The worst mistakes unmatched grads make happen in the first 12 weeks. Not on Match Day.
You either drift. Or you run a disciplined, brutal, week-by-week recovery plan.
This is the second path.
Below is a 3‑month, week‑by‑week playbook for what to do after you fail to match. Not vibes. Not “stay positive.” Concrete tasks. Deadlines. Conversations.
Assumptions:
- You just went unmatched (or partially matched) in the NRMP Main Match.
- You want to maximize your chances for:
- SOAP (if still in progress),
- the Supplemental Offer rounds,
- off-cycle spots,
- or a stronger reapplication next cycle.
If your timeline’s slightly different (late SOAP, military, Canadian match), the structure still holds. Shift weeks as needed.
Big Picture: Your 12‑Week Recovery Map
At this point you should stop thinking in months. Think in weeks. Your opportunities decay fast.

| Period | Event |
|---|---|
| Shock to Strategy - Week 1 | Process emotions, collect data, meet advisor |
| Shock to Strategy - Week 2 | Deep application autopsy, choose target paths |
| Rebuild and Reposition - Week 3 | Fix paperwork, start outreach, line up work |
| Rebuild and Reposition - Week 4-6 | Systematic networking, research/clinical role, exam planning |
| Execute New Trajectory - Week 7-9 | Produce output, letters, applications, interviews |
| Execute New Trajectory - Week 10-12 | Lock next 6-12 months, prepare for reapply |
You’re going to move through three phases:
- Weeks 1–2: Stabilize and Analyze – Stop the emotional free-fall and understand exactly why you didn’t match.
- Weeks 3–6: Rebuild and Reposition – Fix your deficits and get yourself visibly productive.
- Weeks 7–12: Execute and Lock in Next Steps – Secure a meaningful role and prep a stronger application.
Let’s go week by week.
Weeks 1–2: From Shock to Strategy
Week 1: Match Week / SOAP / Immediate Triage
At this point you should contain the damage and keep optionality open.
Day 1–2 (Match Day + next day):
Let yourself react. But give it a time box.
- 24–48 hours max. After that, emotions still exist, but they don’t run the schedule.
- Tell 2–3 key people: one trusted friend/family member, one mentor/faculty, one class dean.
Clarify your match status:
- Fully unmatched vs. partially matched vs. only unmatched in prelim/advanced.
- Identify if SOAP is still ongoing or already past.
-
- Meet with Student Affairs immediately (same day if possible).
- Prioritize:
- Updating your ERAS application (personal statement, experiences).
- Adjusting your program list to realistic options (often community, prelim, categorical IM/FM/psych, etc.).
- Preparing short, direct email templates to programs:
- 2–3 sentences, stating interest, quick CV highlight, attached ERAS application.
If SOAP is done and you still have no position:
- Ask your dean whether there were:
- Any late-opening positions.
- Contacts at nearby programs who might take a transitional/Research/NP role.
- Get clarity on your official status with your medical school (graduation timing, availability for extra rotations, etc.).
- Ask your dean whether there were:
By end of Week 1 you should have:
- A confirmed status (unmatched, partial, SOAP result).
- A scheduled meeting with at least one honest advisor (not just the “it’ll all be fine” type).
- A rough sense of your main weaknesses:
- USMLE/COMLEX score issues?
- Late/weak application?
- Limited interviews?
- Visa or IMG status?
- Specialty too competitive (e.g., derm, ortho, plastics) with no realistic backup?
Week 2: Full Application Autopsy and Path Decision
This is where most people screw up. They skip the autopsy and jump straight to “I’ll just reapply.” That’s how you become a two‑time unmatched story.
At this point you should get brutally clear about why you failed to match and what’s realistically fixable in 12 months.
- Do a structured application review:
Sit down with:
- Faculty advisor in your target specialty (or ex-target if switching).
- Dean or Director of Student Affairs.
- Someone who’s on a residency selection committee if you can get them (they’re blunt; that’s what you need).
Bring:
- Your full ERAS application.
- Score reports.
- Interview list and outcomes.
- Rank list.
Ask them to grade you in each domain on a 1–10 scale:
| Domain | Your Score (1–10) |
|---|---|
| USMLE/COMLEX scores | |
| Clinical grades | |
| Letters of rec | |
| Research/scholarship | |
| Clinical experiences | |
| Professionalism | |
| Personal statement |
Force them to mark:
- Primary red flags (e.g., Step failure, professionalism write‑up).
- Secondary weaknesses (e.g., weak letters, generic personal statement).
- Competitive mismatch (e.g., aiming for derm with 225 and no research).
- Decide your realistic target path(s):
You’re not choosing forever. You’re choosing the next cycle or the next 1–2 years.
Typical shifts:
- Competitive to less competitive (e.g., surgery → IM; radiology → prelim + reapply; derm → IM/FM/psych).
- Same specialty but much stronger application (better scores, research, more letters, strong home program support).
- One-year “bridge role” (research, prelim, non‑ACGME fellowship, or home‑institution role) before reapplying.
- Sketch your 12‑month strategy on one page:
- Target specialty (Primary and true backup).
- Core deficits to fix.
- Concrete plan:
- Scores: Step 3? COMLEX Level 3? Improved OET/IELTS?
- CV: Research project? Extra sub‑I? Teaching role?
- Relationships: New letters? More face time at programs?
By end of Week 2 you should have:
- A written, honest assessment of why you went unmatched.
- A documented 12‑month target path.
- Agreement from at least one faculty mentor that your plan is not delusional.
Weeks 3–6: Rebuild and Reposition
Now you shift from analysis to action. No one cares about your introspection unless it turns into tangible output.
Week 3: Get Visible and Fix the Paperwork
At this point you should start closing obvious structural gaps and get yourself on people’s radar.
Paperwork and logistics:
- Confirm:
- Graduation date.
- Diploma/degree availability.
- School email access duration.
- If you’re an IMG:
- Check ECFMG status.
- Confirm what’s required for Step 3 eligibility and visa constraints.
- Confirm:
Start Step 3 / Level 3 planning (if relevant):
- If your biggest issue was marginal Step 1/2 scores, you need a strong Step 3 as a signal.
- End of Week 3:
- Choose exam window.
- Buy Qbank.
- Sketch a 12–16 week study plan that fits around any job/research.
Immediate outreach to key faculty:
- Goal: You don’t vanish. People remember you’re serious.
- Email 3–5 faculty (especially PDs/APDs you know):
- Thank them for prior support.
- Briefly share you went unmatched and your target plan.
- Ask: “Would you be open to my helping with clinical projects, QI, or research in the department over the coming months?”
Start hunting for a “bridge role”:
- Broad categories:
- Research assistant / research fellow in your specialty or adjacent.
- Clinical observer / junior faculty extender at your home institution.
- Prelim PGY‑1 spots opening late (yes, they pop up).
- Places to look:
- Institutional job boards.
- Cold outreach to program coordinators.
- Specialty listservs and Twitter/X.
- Broad categories:
By end of Week 3 you should have:
- A Step 3/Level 3 plan (if applicable).
- 3–5 meaningful emails sent to potential sponsors.
- At least 3 active “bridge role” prospects.
Week 4: Tighten the Story and Start Systematic Outreach
At this point you should get your narrative under control and scale your networking.
- Draft your “unmatched story” – the 30‑second and 2‑minute versions:
- 30‑second:
- “I applied to X this year, received Y interviews, and unfortunately did not match. After reviewing with my mentors, we identified [key issues]. I’m now doing [concrete plan], and I’m committed to building a much stronger application for [specialty/next cycle].”
- 2‑minute:
- Slightly more detail on what went wrong and what you’re actively doing.
- 30‑second:
Practice this. Out loud. With a friend. You’ll use it constantly.
Update all your application materials:
- Clean up your CV to reflect:
- “Post‑Match 202X – present: Candidate for [bridge role]/Research volunteer” if already started.
- Rewrite your personal statement structure:
- Less fluff about childhood dreams.
- More concrete experience, reflection, and how you’re addressing prior weaknesses.
- Clean up your CV to reflect:
Systematic networking (start the spreadsheet):
- Make a simple tracker with columns:
- Program, Contact, Role (PD/APD/Coordinator/Faculty), Date Contacted, Response, Follow‑up Date.
- This week:
- Reach out to 10–20 programs where:
- You previously interviewed,
- You have school alumni,
- Or you have any thin connection (rotations, conferences, etc.).
- Reach out to 10–20 programs where:
- Make a simple tracker with columns:
Subject line examples:
- “Unmatched applicant from [School] – seeking research or observer role”
- “[Your Name], MD – Interested in off‑cycle PGY‑1 or research position”
By end of Week 4 you should have:
- A polished narrative you can say without freezing.
- Updated CV and draft personal statement.
- 10–20 programs contacted, logged, and scheduled for follow‑up.
Weeks 5–6: Build Real Work and Momentum
Now we move from “looking busy” to “actually doing things programs respect.”
At this point you should be attached to something real (research, clinical, or academic) and advancing your exam prep.
Week 5: Secure and Start a Concrete Role
Lock in something structured:
- Best-case:
- Paid research fellow/assistant in your target specialty at an academic center.
- Off-cycle prelim/transitional position.
- Very acceptable:
- Unpaid research with strong faculty who publish.
- Clinical observer with consistent schedule and opportunities for letters.
- Minimum:
- Teaching role (anatomy TA, OSCE preceptor) plus research on the side.
- Best-case:
Clarify expectations early:
- Ask your supervisor in week one:
- What projects can I realistically complete in 6–9 months?
- What would I need to do for you to feel comfortable writing a strong letter?
- How often can we check in on progress?
- Ask your supervisor in week one:
Step 3/Level 3:
- Start consistent daily questions (even 20–40 per day).
- Do not postpone this indefinitely. Programs smell procrastination.
Week 6: Produce Tangible Outputs and Scale Relationships
At this point you should convert “role” into “outcomes in progress.”
Push for early, visible progress:
- Aim for:
- A literature review draft,
- Data collection started,
- An abstract/submission plan (even if for a small regional meeting).
- Aim for:
Build depth with 2–3 key mentors, not 20 superficial contacts:
- Schedule:
- A 20‑minute check‑in with your main research/clinical mentor to review your reapplication strategy.
- Explicitly say:
- “My goal is to be a much stronger applicant for [cycle year]. I’d appreciate honest feedback on what you think I must accomplish between now and then.”
- Schedule:
Keep job options open:
- Continue monitoring:
- NRMP “Find a Resident,”
- Specialty society job boards,
- Program Twitter/X for sudden PGY‑1 or PGY‑2 spots due to attrition.
- Continue monitoring:
By end of Week 6 you should have:
- A defined role with regular weekly work.
- Active projects (not just “we’re talking about maybe starting something”).
- Step 3/Level 3 prep underway with actual Qbank progress.
Weeks 7–12: Execute, Produce, and Lock in Next Year
This is the phase where people plateau. They settle into the new routine and forget they’re on the clock for the next Match.
You don’t get that luxury.

| Category | Value |
|---|---|
| Research/Clinical Work | 45 |
| Exam Prep | 25 |
| Application Prep & Networking | 20 |
| Rest/Personal | 10 |
Weeks 7–8: Convert Work to Future Application Strength
At this point you should turn your daily grind into concrete bullets on your next ERAS.
Push for early academic output:
- Target:
- 1–2 case reports or brief communications,
- 1 poster abstract,
- Or clear role in a bigger project (data analysis, methods, etc.).
- Don’t worship high‑impact journals. You need anything solid and finished.
- Target:
Clarify letters of recommendation:
- Identify 2–3 future letter writers by Week 8:
- Your current research/clinical supervisor.
- A faculty member who has seen you teach/lead.
- Possibly a PD/APD if you’re embedded in their department.
- Identify 2–3 future letter writers by Week 8:
Phrase it like:
- “If I continue at this pace and contribute meaningfully through the year, would you feel comfortable writing a strong letter of recommendation for my next application?”
Step 3/Level 3 mid-course review:
- Compare:
- Qbank performance vs. your original base.
- If you’re consistently hitting safe ranges:
- Book the exam date if you haven’t already.
- If not:
- Adjust study schedule (may mean fewer social commitments, not fewer questions).
- Compare:
Application planning (quietly):
- Start drafting:
- A list of programs to target,
- A realistic specialty + backup strategy,
- Notes on how your new experiences change your personal statement.
- Start drafting:
By end of Week 8 you should have:
- At least 1 concrete scholarly product in motion (submitted, drafted, or assigned clearly).
- 2–3 mentors who have implicitly or explicitly agreed to back you.
- Firm exam timeline.
Weeks 9–10: Solidify Your Next 6–12 Months
Now you zoom out again.
At this point you should have a clear, defensible story for what you’re doing between now and the next ERAS opening.
Lock in your current role’s duration:
- Get written confirmation:
- Start and end dates,
- Expectations,
- Whether you can continue part‑time if you match.
- Helps for ERAS entries and makes you look like you’re not just drifting.
- Get written confirmation:
Rehearse your “future applicant” interview answers:
- You will get asked:
- “Why do you think you didn’t match the first time?”
- “What have you done in the interim?”
- “Why this specialty and not your original choice (if you switched)?”
- You will get asked:
By Week 10, your answers should:
- Be calm, factual, and not bitter.
- Emphasize growth, not victimhood.
- Point to specific achievements, not vague “reflection.”
- Program‑level targeting (get granular):
- For your top 15–20 realistic programs, know:
- Their usual Step cutoffs.
- How many IMGs/DOs they take (if relevant).
- Whether they value research vs. service vs. local ties.
- Start quietly aligning:
- Projects that involve those faculty,
- Presentations at conferences they attend.
- For your top 15–20 realistic programs, know:
Weeks 11–12: Finalize Infrastructure and Mental Fortitude
Last phase of this 3‑month window. You’re not “done,” but your trajectory should be locked in.
At this point you should have a machine running: consistent work, exam plan, mentor network, and reapplication structure.
- Audit your progress against your Week‑2 autopsy:
- Take the same domain list and re‑score:
- Scores (if you took an exam).
- Research.
- Clinical exposure.
- Letters.
- Professionalism.
- Take the same domain list and re‑score:
Ask yourself and a mentor:
- “If I were a PD seeing my file now vs. six months ago, would I see real change or cosmetic tweaks?”
Fix any obvious residual gaps:
- Examples:
- No US clinical experience → negotiate additional observership or sub‑I.
- No US letters in target specialty → request closer involvement with one faculty to earn a letter.
- Weak communication skills → ask to give short talks, teach students, present at journal clubs.
- Examples:
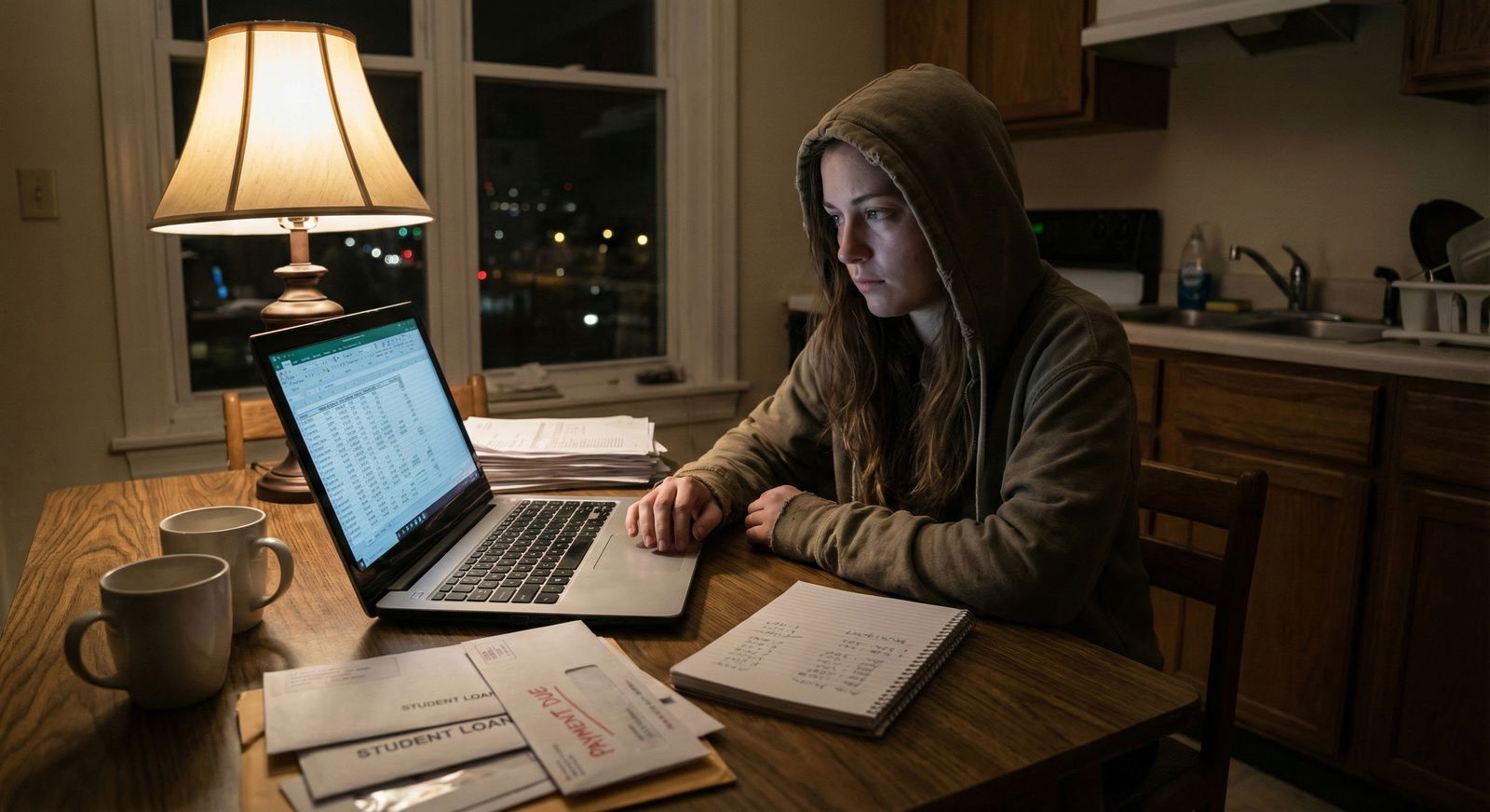
Mental and financial planning:
- Brutal truth: this is a marathon of uncertainty.
- By Week 12 you need:
- A simple budget for the next 6–12 months (rent, food, exam fees, ERAS fees, interview costs).
- A minimum set of non‑negotiable habits:
- Sleep window,
- Exercise 2–3x/week,
- Weekly social check‑in with at least one human who isn’t a doctor.
Set your next checkpoint: 3 months from now
- Mark a date to:
- Reassess progress,
- Adjust specialty/program list,
- Decide whether a second reapplication is rational if you’re considering that path.
- Mark a date to:
What This 12‑Week Plan Really Does for You
Three core things:
It stops the spiral. You’re not waking up months later with nothing to show but anxiety and “I should haves.” Every week has a job.
It turns “unmatched” into “in progress.” Programs don’t care that you were perfect. They care that when something went wrong, you built a structured, disciplined response and produced results.
It gives you a story that makes sense. When a PD asks, “What happened?” you won’t ramble. You’ll walk them through year-by-year, month‑by‑month, with receipts.
Stick to this for 12 weeks and you’re no longer “the person who didn’t match.” You’re “the person who got hit hard and then treated it like a serious professional problem, not a personal collapse.” And that’s the kind of person people are willing to take a chance on.






















