
Selecting and ranking Residency Programs is one of the most consequential decisions in your medical education and early Career Development. Your choice will shape your clinical skills, subspecialty options, professional network, future job prospects, and Work-Life Balance for years to come.
While the process can feel overwhelming, a structured, criteria-based approach makes it far more manageable. Instead of relying on vague impressions or prestige alone, you can systematically evaluate each program against the factors that matter most to you—training quality, culture, Diversity in Medicine, location, support, and long-term fit.
This guide walks through essential criteria for evaluating and ranking residency programs during the Residency Match and Applications phase. Use it as a framework to organize your thoughts, compare programs fairly, and build a rank list that genuinely reflects your goals and values.
Program Reputation and Outcomes: Beyond Name Recognition
Program reputation often dominates early conversations about residency, but it is more nuanced than “top-tier” versus “community.” For your purposes, the key question is: How well does this program prepare residents for the careers they want?
Core Elements of Program Reputation
ACGME Accreditation
- Confirm the program is fully accredited by the ACGME.
- Check for any citations or probation history on the ACGME website.
- For new programs, ask directly about accreditation status and oversight.
Graduate Outcomes
- Where do graduates go?
- Fellowship programs (academic vs community; highly competitive vs general).
- First job placements (academic centers, community hospitals, private practice, rural/urban).
- Ask for:
- A list of fellowships and institutions where recent graduates matched.
- Typical career paths—e.g., hospitalist, outpatient, subspecialist, researcher, educator.
- Where do graduates go?
Program Stability and Leadership
- Longevity of Program Director (PD) and core leadership.
- Recent major changes: mergers, hospital closures, drastic expansion.
- Resident perception of leadership transparency and responsiveness.
How to Evaluate Reputation Effectively
- Use multiple data sources
- FREIDA, Residency Explorer, program websites.
- Doximity and other ranking sites can be a starting point, but don’t overvalue them.
- Talk to people
- Ask attendings and fellows about a program’s clinical rigor and reputation.
- During interviews, ask residents:
- “Would you choose this program again?”
- “How prepared did recent grads feel for independent practice or fellowship?”
Reputation should inform your ranking—but not dominate it. A slightly less “famous” program that aligns with your goals, values, and lifestyle may be a far better long-term fit.
Curriculum and Training Structure: How You Will Actually Learn
The curriculum is the backbone of your Medical Education during residency. It determines what you see, how much responsibility you have, and how prepared you’ll be at graduation.

Core Curriculum and Clinical Exposure
Breadth and depth of training
- Does the program cover the full scope of your specialty (e.g., for Internal Medicine: inpatient, outpatient, ICU, subspecialty clinics, procedures)?
- Are there sufficient volumes and acuity to build confidence and competence?
- Are there unique populations (VA, safety net hospitals, pediatrics vs adult, OB vs no OB, etc.)?
Clinical settings
- Tertiary/quaternary academic center vs community vs hybrid.
- Exposure to different practice environments (VA, county, private, rural).
- Balance of inpatient vs outpatient based on your specialty’s board requirements.
Responsibility and autonomy
- Progressive responsibility from PGY-1 to PGY-3/4.
- Opportunities to lead teams, run codes, supervise juniors.
- Clear supervision policies that ensure safety while promoting growth.
Flexibility, Electives, and Individualization
Elective time
- How many elective months are available, and when (early vs late in training)?
- Can you repeat electives, or do they require variety?
- Are away/audition electives supported?
Tracks and pathways
- Primary care, hospitalist, research, global health, medical education, leadership, quality improvement tracks, etc.
- Structured curricula for these pathways (not just a label).
Customizing your training
- Can you tailor your schedule toward specific career goals (e.g., more ICU for critical care fellowship, more clinic for primary care)?
- Is there mentorship to help plan rotations strategically?
Board and Exam Preparation
Built-in board prep
- Dedicated board review sessions, question banks, or didactic series.
- Program’s pass rates on board exams—are they stable and above national averages?
Protected didactic time
- Are conferences and lectures truly protected (i.e., pages triaged, minimal clinical interruptions)?
- Regular schedule of:
- Morning report
- Grand rounds
- M&M conferences
- Journal clubs
- Simulation sessions
A strong curriculum should balance service and education, provide progressive autonomy, and offer enough flexibility to support your specific Career Development path.
Faculty, Mentorship, and Professional Development
The people who train you—faculty and senior residents—will profoundly shape your residency experience, career choices, and confidence as a physician.
Evaluating Faculty Quality and Engagement
Faculty expertise
- Range of subspecialties represented.
- Faculty with national or regional leadership roles (guidelines committees, academic societies).
- Presence of clinician-educators with a clear focus on teaching.
Teaching culture
- Do residents describe faculty as approachable and invested?
- Are there regular teaching rounds, bedside teaching, and feedback?
- Is there a structured evaluation system for faculty teaching quality?
Mentorship and Career Coaching
Formal mentorship programs
- Assigned mentors vs self-selected mentors.
- Frequency of scheduled check-ins.
- Career advising tailored to:
- Fellowship-bound residents.
- Those pursuing community practice.
- Those interested in research or medical education.
Access to role models
- Faculty who share your interests (e.g., global health, health policy, informatics).
- Mentors who reflect Diversity in Medicine in terms of background, identity, and career paths.
- Opportunities to see different career models (full-time clinical, clinician-educator, physician-scientist).
Career Development support
- Workshops on CV building, interview prep, and negotiation for post-residency jobs.
- Guidance on fellowship applications, letters of recommendation, and networking.
Strong mentorship and faculty support can compensate for other weaknesses in a program; the opposite is rarely true.
Work-Life Balance, Wellness, and Resident Culture
Residency is demanding by design, but the environment should be sustainable and humane. Work-Life Balance is not a luxury—it’s critical for your learning, mental health, and longevity in the profession.
Clinical Workload and Schedule
Duty hours
- Consistent adherence to ACGME duty hour regulations.
- Ask residents how often they actually violate hours, even if not formally reported.
- How does the program respond when duty hour issues arise?
Call structure
- Night float vs 24-hour call vs hybrid.
- Frequency of nights and weekends.
- Transition from heavier PGY-1 call to more senior responsibilities rather than just more hours.
Service vs education
- Are residents primarily “scut workers” or integrated as learners?
- Support staff: presence of scribes, phlebotomy, transport, advanced practice providers.
- Workload per resident—patient caps, typical census, number of admissions per call.
Wellness and Support Systems
Formal wellness initiatives
- Wellness curricula, resilience training, or Balint groups.
- Access to confidential mental health services and counseling.
- Retreats, social events, and built-in time for team bonding.
Paid time off and leave policies
- Vacation days and how easily they can be scheduled.
- Parental leave policies, including for residents having children during training.
- Flexibility for major life events and health issues.
Resident culture
- How do residents describe their relationships with each other?
- Collegial vs competitive.
- Social connections outside of work.
- Do residents feel safe speaking up about concerns?
- Is burnout openly acknowledged and addressed?
- How do residents describe their relationships with each other?
Ask residents directly: “What are the hardest parts of this program?” and “What has the program done to improve wellness in the past 1–2 years?” Their answers are often illuminating.
Location, Community, and Lifestyle Fit
Location is more than city vs countryside—it affects your daily life, support system, and even patient population exposure.
Geographic and Community Considerations
Urban vs suburban vs rural
- Urban centers: often higher volume, more diverse patients, specialized services; usually higher cost of living.
- Suburban/rural: closer-knit communities, broader scope of practice, sometimes fewer subspecialties on-site.
Cost of living and salary
- Compare resident salary to cost of housing, transportation, childcare, and basic expenses.
- Ask residents if they can live reasonably on their salary without excessive moonlighting.
Support networks
- Proximity to family, friends, or a partner’s work.
- Social and cultural amenities important to you (places of worship, community organizations, hobbies).
Community Engagement and Patient Population
Patient demographics
- Socioeconomic diversity, language diversity, immigrant/refugee populations.
- Exposure to underserved communities and health disparities.
Community partnerships
- Outreach clinics, mobile health programs, school-based clinics, free clinics.
- Opportunities for advocacy, public health work, and longitudinal community projects.
Training in a setting that aligns with your long-term goals—such as serving underserved populations or working in a specific region—can give you a strong foundation for your future practice.
Research, Scholarly Activity, and Academic Opportunities
If you are considering a subspecialty fellowship, academic medicine, or research-focused career, the program’s scholarly environment is crucial to your Career Development.

Research Infrastructure and Support
Access to projects
- Are there ongoing clinical, translational, or basic science projects with room for resident involvement?
- Is QI/QA (quality improvement/assurance) integrated into required scholarly activity?
Resources
- Research coordinators, biostatistical support, and IRB assistance.
- Protected time for research—especially for residents in research tracks.
- Internal funding or small grants for resident projects.
Presentation and publication
- Percentage of residents presenting at regional/national conferences.
- Typical number of publications, posters, or abstracts per graduating resident.
- Support for conference attendance:
- Time off.
- Funding for travel, registration, and lodging.
Academic and Teaching Opportunities
Teaching roles
- Opportunities to teach medical students, junior residents, or other learners.
- Formal training in medical education (teaching skills workshops, educator tracks).
Advanced degrees or certificates
- Options for MPH, MSc, MEd, MBA, or certificates in education, QI, or leadership.
- Institutional support or partial tuition coverage.
You don’t need to be research-focused to benefit from scholarly activity; even clinically oriented residents gain from learning to ask and answer meaningful questions about patient care and systems improvement.
Diversity, Inclusion, and Equity in Residency Programs
Diversity in Medicine is not just a buzzword—programs that value diversity and practice equity often provide richer learning environments and better patient care.
Evaluating Diversity and Representation
Resident and faculty demographics
- Is there visible diversity across race, ethnicity, gender identity, sexual orientation, disability status, and background?
- Are underrepresented groups present in leadership roles (chief residents, PDs, APDs, department chairs)?
Recruitment and retention efforts
- Pipeline programs, visiting student scholarships, or second-look events for underrepresented applicants.
- Programs to support retention and advancement of diverse residents and faculty.
Inclusion, Climate, and Equity Efforts
Training and curriculum
- Explicit teaching on health disparities, structural racism, LGBTQ+ health, disability in healthcare, and cultural humility.
- Integration of social determinants of health into clinical teaching.
Institutional culture
- How are microaggressions, discrimination, or harassment handled?
- Existence of safe reporting systems and follow-through on concerns.
- Active DEI committees or task forces with resident representation.
Support networks
- Affinity groups (e.g., SNMA, LMSA, APAMSA, Pride/LGBTQ+ groups, women in medicine networks).
- Mentorship for residents from underrepresented backgrounds.
Ask residents: “Do you feel the program is inclusive?” and “Can you share examples of how the program supported residents in challenging situations?” Their real stories matter more than mission statements.
Resident Support, Resources, and Program Infrastructure
Practical resources can substantially affect your day-to-day well-being and educational experience.
Educational and Clinical Resources
Learning tools
- Access to major medical journals and databases (UpToDate, AccessMedicine, etc.).
- Simulation centers for procedures, communication skills, and team training.
- Regular skills labs for procedures relevant to your specialty.
Technology and support
- User-friendly EMR systems with adequate training.
- IT support and on-call help for EMR or hardware issues.
- Availability of dictation, templates, and other efficiency tools.
Financial and Practical Support
Salary and benefits
- Health, dental, and vision insurance.
- Retirement contributions (even small ones early on are valuable).
- Meal stipends, parking, and transportation benefits.
Licensing and exam support
- Coverage or partial reimbursement for licensing fees, DEA, board exams, and required courses (ACLS, BLS, PALS, etc.).
- Education funds for books, question banks, and courses.
Family and life logistics
- Childcare options, lactation rooms, and family-friendly policies.
- Schedules that consider major life events when possible.
Programs that invest in resident resources signal that they view you not only as labor, but as learners and future colleagues.
Interpreting Match Statistics and Competitiveness
Evaluating a program’s match and applicant statistics can help you understand both your chances of matching and how well a program supports graduates in their next steps.
Program Competitiveness and Fit
Applicant metrics
- Average Step scores, publications, and class rank of matched residents (when shared).
- Proportion of DO vs MD graduates, international medical graduates, and home institution students.
Interview impressions
- Did you feel welcomed and respected?
- Were interviews conversational and focused on mutual fit, or one-sided and impersonal?
Graduate Match Outcomes and Success
Fellowship match data
- Where and in what fields grads match for fellowship.
- Are people matching into the types of positions you aspire to?
Career diversity
- Graduates entering community practice, academic roles, hospitalist work, or subspecialty practice.
- Support for non-traditional paths (health policy, administration, industry, digital health, etc.).
Match statistics are useful context, but they must be interpreted in light of your own application strength and priorities. Don’t avoid a “competitive” program solely out of fear—if it’s a strong fit, it may still be worth ranking highly.
Aligning Programs with Your Personal Preferences and Values
After you evaluate all the “objective” factors, you still need to answer a more personal question: Where will I thrive as both a physician and a person?
Reflective Questions to Guide Your Rank List
Ask yourself:
Career alignment
- Does this program support my likely career path (fellowship vs general practice, academic vs community)?
- Can I see myself practicing the way recent graduates do?
Daily life and Work-Life Balance
- Can I imagine living in this city for 3–7 years?
- Is the call schedule compatible with my personal and family needs?
Culture and “gut feeling”
- Did I feel like I could be myself during interview day?
- Did I leave thinking, “These are my people”?
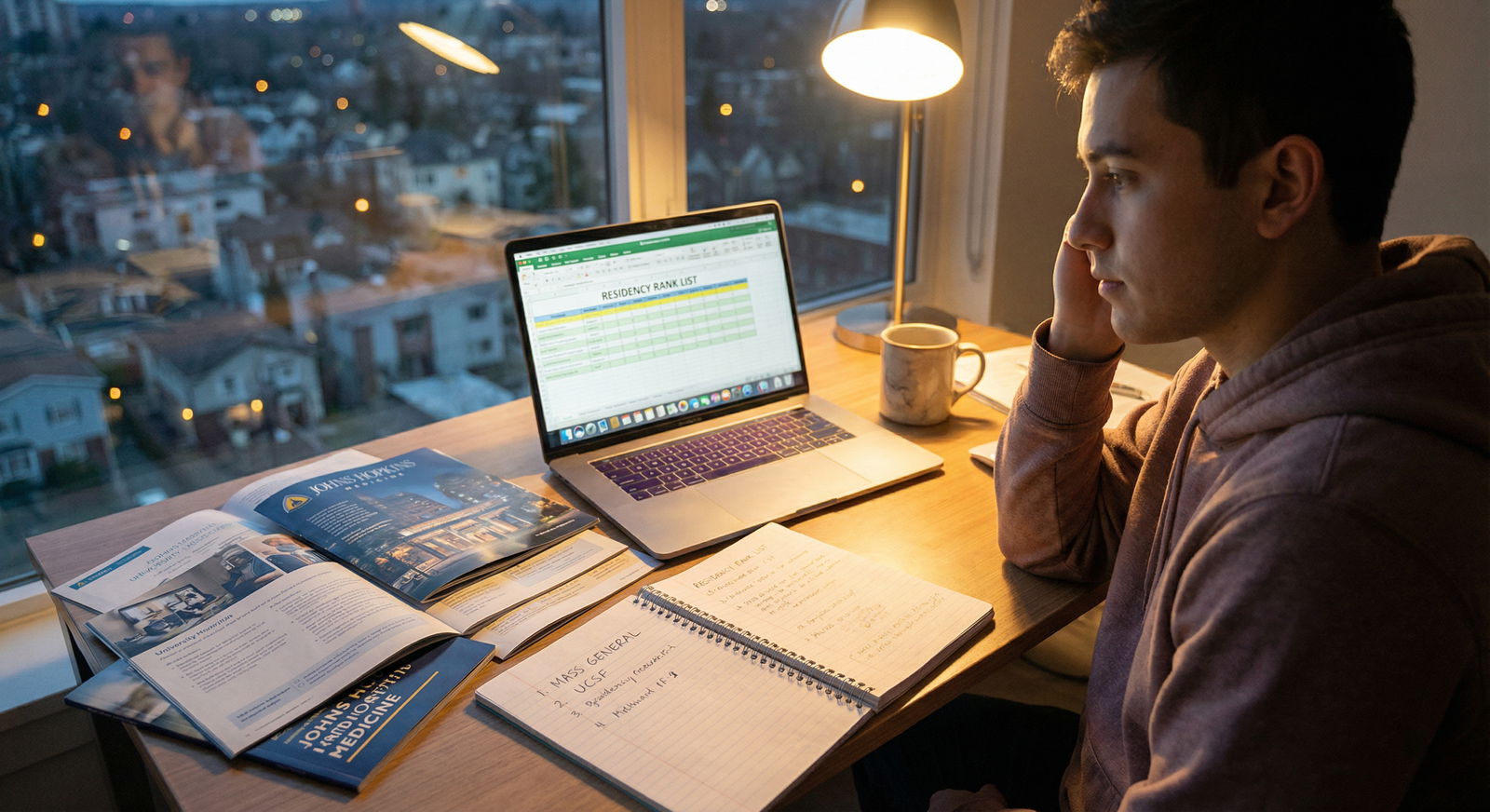
A Practical Strategy for Ranking
Create a spreadsheet or ranking rubric
- Columns for key categories: reputation, curriculum, faculty/mentorship, Work-Life Balance, location, research, Diversity in Medicine, support/resources, “fit.”
- Score each program (e.g., 1–5) and add brief notes.
Weight what matters most to you
- If fellowship is your top priority, weight research and graduate outcomes more heavily.
- If you value Work-Life Balance or geographic stability, give those factors more weight.
Revisit after some time
- Let your impressions settle, then review notes a week or two later.
- Talk with trusted mentors who know you well and can help identify blind spots.
Remember: the NRMP algorithm is applicant-favorable. Rank programs in true order of your preference, not based on where you think you are “most likely” to match.
FAQs: Evaluating and Ranking Residency Programs
1. How should I start building my list of residency programs to apply to?
Begin with your specialty choice and broad career goals. Use FREIDA and AAMC’s Residency Explorer to identify all ACGME-accredited programs in your specialty. Filter by location preferences, program size, and type (academic vs community vs hybrid). Then, narrow based on factors like fellowship outcomes, research presence, and patient population. Discuss your preliminary list with mentors, who can give specialty-specific advice on realistic ranges and “reach vs safety” programs.
2. What if I’m genuinely torn between two specialties?
If you are early in medical school, prioritize clinical rotations and shadowing in both fields. If you are closer to applying:
- Do away or sub-internship rotations in each specialty.
- Seek honest conversations with residents and attendings about daily life, long-term job prospects, and Work-Life Balance.
- Reflect on which clinical problems and patient populations energize you vs drain you. If the decision remains difficult, some students apply to two specialties, but this requires careful planning and open discussion with advisors to avoid mixed signals.
3. How important is program prestige compared to fit and location?
Prestige can influence certain opportunities (e.g., highly competitive fellowships), but it is only one piece of the puzzle. For many residents, training quality, mentorship, resident culture, and geographic fit end up mattering more. A moderately well-known program where you receive strong mentorship and feel supported can position you better than a “brand-name” program where you are unhappy or overlooked. For most applicants, prioritize programs that will train you well and support your career goals—even if they are not the top-ranked names.
4. What are reliable resources for evaluating residency programs?
Useful tools include:
- FREIDA and Residency Explorer for objective data (program size, call structure, salary, etc.).
- Program websites for curriculum, leadership, and special tracks.
- ACGME site for accreditation and any citations.
- Virtual or in-person open houses and social events.
- Most importantly, conversations with current residents and recent graduates—their candid insights into culture, workload, and support are invaluable and often more informative than any brochure.
5. Should I prioritize Work-Life Balance or training rigor if I can’t find both in one program?
This is a truly personal decision and depends on your resilience, support system, and long-term goals. Extremely rigorous programs may offer exceptional clinical training but carry higher risk of burnout if not balanced by strong support. Programs with very light workloads might compromise exposure and confidence. Look for a sustainable middle ground: robust clinical training with clear evidence that the program actively works to protect resident wellness, adheres to duty hours, and fosters a supportive culture.
Approach residency selection as a major, but manageable, step in your medical journey. By systematically evaluating each program’s reputation, curriculum, mentorship, Work-Life Balance, Diversity in Medicine, and overall fit with your values, you can build a rank list that supports both your professional ambitions and your personal well-being.




















