to justify your spot. Dropping call or cutting your schedule can mean significant income loss, political fallout, or being quietly pushed out. Concierge and boutique models exist, but they’re rare, competitive, and require brand, capital, and a specific patient base. You cannot bank on that escape hatch.
2. Are academic jobs in these specialties always better for lifestyle?
No. That’s a myth students cling to. In some places, academic neurosurgeons, ortho trauma, or IR attendings work more than private counterparts because they do tough cases, run services, teach, and do admin on top. The lifestyle equation varies by institution, division, call structure, and how many people share the burden. “Academic” is not a synonym for humane.
3. How much should I let money influence my specialty choice?
More than idealists claim, less than cynics think. You will feel financial stress at some point—debt, cost of living, family responsibilities. Having a strong income helps. But if you hate the day-to-day work, no salary will fix that. I’ve watched people in high‑pay fields quietly fantasize about switching to EM or psych because they’re miserable. Use income as a tiebreaker between fields you genuinely like, not the primary driver.
4. What’s the best way to get honest lifestyle information from residents and attendings?
Ask specific, non‑flattering questions when you’re off the record. “How many nights last month did you get more than 6 hours of uninterrupted sleep?” “When was the last time you canceled personal plans because of work?” “If your kid has a school performance at 3 p.m. on a weekday, can you go?” Vague questions get brochure answers. Concrete questions force people to tell you how their life actually runs.
Key takeaways: High‑paid specialties don’t just cost hours; they restructure your relationships, your sleep, and your identity. Salary tables hide the realities of call, control, and chronic stress. Choose your field based on which problems you’re willing to wake up with for 20–30 years, not just which number looks best in an MGMA column.

















