Crafting the Perfect Residency Rank List: Practical, Strategic Steps for the Match
Navigating residency applications and the Match Process is one of the most intense phases of medical education. Beyond personal statements, interviews, and letters of recommendation, one decision holds disproportionate weight: how you build your Residency Rank List (RRL).
Your RRL is more than a list; it’s a strategic roadmap that influences where you will train, who will mentor you, and what doors may open for your long-term career development. A thoughtful, well-structured Rank List Strategy can mean the difference between simply matching and matching into a program where you truly thrive.
This guide walks you through a step-by-step approach to crafting a residency rank list that reflects both your professional goals and personal values—grounded in how the Match algorithm actually works and what current residents wish they had known.
Understanding the Residency Rank List and the Match Algorithm
Before building your strategy, it’s crucial to understand what your Residency Rank List is—and what it is not.
What the Residency Rank List Really Does
Your RRL is the official, ordered list of programs you would be willing to train at, submitted via NRMP (for U.S. allopathic residencies) or a similar matching service. The algorithm then compares:
- Your list of programs (in order of your true preference)
- Each program’s rank list of applicants
The algorithm is applicant-proposing, meaning it tries to match you to the highest-ranked program on your list that also ranks you highly enough to have a spot. This is critically important:
You should always rank programs in the true order of your preference, not based on where you “think” you’ll match.
Trying to “game” the system—putting “safer” programs higher or downgrading “reach” programs—almost always works against you.
What the Rank List Is Not
- It is not a prediction tool for where you will match.
- It is not a signal to programs of your interest (that ship sailed with ERAS and interviews).
- It is not set in stone until the final submission deadline—you can and should revise thoughtfully until you’re confident.
Understanding this foundation allows you to focus on what matters: where you actually want to train and what kind of physician you want to become.
Step 1: Clarify Your Priorities and Non-Negotiables
Creating a strong Rank List Strategy starts with introspection. Before you evaluate programs, you need to know what you’re optimizing for.
Identify Your Core Professional Goals
Reflect honestly on where you are in your medical education and where you hope to be:
Ask yourself:
- What specialty am I most committed to—and why?
- Am I interested in an academic career, community practice, or a mix?
- Do I see myself pursuing fellowship? If so, which ones?
- How important are research, teaching, or leadership opportunities?
If you are undecided between fellowship or practice style, lean toward programs that keep doors open—those with strong mentorship, broad exposure, and proven resident outcomes.
Define Lifestyle and Personal Priorities
Residency is demanding, but the environment can either support or strain your well-being. Consider:
- Location
- Proximity to partner/family
- Cost of living and housing
- Urban vs. suburban vs. rural
- Climate and your tolerance for it
- Work–Life Integration
- Call schedules and night float structure
- Wellness resources (counseling, protected time, fitness)
- Flexibility for significant life events (weddings, children, family illness)
Create a Ranking Criteria Framework
Turning vague preferences into a structured framework will make your Rank List decisions clearer and less emotional. Common criteria include:
Training Quality and Reputation
- Board pass rates
- Case complexity and volume
- Fellowship match outcomes
- Program accreditation status and any recent citations
Faculty, Culture, and Mentorship
- Faculty accessibility and teaching style
- Presence of formal mentorship or coaching programs
- Resident camaraderie and psychological safety
- Diversity, equity, and inclusion efforts (and how genuine they feel)
Program Structure and Curriculum
- Balance of inpatient vs. outpatient exposure
- Subspecialty rotations and elective time
- Simulation training, didactics, quality improvement exposure
- Flexibility in scheduling (e.g., research blocks, global health electives)
Compensation and Benefits
- Salary relative to local cost of living
- Health, dental, and disability insurance
- Meal stipends, parking, educational funds, conference support
- Parental leave policies and vacation time
Action Step:
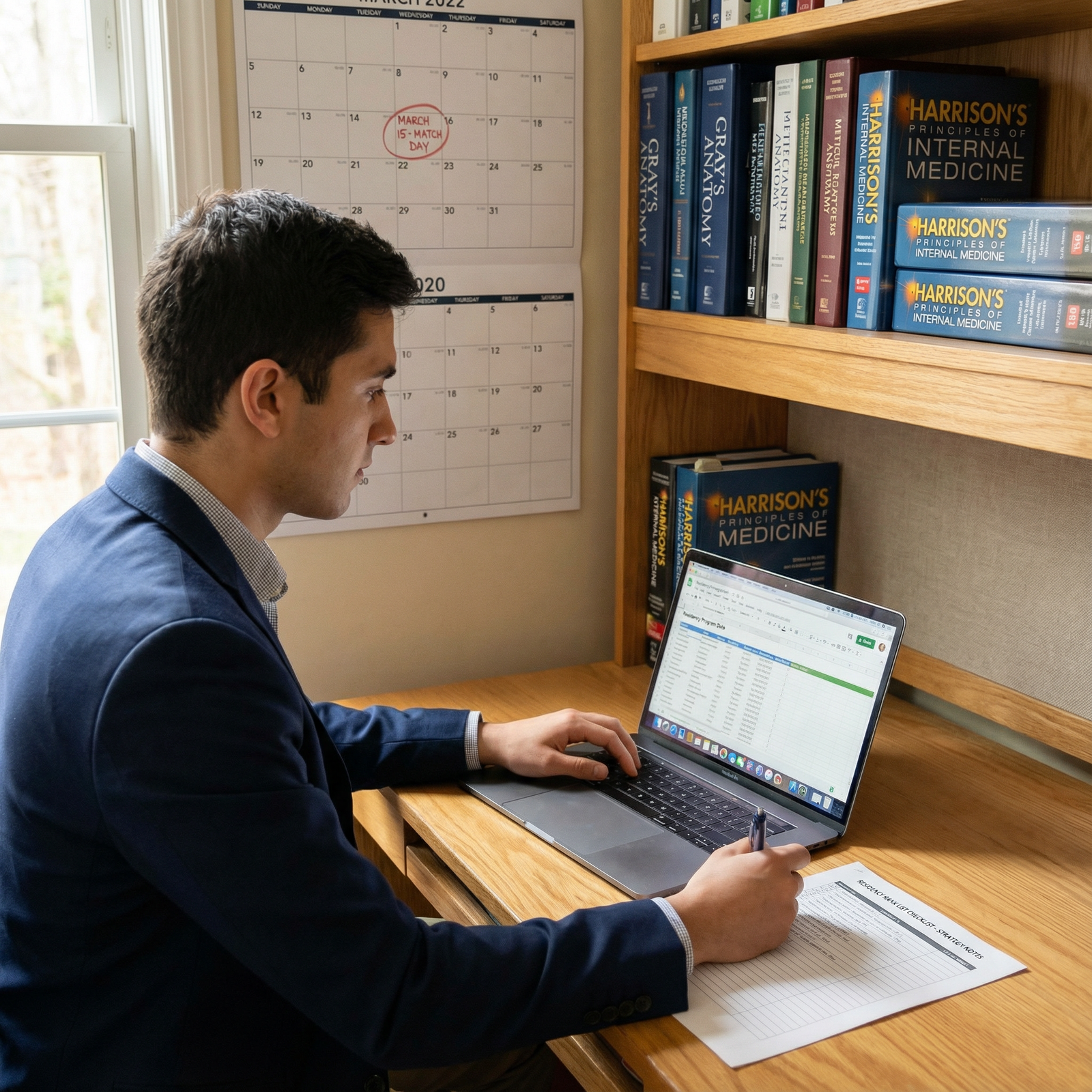
Create a spreadsheet with columns for each criterion and rows for each program. Assign importance weights (for example, 1–5) to each criterion based on how much it matters to you. This will later help structure your Rank List Strategy more objectively.

Step 2: Researching and Evaluating Residency Programs Thoroughly
Once you know what you want, systematically gather information about each program on your list.
Use Multiple Information Sources
Rely on more than one channel when evaluating programs:
Official Program Websites
- Curriculum details and rotation schedules
- Faculty profiles and leadership bios
- Resident roster and alumni destinations
- Call schedules, didactic structure, and wellness initiatives
Online Databases and Tools
- FREIDA (AMA): Program size, benefits, contact info, fellowships, and more
- Specialty-specific resources (e.g., ACGME data, professional society websites)
- State medical boards or accreditation updates
Word of Mouth and Informal Channels
- Current residents and alumni from your medical school
- Faculty advisors who know certain programs well
- Peer networks and student organizations
Social Media and Virtual Presence
- Program Instagram/Twitter/X: resident life, community outreach, culture signals
- Resident-led Q&A sessions or webinars
- Virtual open houses and information sessions
Critical Questions to Ask About Each Program
As you research, focus on questions that matter to your career development and well-being:
Clinical Training
- Do residents graduate feeling confident and well-prepared?
- Are there enough procedures, complex cases, and autonomy?
- Is there a good mix of patient populations and pathologies?
Culture and Support
- Are residents comfortable raising concerns?
- How does the program respond to burnout, mistreatment, or crises?
- Do residents have a voice in program changes?
Career Outcomes
- Where do graduates practice or match for fellowship?
- Does the program support research or scholarly projects if desired?
- Are there career development workshops, CV review, mock interviews?
Action Step:
As you research, immediately log key pros/cons and objective notes in your spreadsheet. Don’t rely on memory—by the time you’re ranking, interviews will blur together.
Step 3: Using Interview Experiences to Refine Your Impressions
Your interview season is not just about programs evaluating you—it’s your chance to evaluate them. This is one of the most important inputs into your Rank List Strategy.
Maximize What You Learn on Interview Day
During interviews (virtual or in-person), pay attention to both spoken content and the “hidden curriculum”:
From Faculty and Program Leadership
- Are they transparent about challenges (e.g., recent changes, duty hour issues)?
- How do they talk about their residents—proudly, respectfully, or dismissively?
- Do they ask about your goals and show genuine interest?
From Residents
- Do they seem satisfied and supported?
- Can they speak honestly, or do they appear guarded?
- How do they describe:
- Workload and call
- Camaraderie and social life
- Mentorship and feedback
Environment and Logistics (especially for in-person visits)
- Clean, organized workspaces?
- Availability of resident workrooms and call rooms?
- Hospital systems and EMR usability?
Post-Interview Reflection: Capture Impressions Immediately
Right after each interview, take 10–15 minutes to jot down:
- Gut reaction (1–10): How excited would you be to match here?
- Major pros: At least 3 distinct positives
- Major cons or concerns: At least 2 honest drawbacks
- Lifestyle fit: Can you see yourself living in this city for 3–7 years?
- Red flags: Any hints of toxicity, poor support, or resident burnout?
These immediate reflections are often more accurate than what you remember weeks later.
Step 4: Building and Refining Your Initial Rank List
With research and interview impressions in hand, you’re ready to create a structured draft of your Residency Rank List.
Start with Your True Preferences
Using your spreadsheet and interview notes:
- Make an initial, intuitive ranking based on where you’d be happiest and best-trained.
- Then compare that with your weighted criteria scores to see if any major mismatch jumps out.
Sometimes your top “feel” programs and top “score” programs will align. If they don’t, examine why:
- Did prestige overshadow culture?
- Did location bias your judgment too strongly?
- Are you undervaluing a program that fits your career goals better?
Distinguish Between “Good,” “Acceptable,” and “No-Go” Programs
Label each program as:
- Category A: Ideal Fit – You’d be thrilled to match here.
- Category B: Solid Options – You’d be satisfied and well-trained.
- Category C: Acceptable – You’d be okay but not enthusiastic.
- Category D: Do Not Rank – You would genuinely rather go unmatched than train here.
A key principle:
Do not rank any program where you would be miserable or unsafe, or that would severely compromise your well-being or integrity.
If a program is a “red flag” for serious toxicity, harassment, safety issues, or personal incompatibility, leave it off your RRL altogether.
Seek Input—but Stay in the Driver’s Seat
Share your draft list with:
- A trusted faculty advisor or mentor
- A resident in your desired specialty
- A supportive peer who knows your values well
Ask them:
- “Does anything about this order surprise you?”
- “Do you see any potential blind spots in my reasoning?”
Incorporate feedback where it clarifies your thinking, but remember:
- They will not live your life, you will.
- Don’t rank a program higher just because a mentor loves it or it’s their alma mater.
- Don’t downgrade a program that fits you just because it’s less famous.
Step 5: Finalizing a Strategic, Authentic Rank List
As the NRMP Rank Order List (ROL) deadline approaches, it’s time to refine and stress test your final rankings.
Put the Match Algorithm to Work for You
Because the Match Process favors the applicant’s preferences:
- Rank your lists in the exact order you want them, from most to least preferred.
- Do not move a program up simply because you think it’s “easier” to match there.
- Do not move a strong “reach” program down just because you’re worried it’s unrealistic.
You lose nothing by ranking a dream program #1; if they don’t rank you, the algorithm simply moves to your #2 choice.
Stress Test Each Ranking Position
Starting from the top of your list, ask:
- “If I matched at Program #1 and never found out about offers from #2–5, would I be happy?”
- “If I matched at Program #3, would I regret not having ranked Program #2 higher?”
- “How would I feel if I matched at the last program on my list?”
Consider realistic scenarios:
- Matching away from family vs. staying close but with weaker training.
- Choosing stronger academic opportunities vs. better lifestyle.
- Prioritizing location in a city you love vs. a program with better reputation.
These tradeoffs are personal; there is no universally “correct” Rank List Strategy—only one that fits your life and values.
Practical Tips for the Final Submission Phase
- Double-check for errors: Ensure all programs and codes are correct in the NRMP R3 system.
- Use the certification function carefully: You can change your list until the deadline, even after certifying, but don’t wait until the last hour.
- Have a backup: If you’re dual applying or ranking preliminary/advanced programs, verify you’ve aligned them appropriately (e.g., advanced program + prelim year).
Most importantly, once you submit a list you feel at peace with, give yourself permission to let go. The work is done.
Step 6: Managing Stress, Expectations, and Post-Submission Anxiety
Even with a strong Rank List Strategy, the waiting period before Match Day can be stressful.
Normalize the Emotions
It is common to feel:
- Second-guessing and “what-if” thinking
- Anxiety about going unmatched
- Envy or comparison with peers’ interview lists
Remind yourself:
- You crafted the best list you could with the information you had.
- The algorithm is designed to honor your preferences.
- Your worth as a future physician is not defined by a single program’s name.
Healthy Ways to Cope While You Wait
- Reconnect with non-medical hobbies and relationships.
- Maintain sleep, exercise, and healthy eating—residency will test your baseline habits.
- Avoid obsessively rechecking your submitted list.
- If anxiety is overwhelming, consider speaking with a counselor or mental health professional.
Planning for All Outcomes
It’s wise—not pessimistic—to understand contingencies:
- Know the SOAP (Supplemental Offer and Acceptance Program) process if you’re in a system that uses it, in case of not matching.
- Reflect on how you’d adapt if you matched at a lower-ranked program: who you’d lean on for support, how you’d maximize opportunities there, and how you’d protect your well-being.
Being mentally prepared helps you handle any Match outcome with resilience and professionalism.
FAQs: Residency Rank List, Match Strategy, and Career Development
Q1: How many programs should I rank on my Residency Rank List?
There’s no strict “correct” number, but data show that ranking more programs generally increases your chances of matching. For competitive specialties, many applicants rank 10–15 programs or more, while for less competitive fields some may rank fewer. Only rank programs where you’d genuinely be willing to train. Do not add programs “just to fill space” if they’re truly unacceptable to you.
Q2: Should I ever rank a highly prestigious program above a better overall fit?
You should prioritize true fit over name recognition. Prestige can offer benefits (network, fellowship options, academic reputation), but if the culture, location, or training style clashes with your needs or values, you may be unhappy or burn out. A slightly less famous program that aligns better with your goals and lifestyle will often support more sustainable and successful career development.
Q3: How much should location influence my Rank List Strategy?
Location is a major factor and valid priority. Consider:
- Support systems (partner, children, parents)
- Cost of living and safety
- Long-term plans (where you might want to practice)
If location is critical (for family or personal reasons), give it appropriate weight. Just be honest about what tradeoffs you’re willing to make regarding program reputation, case mix, or fellowship opportunities.
Q4: Can I change my residency rank list after I certify it in the NRMP system?
Yes—until the official NRMP deadline. You can log back in, adjust your list, and re-certify as many times as needed before the cutoff. After the deadline passes, your last certified list becomes final and cannot be changed. Plan to finalize a few days before the deadline to avoid last-minute technical issues.
Q5: How can I tell if a program’s culture is truly supportive and not just “marketed” that way?
Look for:
- Consistency between what leadership says and how residents talk about their day-to-day lives.
- How residents respond to questions about fatigue, workload, and conflict—do they give specific examples or vague reassurances?
- Evidence of concrete wellness policies (not just slogans), such as backup coverage, mental health access, protected didactics, and responsiveness to resident feedback.
- Transparency about past challenges (e.g., duty hour violations) and how the program addressed them.
Patterns across multiple residents and interactions often reveal more than a polished presentation.
Thoughtfully crafting your Residency Rank List is one of the most empowering steps you can take during the Match Process. By clarifying your priorities, systematically researching programs, critically reflecting on interview experiences, and ranking them in the honest order of your preference, you align your residency training with the kind of physician—and person—you hope to become.




















