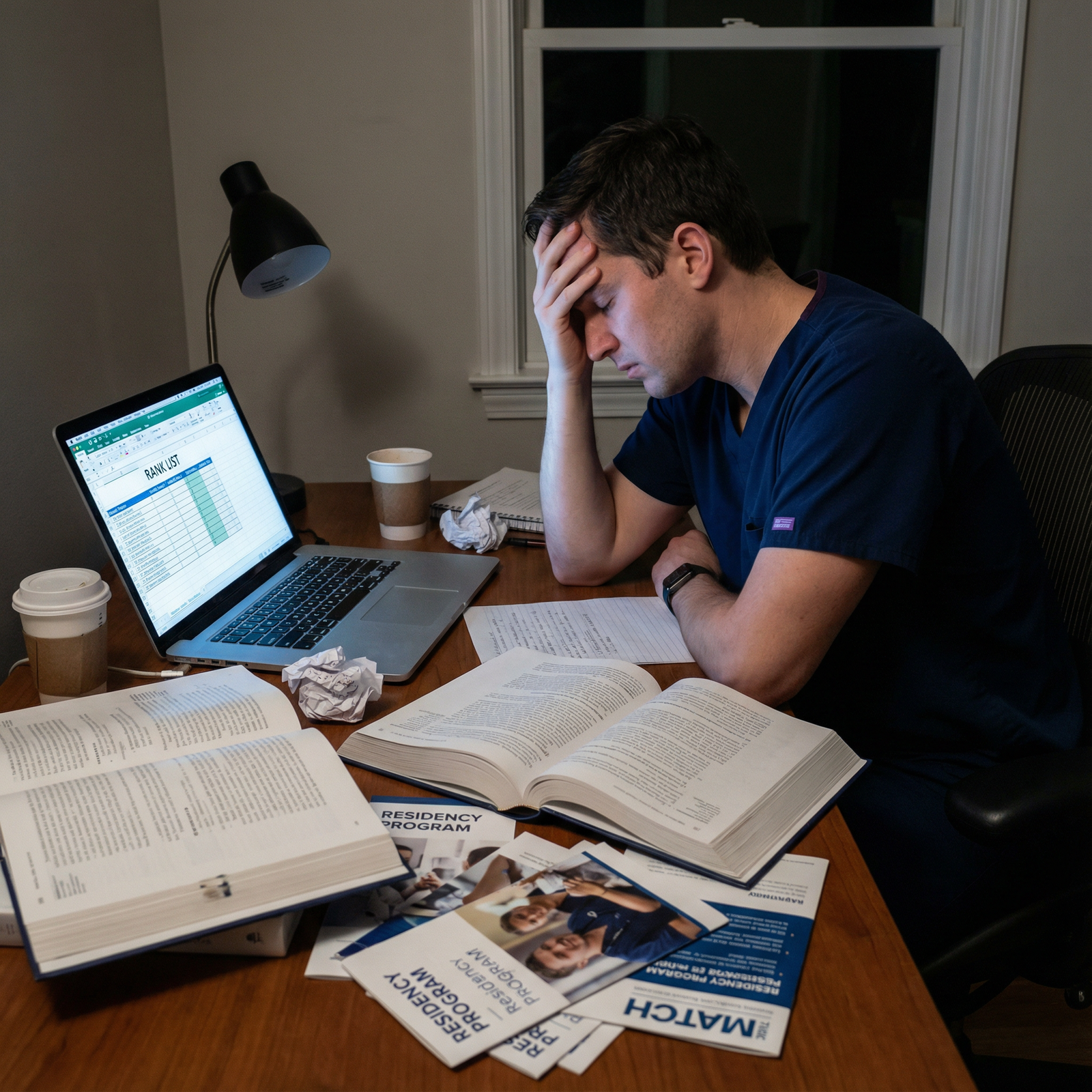
Most people rank physician‑scientist tracks vs categorical spots exactly backwards. And it costs them the career they actually want.
Let me be blunt. The default advice you hear in the hallway—“Just rank whatever’s ‘stronger’ overall” or “Always prioritize location” or “Research tracks are only for superstars”—is lazy thinking. If you want a serious research career, or even to keep that door genuinely open, you cannot afford lazy.
You are not just ranking programs. You are ranking future versions of yourself:
- One who is protected for research.
- One who is a full‑time clinical workhorse.
- Or one who has quietly given up on ever leading a lab, even if you will not admit it yet.
Let me break this down specifically, because this decision is more nuanced than “MD/PhD → research track, everyone else → categorical.”
1. First, get brutally clear on your real endpoint
Before you even touch the rank list, you need to define the endpoint you are optimizing for. Not vibes. Not prestige. The job you want at 40.
There are roughly four realistic endgames here:
Pure physician‑scientist:
- 70–80% research, 20–30% clinical
- K‑award / equivalent early‑career grant
- Tenure‑track or equivalent appointment at a research‑intensive institution
Hybrid academic clinician‑educator with meaningful research:
- ~50/50 or 60/40 clinical/research
- Some grants, some publications, a niche
- Academic title, protected time, but not lab‑empire level
Primarily clinician, research‑friendly:
- 80–90% clinical
- Occasional projects, collaborations, maybe some QI or clinical research
- Possibly community‑academic hybrid
Pure clinician (no real research plans):
- 100% clinical
- Teaching or leadership maybe, but no ongoing research responsibility
Now, here is the uncomfortable truth:
Your choice between physician‑scientist tracks and categorical spots should map ruthlessly onto which of these you actually want—and are willing to work for—not what sounds impressive on paper.
If your honest target is #3 or #4, chasing the most protected‑time research track at all costs is silly and possibly harmful.
If your target is #1 and you rank a strong categorical program above weaker but research‑structured options, you are probably sabotaging future you.
So ask yourself three specific questions and write the answers down:
- In an ideal world, what percent of my time do I want to spend doing research at age 40?
- Am I willing to accept more training years and lower early‑career salary for a real shot at that?
- Do I actually enjoy the process of research (grant writing, paper revisions, failed experiments), or just the idea?
If you cannot answer those honestly, you are not ready to rank.
2. What “physician‑scientist track” actually means vs. buzzword nonsense
Programs use “physician‑scientist,” “research track,” “investigator pathway,” “ABIM research pathway,” and “scholarly concentration” interchangeably—and that muddies the water.
You need to separate marketing from structure.
| Feature | True Research Pathway (e.g., ABIM) | Research‑Friendly Categorical |
|---|---|---|
| Formal structure | Yes, defined sequence & requirements | Variable, often informal |
| Guaranteed protected time | Typically 1.5–3 years | Often negotiable, not guaranteed |
| Linked fellowship pathway | Usually yes | Often no, or ad hoc |
| Salary support mechanism | Built into track | Case‑by‑case, grant‑dependent |
| Promotion of research career | Core mission | Variable priority |
If you are in internal medicine, pediatrics, or a field that uses ABIM/ABP research pathways, these tracks may:
- Shorten clinical residency time
- Lock you into research time during residency + fellowship
- Extend total training, but front‑load research skill‑building
In surgery, OB/GYN, EM, etc., “physician‑scientist track” might mean:
- Intercalated research year(s)
- T32‑funded slots
- Or just a “research‑heavy environment” with unclear protection
You must do the unglamorous work of asking programs explicitly:
- Is this an ABIM/ABP research pathway or equivalent, or just a label?
- How many months of protected time are contractually guaranteed?
- How many physician‑scientists have actually come out of this track in the last 5–10 years—and where are they now?
If they cannot answer cleanly, you are not looking at a true physician‑scientist track. You are looking at a good categorical with research support. Which is fine. As long as you treat it that way when ranking.
3. The real tradeoffs: research track vs categorical, point by point
Let us compare what you are actually trading.

| Category | Value |
|---|---|
| Research Track | 24 |
| Research-Friendly Categorical | 6 |
| Standard Categorical | 2 |
(Values approximate typical total months of real research time over residency + early fellowship.)
A. Time and flexibility
Research track:
- Longer overall training (often +1–2 years).
- You lock in earlier to an investigative trajectory and often to a subspecialty.
- Easier to build deep, long‑term projects and preliminary data for K‑level grants.
- Harder to pivot specialties or move to a different style of career mid‑way.
Categorical:
- Standard training length.
- Maximal flexibility—fellowship vs no fellowship, subspecialty shifts, academic vs community.
- But you usually squeeze research into electives, nights, and “optional” blocks.
- You are constantly fighting clinical demands for time and energy.
Here is the key:
If you are even half serious about an RO1‑style or K‑style career, you cannot build that on scraps of time during a standard categorical without strong structural support. I have seen a few people pull it off. They are outliers and they usually pay for it with burnout.
B. Signaling and mentorship
Programs that invest in true physician‑scientist tracks are explicitly signaling:
- “We expect you to do serious research here.”
- “We will pair you with senior investigators.”
- “Your success will reflect directly on our track.”
You become part of a small, watched cohort. That cuts both ways.
Pros:
- High‑level mentors take you seriously.
- You get looped into grants, projects, and collaborations faster.
- You often get priority for lab space, resources, and high‑value meetings.
Cons:
- Expectations are real. Weak productivity stands out.
- It is harder to quietly decide “actually I am done with research” without raising eyebrows.
In a categorical spot, you have to build that pipeline from scratch. Different skill set. Some people thrive on that independence. Others disappear in the clinical machine.
C. Funding and early‑career runway
People underestimate this part.
Physician‑scientist tracks often:
- Tie you into departmental or T32 funds during your research years.
- Give you salary while you develop projects that lead to K‑level applications.
- Put you in front of grant writers and core facility directors by default.
Strong categorical programs with real research support can mimic this—but it is very program‑dependent, and the burden is on you to hustle.
If your long‑term endpoint depends on K‑ or equivalent funding, having 18–36 continuous months of protected, funded research time early on is a massive advantage. Not subtle. Massive.
If, on the other hand, you want to publish some solid clinical work and be the “research person” in a community group, the categorical path is not just sufficient—it is probably more sensible.
4. How competitiveness and your CV should reshape the rank list
Let me be very direct: some applicants overestimate their research trajectory; others wildly underestimate it.
You should strongly favor physician‑scientist tracks (rank them higher) if:
You already have:
- Multiple first‑author papers in a coherent area (not just random case reports).
- Strong letters from PIs who call you “among the best in 10 years.”
- A clear niche you can articulate in 60 seconds: “I work on X problem using Y methods in Z disease.”
You felt at home talking with faculty about:
- Mechanisms, trial design, or methodology.
- Long‑term grant strategy.
- How to sequence residency → fellowship → K‑award → first RO1.
Your stress is not “will I do research?” but “how do I get enough protected time to make it count?”
That person leaves money on the table by ranking pure categoricals over well‑structured research tracks at credible institutions, unless location or personal constraints are truly non‑negotiable.
You should lean toward categorical spots (or de‑prioritize research tracks) if:
Your “research” is:
- One poster.
- Maybe a middle‑author retrospective.
- Significant gaps in involvement.
On interview day, you struggled to articulate:
- A specific research focus.
- Why you need structured research time versus just “liking academics.”
When you shadowed full‑time investigators, the life did not appeal. The grinding, the rejected grants, the constant pressure to publish.
Could you still grow into a physician‑scientist from a categorical start? Yes. It is just a steeper climb, and you should be honest about probabilities.
5. Concrete ranking scenarios: how to think through them
Let us walk through the scenarios I see every year.
Scenario 1: Strong research track at “mid‑tier” vs elite categorical
Example (fictional, but you have seen this story):
- Program A: Mid‑tier university hospital, ABIM research pathway, 2 years protected post‑IM, strong T32, solid but not famous brand.
- Program B: Top‑5 name‑brand IM residency, categorical, “you can find mentors, many people do research.”
You want: 70–80% research at age 40, R01‑style lab or equivalent clinical‑research program.
My answer:
If Program A’s track is robust—documented graduates in K/R careers, real protected time, mentorship you respect—you should strongly consider ranking A above B. The name recognition of B will not compensate for structurally missing research time and support, unless B has a de facto research pathway under a different label.
I have watched too many trainees choose “prestige now” over “infrastructure later” and then crash into full‑time attending responsibilities with no K‑ready data.
Scenario 2: Research track in a city you dislike vs categorical in your ideal location
- Program C: Physician‑scientist track, great mentorship, city you actively dislike, partner’s career would suffer.
- Program D: Categorical, decent academics, city where your support network is strong.
You want: Unclear between hybrid academic (#2) and primarily clinical (#3).
This is where it gets personal. A few hard truths:
- Longitudinal support (family, partner, mental health) matters more for your career durability than a T32.
- Misery in location bleeds into your productivity. I have watched it blunt very promising early scientists.
If you are ambivalent about a hardcore research endpoint, and the location sacrifice is severe, ranking D above C can be rational. You can still pick up serious research in a categorical if the program is at least moderately academic and you are proactive.
Scenario 3: Multiple “research tracks” with wildly different quality
Not all “physician‑scientist” labels are equal.
You might have:
- Program E: True ABIM research pathway, clear curriculum, 5–10 graduates now in K/R funded roles.
- Program F: Research track with nominal extra elective time, one T32 slot, vague promises.
- Program G: No named track, but one division with a powerhouse PI who essentially runs a mini‑pipeline of mentees.
You want: #1 or #2 endpoint.
My hierarchy in this situation:
- E (if mentorship matches your interests)
- G (if that PI’s group is really that strong and track record is proven)
- F (unless you confirm it is more than branding)
Do not get seduced by the label. Look at outcomes.
6. How to interrogate programs (quietly) before finalizing your rank list
You should be borderline annoying about this in January–February. Not on interview day. After.
Use follow‑up emails, second looks (virtual or in‑person), and current residents/fellows to get very specific answers.
Here is exactly what to ask different people.
Ask current research‑track residents/fellows:
- “How many truly protected months have you had so far? Not just on paper—actually not being pulled to the floor or clinic.”
- “How many papers / major abstracts have you gotten out of your research time?”
- “Who are your primary mentors and how often do you meet with them?”
- “Have any residents here recently gotten K‑awards or equivalent? Can you tell me who they are?”
- “If you could re‑rank your programs now, would you still choose this track?”
If you hear:
- “Protected time is… variable,” or
- “We sometimes get pulled to service a lot,”
that tells you what you need.
Ask faculty:
- “How do you decide which residents are selected for the physician‑scientist track?”
- “What happens if a research‑track resident struggles or wants to pivot out?”
- “What department‑level resources (bridge funding, startup, core access) are available for graduating fellows who stay on faculty?”
- “What proportion of your last 5–10 research‑track grads are still in research‑intensive roles?”
You are looking for specific numbers and names, not airy answers like “many go on to successful careers.”
7. The personal‑life layer you are secretly weighting
Nobody likes to talk about this on the record, but it absolutely drives ranking decisions:
- Partner’s career and location constraints
- Kids / childcare
- Elderly parents
- Your own tolerance for being far from any support for 7–9 years
Physician‑scientist tracks often glue you to a single institution for IM + fellowship + research years. That might be:
- A blessing (continuity, deep roots, stable mentors).
- A trap (frozen in a city or environment that is misaligned with your life).
It is not “unprofessional” to let these weigh heavily. It is smart. Just be deliberate:
- If you know you cannot stay long‑term in City X, ranking a track that locks you into 7–8 years there is risky.
- If you have strong local support that will keep you functional and sane, ranking a slightly weaker research structure in that city above a “perfect” track elsewhere can be the right move.
The key: do not pretend you are ranking in a vacuum. Be explicit about what trade you are making.
8. How your ranking strategy should actually look
Let me give you a rough template. You of course adjust based on your specific list.
If you are fully committed to a physician‑scientist career (endpoint #1):
Group programs into tiers by research infrastructure and track strength, not brand name.
- Tier 1: Proven research track, multiple recent K/R‑funded grads.
- Tier 2: Strong research culture, some protection, good mentorship.
- Tier 3: Mainly clinical with ad hoc research.
Within Tier 1, rank by:
- Mentor fit in your area.
- City/life constraints.
- Fellowship pipeline in your field.
Only then bring in:
- Prestige
- Minor quality‑of‑life issues
- Marginal salary differences
In practice, this often means:
- Top of your list: best research tracks where you have real mentors, even if institution is “mid‑tier.”
- Mid list: elite categorical programs with robust research histories.
- Lower list: good clinical programs that keep the door cracked open but will not drive your research.
If you are leaning hybrid (#2) or research‑interested clinician (#3):
Group programs by flexibility:
- Programs where you can do credible research without being chained to a track.
- Programs where physician‑scientist track is “all in” culturally.
- Programs where research is window dressing.
Rank higher:
- Places with optional but strong research infrastructure, where you can adjust your intensity up or down without burning bridges.
Be honest:
- If you are 60/40 between academic and community, weighting location and clinical training slightly above research structure is reasonable.
In this scenario, a stellar categorical in a supportive academic environment will usually beat a rigid research track you feel ambivalent about.
9. Red flags that should push a program down your list
I have seen these burn people:
- Research‑track residents are indistinguishable from categorical clinically—no real protected blocks ever materialize.
- Residents quietly advise you: “If you really want to do research, go somewhere else.”
- Program leadership cannot name a single recent graduate in an R‑funded or equivalent role.
- You get hand‑waving instead of concrete outcomes: “Our grads do all kinds of things.”
- The “track” is clearly a marketing response to other institutions, not built from the ground up.
If you see this pattern, it does not mean do not rank the program at all. It means:
Treat it as a normal categorical with a research‑friendly attitude, not as a true physician‑scientist slot.
10. A quick visual: choosing paths over time

| Step | Description |
|---|---|
| Step 1 | Rank List Decision |
| Step 2 | Structured Research Training |
| Step 3 | Categorical Residency |
| Step 4 | Early K-Ready Productivity |
| Step 5 | Primarily Clinical Career |
| Step 6 | Physician-Scientist / Hybrid Academic |
| Step 7 | Choose Research Track? |
| Step 8 | Self-Built Research? |
This is simplified, but it captures the reality: you can reach a research career from both starting points, but the path from categorical usually demands that you bootstrap the structure yourself.
FAQs
1. I am an MD‑only with limited research. Is ranking physician‑scientist tracks high unrealistic?
Not automatically. I have seen MD‑only residents in research tracks thrive, if they come in hungry, with at least some substantive exposure (even if not heavily published) and a clear vision. But if your research interest is vague and you do not yet know what you enjoy scientifically, locking into a rigid track can be premature. In that case, a strong categorical in a research‑dense environment may give you space to mature before committing.
2. If I choose a categorical spot, can I still become a serious physician‑scientist later?
Yes, but it requires discipline and structural support. You will need to aggressively seek mentors early, use electives for research, pursue research‑heavy fellowships (often T32‑linked), and possibly take dedicated research years in fellowship. People do it. The ones who succeed treat research like a second job during residency, not a hobby.
3. Does program prestige ever outweigh weaker research structure for aspiring physician‑scientists?
Sometimes. If the elite program has deep bench strength in your exact niche and a track record of launching researchers—even from categorical spots—that can compensate. But “big name, minimal structured protection” is a trap if you are relying on institutional glow to carry a weak infrastructure. Look at actual graduates, not reputation.
4. What if I am undecided and fear closing doors by choosing either track?
You are not actually closing as many doors as you think. Choosing a research track narrows your flexibility somewhat but strengthens your research odds. Choosing categorical preserves flexibility but shifts more of the research burden onto you. In true uncertainty, prioritize: programs where both categorical and research‑oriented residents have done well, plus locations where you and your support system can realistically thrive for years.
5. Bottom line, how should I decide between a research track and a categorical spot when torn between two programs I like?
Ask yourself: “If I wake up five years from now doing 80–90% clinical work with minimal research, will I feel relieved or disappointed?”
If relieved, rank the stronger overall categorical higher, paying attention to teaching, mentorship, and location. If disappointed, give weight to real protected time, mentor fit, and research outcomes—and let that physician‑scientist track climb above a slightly shinier categorical on your list.
Key takeaways:
- Align your rank list with the career you actually want at 40, not the one that sounds good this month.
- Judge physician‑scientist tracks by structure, protected time, and graduate outcomes—not by labels or prestige alone.
- Decide consciously how much life‑logistics and location you are willing to trade for research infrastructure, and rank accordingly.




















