
How to Rank Residency Programs: Key Factors to Consider for a Successful Match
Navigating the residency Match Process is one of the most consequential steps in your medical training and career development. After years of rigorous study and clinical rotations, you now face decisions that will shape not only the next three to seven years of your life, but also your long‑term professional trajectory.
This guide walks you through how to rank residency programs strategically—integrating personal fit, educational quality, and future career goals—so your rank order list truly reflects where you will thrive.
Understanding the Residency Match Process and Your Rank List
Before you can rank residency programs wisely, you need a clear understanding of how the Match works and what your rank order list actually does for you.
How the NRMP Match Algorithm Works (In Practical Terms)
The National Resident Matching Program (NRMP) uses a “candidate‑proposing” algorithm. In practice, this means:
- The algorithm tries to place you into your highest-ranked program that also ranks you high enough to fill one of its positions.
- Your rank list should represent your true preferences, from most to least desired, without trying to “game” the system.
- Programs do not see your rank list. They only submit their own list of applicants in order of preference.
- The algorithm favors applicant preference, not program preference, as long as the program has open spots.
Key implication for you:
If you would be happy training there, rank it ahead of programs you prefer less—even if you think it’s a “reach” or you’re worried it’s too competitive. Do not reorder your list based on where you think you’ll match; base it on where you most want to train.
Timeline and Strategy Around Creating Your Rank Order List
- During interview season: Take detailed notes immediately after each interview—impressions, pros/cons, culture, red flags, and how you felt around residents and faculty.
- January–February: Revisit your notes, talk with trusted mentors, and gather additional information about unclear programs.
- Before the NRMP rank list deadline: Finalize your list, verify for accuracy, and submit. You can adjust your list until the official deadline—but once the deadline passes, it is locked.
Your goal is to walk into Match Week knowing that every program on your list is somewhere you could see yourself learning, growing, and living for several years.
Key Educational Factors When Ranking Residency Programs
Residency is, first and foremost, specialized healthcare education. How a program trains you will affect your competence, confidence, and later career options.
1. Training Quality, Curriculum, and Clinical Exposure
The core of any residency program is its curriculum and training environment.
Breadth and Depth of Clinical Experience
Ask yourself:
- Does the program offer broad exposure to the full scope of your specialty?
- Will you see high-volume, high-acuity cases?
- Are there subspecialty rotations (e.g., cardiology, critical care, palliative, sports medicine) that match your interests?
Consider these examples:
- In Internal Medicine, does the program have strong inpatient, outpatient, ICU, and subspecialty experiences?
- In Pediatrics, do you get exposure to NICU, PICU, community pediatrics, and subspecialties like adolescent medicine or pediatric cardiology?
- In Surgery, will you get enough hands-on operative experience early on, or mostly observe senior residents?
Look for programs that document case numbers, board pass rates, and rotation schedules clearly.
Structure of the Curriculum
Programs may use different training models:
- Traditional block rotations (e.g., 4-week inpatient, then 4-week ambulatory, etc.)
- Longitudinal or continuity-based models, integrating outpatient and inpatient responsibilities across the year
- Special tracks:
- Primary care tracks
- Hospitalist tracks
- Research tracks
- Global health tracks
- Physician‑scientist pathways (e.g., ABIM Research Pathway)
Review:
- Sample rotation schedules for each year
- Amount of elective time and flexibility
- Specific required rotations and whether they align with your goals
Programs that share detailed rotation schedules on their websites (or in interview materials) demonstrate transparency about their training structure.
Procedural and Hands-On Opportunities
For procedure-heavy specialties (EM, surgery, anesthesia, OB/GYN) and even fields like internal medicine or pediatrics, hands‑on training is crucial. Ask:
- How are procedures taught and tracked?
- Are simulation labs used regularly?
- Do residents feel they graduate with confidence and competence in required procedures?
If possible, ask current residents if they feel “overtrained,” “appropriately trained,” or “undertrained” in procedures by graduation.
2. Faculty, Teaching Culture, and Mentorship
Your faculty and mentors will strongly influence how you grow during residency.
Faculty Accessibility and Teaching Style
During interviews and second looks, pay attention to:
- Do faculty appear engaged in resident education, or primarily focused on their own clinics/research?
- Are attendings approachable for questions, feedback, and debriefing difficult cases?
- Is there structured teaching (morning report, noon conference, grand rounds) that residents actually attend?
You’ll learn clinical medicine not only from the volume of patients you see, but also from how effectively your attendings teach and model reasoning and professionalism.
Mentorship and Career Development Support
Mentorship is especially important if you:
- Are considering competitive fellowships (e.g., cardiology, GI, derm, ortho)
- Plan to do academic medicine or research
- Are interested in non-traditional paths (policy, global health, med ed, informatics)
Look for:
- Formal mentorship programs pairing you with a faculty advisor
- Access to subspecialty mentors
- Regular career development meetings (e.g., annual individual meetings with program leadership)
- Support for research projects, QI initiatives, or conference presentations
Ask residents:
- Do you feel you have at least one go‑to mentor for career guidance?
- How responsive are faculty to requests for letters of recommendation?
A strong mentorship environment can open doors and make your residency years more purposeful and rewarding.

Program Reputation, Accreditation, and Outcomes
While reputation is not everything, it does matter—particularly for certain career paths.
3. Program Reputation and Institutional Environment
Consider reputation in context rather than chasing prestige blindly.
Institutional Prestige vs. Personal Fit
Programs affiliated with major academic centers or well‑known hospitals may offer:
- Stronger research infrastructure
- More competitive fellowship pipelines
- Greater name recognition when applying for jobs or fellowships
However:
- A less “famous” program with excellent teaching, supportive culture, and strong outcomes might be a better fit—and can still launch a stellar career.
- If you plan a community-based career, a well‑regarded regional or community program might serve you better than a big tertiary center where you’re one of many.
Try to look beyond name recognition to actual outcomes and environment.
ACGME Accreditation and Program Stability
Confirm that the residency is:
- Fully ACGME-accredited
- Free from recent serious citations or chronic issues (some of this can be inferred from word-of-mouth, resident turnover, or abrupt leadership changes)
Red flags to ask about:
- Frequent program director turnover
- Sudden loss of key rotations or training sites
- Significant declines in board pass rates over several years
4. Board Pass Rates, Fellowships, and Job Placement
Your residency should prepare you to pass boards and secure your next step.
Ask or research:
- Board exam pass rates over the last 3–5 years
- The proportion of graduates going into:
- Fellowships (and which ones/where)
- Academic vs. community practice
- Hospitalist or outpatient roles
- Whether residents feel supported in:
- Fellowship applications (mock interviews, letter writing, research)
- Job search (networking, introductions, career advising)
For example, if you’re certain about pursuing cardiology, a program where multiple residents match into competitive cardiology fellowships annually may be a better fit than one with limited fellowship exposure or mentorship.
Resident Life, Workload, and Wellness
No matter how strong the curriculum, you cannot learn well if you’re burned out, unsupported, or unhappy in your environment.
5. Workload, Schedules, and Work-Life Balance
Residency will be demanding everywhere—but programs differ in how they handle resident workload.
Duty Hours and Reality on the Ground
All programs must adhere to ACGME duty hour limits, but actual experiences can vary.
Ask residents:
- Do you consistently work within duty hour rules, or are violations common?
- Are residents expected to “stay after” frequently to complete work?
- How often do you get post‑call days off or adequate rest between stretches of shifts?
Patterns of chronic overwork may indicate systemic problems with staffing or workflow.
Call Schedules and Night Coverage
Clarify:
- How is overnight coverage handled (night float, 24‑hour call, shift work)?
- How many weekends do you work per month on average?
- Are there holiday coverage policies that feel fair?
For shift-based specialties (e.g., EM, anesthesia), ask about:
- Distribution of nights, weekends, and holidays
- How far in advance you get your schedules
- Respect for time off requests
Wellness Resources and Support Systems
Look beyond buzzwords. Concrete wellness elements include:
- Confidential mental health services and counseling
- Peer support groups or Balint groups
- Protected time for resident retreats or wellness days
- Clear policies and a supportive culture around:
- Medical leave
- Parental leave
- Accommodations when needed
Ask residents: If someone is struggling—burnout, depression, personal crisis—how does the program respond?
6. Program Size, Culture, and Resident Cohesion
The social and cultural environment will deeply affect your day‑to‑day satisfaction.
Program Size: Small vs. Large
Smaller programs may offer:
- More individualized attention
- Close relationships with faculty
- A “family” feel and easier schedule flexibility
Larger programs may offer:
- More varied rotations and electives
- More peers at your level (support, coverage, social life)
- Subspecialty and research options that smaller programs can’t match
Reflect on your own preferences: Do you thrive in intimate settings or large, bustling environments?
Culture, Communication, and Psychological Safety
Try to sense:
- Do residents seem genuinely happy and supportive of each other, or exhausted and cynical?
- Is it acceptable to ask questions, admit uncertainty, and learn from mistakes without humiliation?
- Are there resident voices in decision‑making (e.g., resident reps on committees, regular town halls with leadership)?
Red flags may include:
- Residents being reluctant to speak openly in front of faculty or leadership
- Reports of bullying, harassment, or microaggressions without adequate response
- High resident attrition or frequent transfers out of the program
When you leave an interview, ask yourself: Can I picture myself working alongside these residents at 3 AM on a rough call night?
Location, Lifestyle, and Personal Priorities
Residency is also where you will live your life, not just learn medicine. Ignore this at your peril.
7. Geographic Location and Day-to-Day Living
Think about your life outside the hospital:
- Urban vs. suburban vs. rural settings:
- Urban: diverse pathology and population, but often higher cost of living, traffic, housing competition
- Suburban: potentially better housing options and schools, moderate cost, mixed patient populations
- Rural: close-knit communities, broad scope of practice, more independence, but fewer amenities and possibly less anonymity
Consider proximity to:
- Family or support networks
- A partner’s job or training
- Hobbies that keep you grounded (outdoor activities, arts, faith communities, etc.)
8. Cost of Living and Financial Considerations
Resident salaries are relatively similar across programs, but cost of living can vary dramatically.
Assess:
- Average rent for a safe, reasonable apartment
- Transportation costs (car payments, parking, gas, public transit)
- Childcare, if relevant
- Taxes and other recurring expenses
A prestigious program in an extremely expensive city may cause significant financial stress, while a slightly lesser-known program in a more affordable area could give you a healthier quality of life.
Create a simple estimated monthly budget for a few top programs to compare realistically.
How to Research Programs and Organize Your Rank List
Information overload is common. Systematically organizing what you learn will help you see patterns clearly.
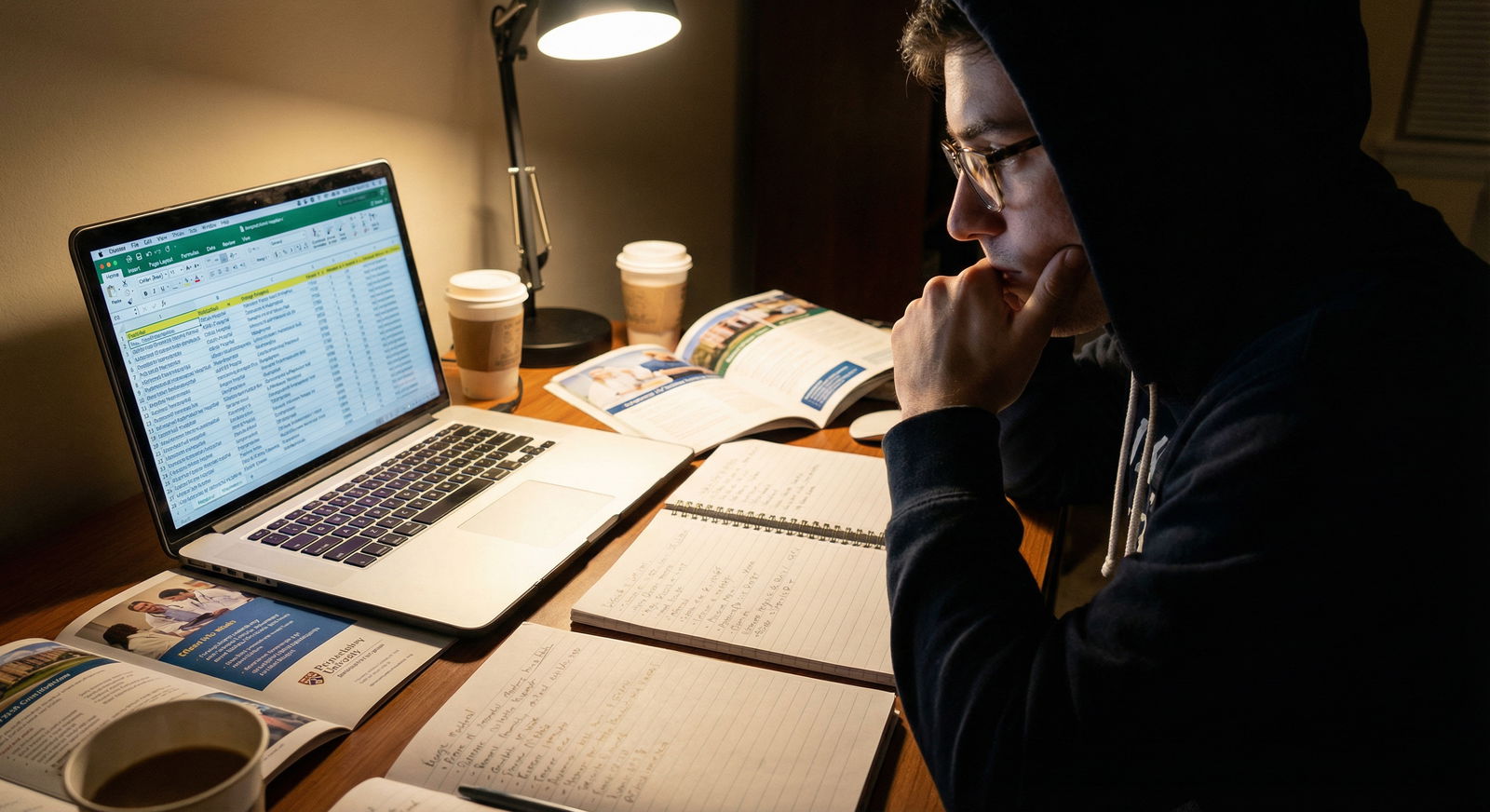
9. Building a Structured Comparison System
A simple spreadsheet can make your final ranking process much more rational and less emotional.
Include columns such as:
- Program name and location
- Type (academic, community, hybrid)
- Curriculum highlights (tracks, electives, fellowships)
- Call schedule & duty hours
- Culture (your impression, resident morale)
- Cost of living
- Career outcomes (fellowships/jobs)
- Personal notes from interview day (gut impressions, red flags)
You can:
- Assign weights or scores to factors you care about most (e.g., training quality, location, lifestyle, fellowship prospects).
- Color‑code programs (green = strong fit, yellow = neutral, red = concerns).
This doesn’t have to be perfectly quantitative, but it helps you avoid making decisions based solely on recency bias or name recognition.
10. Using Trusted Insights: Residents, Alumni, and Mentors
Beyond official websites and brochures, some of your best information comes from people:
- Current residents: Ask candid questions about workload, support, how the program has handled crises (e.g., COVID surges), and whether they would choose the same program again.
- Recent alumni: They can tell you how well the program prepared them for boards, fellowship, or practice.
- Faculty mentors at your medical school: They may know program reputations, leadership, and outcomes that aren’t obvious from the outside.
Be mindful of:
- Individual bias: One person’s negative experience may not reflect the whole picture—but multiple similar stories should be taken seriously.
- Your own identity and needs: Seek input from mentors who understand your background and goals (e.g., as an international medical graduate, nontraditional applicant, or underrepresented in medicine).
Making Your Final Rank List: Strategy and Mindset
After research, reflection, and countless conversations, you eventually must decide how to order your programs in the NRMP system.
11. Aligning Programs With Your Values and Goals
Clarify your top priorities before finalizing your list. Common priority categories include:
- Training quality and clinical rigor
- Location and lifestyle
- Fellowship or academic career potential
- Program culture and wellness
- Proximity to family or partner
Some strategies:
- Write out your top 3–5 non-negotiables (e.g., “strong ICU training,” “supportive culture,” “within driving distance of partner”).
- For each program, briefly note how it meets or fails each non‑negotiable.
- Pay attention to whether certain programs consistently come to mind when you imagine starting residency.
12. Trusting Your Gut—Within a Structured Framework
Intuition is not unscientific—it’s your synthesis of many data points and experiences. Once you’ve done your homework:
- If you keep picturing yourself at a particular program and your rational analysis also supports it, that program likely belongs high on your list.
- If a program “looked good on paper” but you felt uneasy on interview day (disorganized, dismissive faculty, unhappy residents), don’t ignore that signal.
Rank programs in the exact order you would prefer to attend them, from #1 (dream) to #N (still acceptable). Do not:
- Rank a program you would not be willing to attend under any circumstances. If you match there, you are contractually obligated to go.
- Change your list to “game” perceived competitiveness. The algorithm is designed so that you maximize your chances by being honest.
Once you submit your list, take the time to acknowledge the thought and work you invested. You’ve made a reasoned, informed decision with the information you had at the time.
Frequently Asked Questions About Ranking Residency Programs
Q1: What is the NRMP, and how does it affect how I should rank programs?
The National Resident Matching Program (NRMP) is the organization that oversees the Match Process for residency and many fellowship programs in the United States. It uses an algorithm that starts with your top-ranked program and attempts to place you there, moving down your list only if necessary.
Implications for your ranking strategy:
- Always rank programs in your true order of preference.
- Don’t lower a program on your list because you think it’s “too competitive” or unlikely—if you do that, you’re only hurting your own chances of going there.
- Programs do not see your rank list, so you cannot offend a program by ranking them lower.
Q2: Should I prioritize program reputation or location when ranking residency programs?
It depends on your goals:
- If you aim for highly competitive fellowships or academic medicine, a program with strong research infrastructure, fellowship pipelines, and national reputation can be helpful—but it is not the only path to success.
- If personal support systems, partner jobs, cost of living, or family responsibilities are critical, location may justifiably take priority.
- Often, the best choice balances solid training and outcomes with a location where you can realistically be well and functional.
When in doubt, ask: Where am I most likely to become the physician I want to be—and stay healthy while doing it?
Q3: How can I realistically evaluate work-life balance at a program?
Use multiple sources:
- Ask residents specific questions about:
- Average hours per week on different rotations
- Night/weekend frequency
- How often duty hours are violated in practice
- How approachable leadership is when residents feel overwhelmed
- Look for concrete wellness initiatives:
- Access to mental health care
- Retreats, wellness days, resident support groups
- Reasonable parental leave and medical leave policies
- Pay attention to residents’ energy and tone on interview day. Do they seem exhausted and disengaged, or tired but still supported and engaged in learning?
No program will be easy, but there is a difference between challenging but supportive and chronically unsustainable.
Q4: How important are mentorship and research when ranking programs?
Mentorship and research matter most if:
- You want a fellowship, particularly in a competitive subspecialty
- You’re interested in academic medicine, medical education, or clinician‑scientist roles
- You’re drawn to quality improvement, health policy, or global health
Even if you’re unsure of your future path, a program with:
- Accessible mentors
- Opportunities for scholarly work (research, QI, education projects)
- Support for conference presentations
…gives you more flexibility later. That said, if your primary goal is to be an excellent community clinician, you may prioritize programs with strong clinical training and supportive culture over research intensity.
Q5: Can I change my rank order list after I submit it? What if I change my mind?
You can edit and resubmit your rank order list as many times as you like up until the NRMP deadline. After the deadline:
- Your list is locked, and you cannot change it.
- The NRMP uses the last certified version of your list submitted before the deadline.
If you’re uncertain as the deadline approaches:
- Review your priorities and notes one more time.
- Discuss with a trusted mentor who knows you and your goals.
- Once the deadline passes, allow yourself to move forward—ruminating won’t change the outcome, but can increase anxiety.
By thoughtfully evaluating training quality, mentorship, reputation, work‑life balance, location, and program culture—and organizing your observations systematically—you can create a rank list that truly supports your long‑term goals in healthcare education and career development. Ranking residency programs is less about finding the “perfect” choice and more about finding the right environment for you to grow into the physician you want to become.




















