
Introduction: Why Your Residency Ranking Strategy Matters
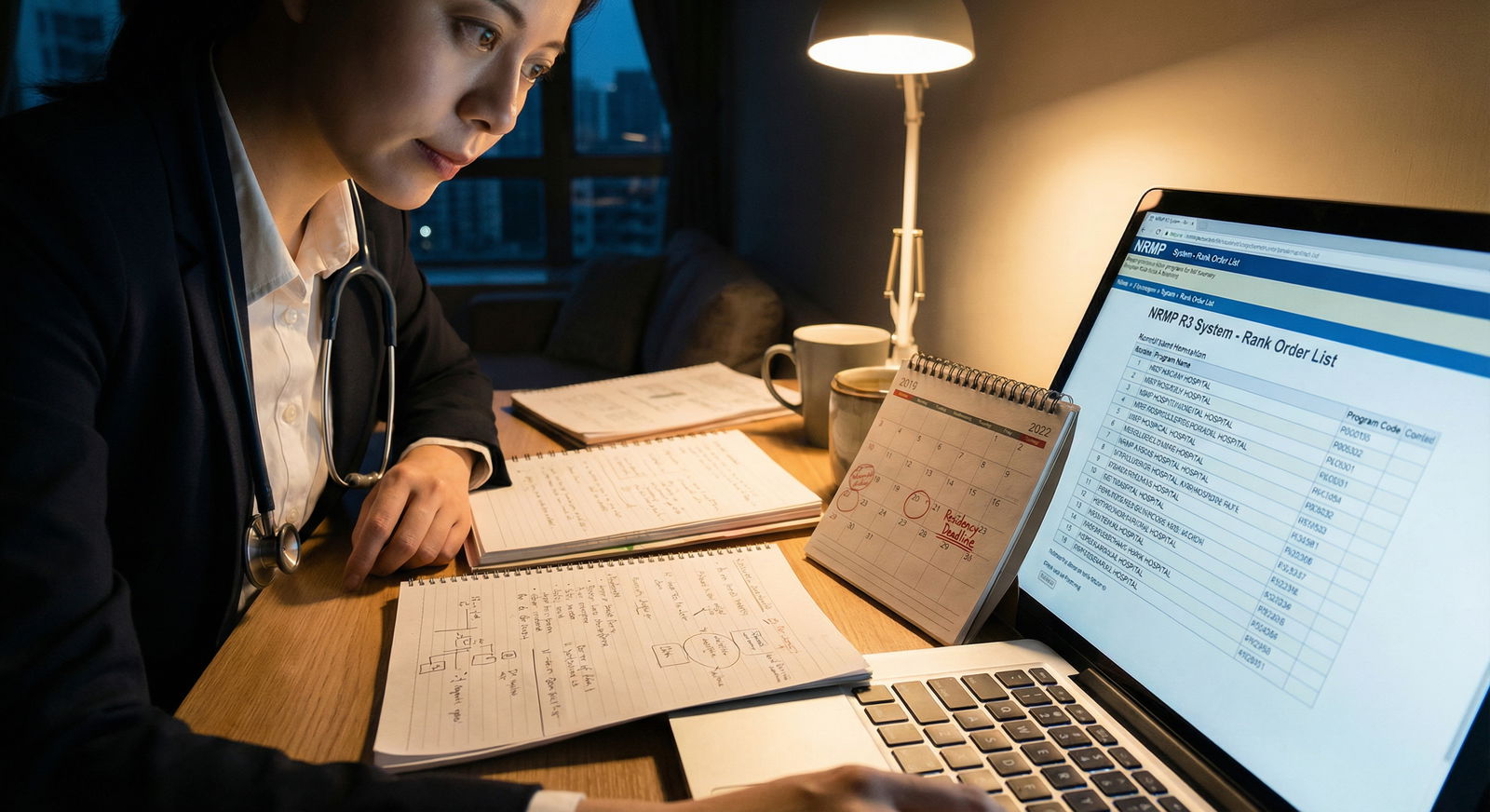
The transition from medical school to residency is one of the most defining turning points in your medical education. Years of exams, clerkships, and sub-internships lead to a single, high‑stakes outcome: your NRMP Match result. While you cannot control everything, you can control how thoughtfully you approach the residency ranking process.
A strong Residency Ranking Strategy is not simply about putting big‑name programs at the top of your list. It is about aligning your values, learning style, and long‑term Career Development goals with programs that will support your growth. Done well, your rank list becomes a powerful tool to maximize your chances of matching into a residency where you will thrive—not just survive.
This guide walks through a comprehensive, step‑by‑step approach to navigating the Residency Process and NRMP Match, from early preparation through final submission of your Rank Order List (ROL).
Understanding the Residency Application and Match Timeline
Before zooming in on ranking, it helps to see where it fits in the broader Residency Process. Viewing ranking in context will keep you organized and reduce last‑minute stress.
Key Phases of the Residency Process
Early Preparation (MS2–early MS3)
- Explore specialties through shadowing, elective rotations, and interest groups.
- Start reflecting on what kind of physician you want to become and what environments bring out your best.
- Begin informal research on programs and regions that appeal to you.
Application Development (MS3–early MS4)
- Prepare your ERAS application: CV, personal statement, and activity descriptions.
- Request letters of recommendation (LORs) early from faculty who know you well.
- Take and, if needed, retake USMLE/COMLEX exams according to your specialty’s expectations.
Application Submission (Early Fall)
- Submit ERAS applications strategically—balancing reach, target, and safety programs.
- Tailor personal statements or supplemental material where appropriate.
- Track specialty‑specific and program‑specific requirements.
Interview Season (Late Fall–Winter)
- Attend interviews (in‑person or virtual) with programs that invite you.
- Evaluate program culture, resident happiness, faculty engagement, and educational structure.
- Keep organized notes after each interview to inform your future rank list.
Ranking and the NRMP Match (Late Winter)
- Create and certify your NRMP Rank Order List.
- Programs also submit their ranking of applicants.
- The NRMP algorithm uses both sets of preferences to determine Match outcomes.
Match Week and Transition to Residency (Spring)
- Receive your Match result.
- If you do not match, participate in SOAP and reassess your strategy.
- Prepare for relocation, licensure, and the start of residency.
Understanding this timeline reinforces an important point: your Residency Ranking Strategy starts long before you log into NRMP. Every rotation, mentorship conversation, and interview feeds into the decisions you make later.
The NRMP Match: How the Algorithm Uses Your Rank List
What Is the NRMP and Why Does It Matter?
The National Resident Matching Program (NRMP) is the central organization that coordinates most U.S. residency placements. It uses a computerized, applicant‑favorable algorithm to match applicants and programs based on their submitted rank lists.
This is critical: the algorithm is intentionally designed to prioritize applicant preferences. Understanding this helps you avoid common ranking mistakes driven by anxiety rather than logic.
How Ranking Works in the NRMP Match
At the end of interview season:
- You submit a Rank Order List of the programs where you interviewed, in true order of preference.
- Programs submit Rank Order Lists of applicants they are willing to train.
The NRMP algorithm then:
- Starts with an applicant’s first‑choice program.
- Tries to place the applicant there if:
- The program ranked the applicant, and
- The program has a position available or prefers the applicant over someone already tentatively placed.
- If placement isn’t possible, the algorithm moves to the applicant’s second choice, and so on.
Because applicants are considered for their highest‑ranked choices first, you should always rank programs in your genuine order of preference, regardless of how competitive you think they are. Trying to “game” the algorithm almost never helps and often hurts your chances of getting the best possible match for you.

Building a Thoughtful Residency Ranking Strategy
A strong Residency Ranking Strategy is systematic. Instead of relying on vague impressions, you will move through structured steps: self‑assessment, research, engagement, reflection, and finally building your Rank Order List.
Step 1: Deep Self‑Assessment – Clarifying What You Actually Want
Before you judge programs, clarify your own needs and priorities. Without this, it’s easy to be swayed by name recognition, peer pressure, or interview‑day charm.
Consider reflecting in a journal or spreadsheet on questions like:
A. Specialty and Career Goals
- Which specialties truly energized you during rotations, and why?
- Do you envision a career in:
- Academic medicine (teaching, research, leadership)?
- Community practice or private practice?
- Subspecialty fellowship (e.g., cardiology, GI, critical care)?
- Underserved or rural care?
Your career direction affects what you need from a residency—for instance, strong research support may be crucial if you aspire to competitive fellowships or academic positions.
B. Educational Environment and Learning Style
- Do you thrive with:
- High‑volume, high‑acuity experiences?
- Smaller, more intimate programs with close faculty contact?
- Structured didactics vs. more self‑directed learning?
- Do you value:
- Early autonomy, or more gradual responsibility?
- Strong simulation resources and procedural training?
C. Location and Lifestyle
- Geographic preferences:
- Do you need to be near family or a partner?
- Urban vs. suburban vs. rural settings?
- Cost of living and commuting time?
- Lifestyle considerations:
- Access to childcare, schools, public transportation.
- Climate and outdoor/recreational opportunities.
- Social support networks (friends, communities, religious groups).
D. Culture and Wellness
- Are diversity, equity, and inclusion priorities for you?
- How important is formal wellness programming, mental health support, and reasonable scheduling?
- How much do you value resident camaraderie and faculty approachability?
Organize your self‑assessment into “non‑negotiables,” “strong preferences,” and “nice‑to‑haves.” This framework will guide every step that follows.
Step 2: Researching Residency Programs Strategically
Once you’re clear on what you want, evaluate programs through multiple lenses beyond their websites.
A. Program Websites and Official Materials
On each program’s website, look for:
- Curriculum structure: Rotations, electives, continuity clinics, ICU time.
- Patient population and clinical sites: Community vs. tertiary center; VA hospitals; children’s hospitals.
- Faculty and leadership: Stability of program leadership, core faculty interests.
- Research infrastructure: Protected time, mentorship, ongoing projects, track records for fellowships.
- Call schedules and duty hours: Night float vs. traditional call; weekend frequency.
- Resident outcomes:
- Fellowship match lists.
- Job placement locations.
- Chief resident selections.
Cross‑check with the ACGME and FREIDA databases for objective data (program size, accreditation status, etc.).
B. Unofficial Resident Feedback and Online Communities
While you should interpret anonymous comments cautiously, resident‑driven platforms can provide valuable insight:
- Reddit (e.g., r/medicalschool, r/Residency)
- Student Doctor Network
- Specialty‑specific forums or Discord groups
Look for patterns rather than single comments:
- Are there recurring concerns about toxic culture, scut work, or chronic understaffing?
- Do multiple people highlight strong teaching, flexible leadership, or happy residents?
C. Leveraging Your Network
Your network is one of the most underused tools in the Residency Process:
- Faculty mentors: Ask for honest opinions about programs’ reputations, training quality, and fellowship outcomes.
- Recent alumni: Talk with graduates of your medical school who matched into your specialty. Ask:
- What do you wish you knew about your program before ranking?
- How supportive has your program been in pursuing fellowships or research?
- Residents you met on rotations: Reach out for informal chats about day‑to‑day life and program culture.
Always remember: one person’s experience is just one data point—but enough data points can reveal trends.
Step 3: Attending Open Houses, Second Looks, and Meeting Residents
Programs increasingly offer virtual open houses, meet‑and‑greet events, and second looks. These events, along with your interview day, are some of the best opportunities to evaluate fit.
How to Maximize These Interactions
Prepare focused questions tailored to your priorities:
- “How is feedback delivered to residents?”
- “What changes has leadership made in response to resident feedback in the last 2–3 years?”
- “Can you describe how the program supports resident wellness and mental health?”
- “How are struggling residents supported academically and personally?”
Observe interactions and body language:
- Do residents seem comfortable speaking honestly in front of leadership?
- Do they appear exhausted, disengaged, or genuinely collegial and proud of their program?
- How do faculty address residents—respectfully, dismissively, humorously?
Take structured notes afterward:
- Rate programs on domains like teaching, culture, location, wellness, and career support.
- Capture specific examples (e.g., “PD gave clear example of adjusting night float after resident feedback”).
Over time, your notes will provide a much more reliable foundation than vague memories.
Step 4: Reflecting on Interview Experiences in Real Time
Interview season can blur quickly—especially when you have 10–20 interviews over several weeks. Intentional reflection right after each interview is critical for an effective Residency Ranking Strategy.
Create a Standardized Post‑Interview Template
After each interview, immediately jot down your impressions. For each program, consider rating or describing:
- Overall program fit: Did you feel like you belonged?
- Resident satisfaction: Did residents seem supportive and engaged, or burned out and cynical?
- Faculty engagement: Did interviewers seem genuinely interested in you, or distracted and rushed?
- Educational quality: How robust did morning reports, conferences, and bedside teaching seem?
- Support for your specific goals:
- Fellowship placement for your desired field.
- Research alignment with your interests.
- Opportunities for teaching or global health.
You might create a simple 1–5 score for each domain and an overall “gut feeling” score. Remember: your subjective experience matters. You are selecting not just a training site—but a community for the next 3–7 years of your life.
Step 5: Constructing and Refining Your Rank Order List
Once interviews wind down, it’s time to translate all your information into a structured, thoughtful Rank Order List.
A. Start with a Draft List
- List all programs where you interviewed.
- Sort them roughly by your current preference.
- Don’t overthink at the start—this is a first pass based on your notes and impressions.
B. Group Programs into Tiers
Many applicants find it helpful to group programs before fine‑tuning:
- Tier 1 – Ideal Fit Programs
- You loved the culture and training.
- They match your career goals and location preferences.
- Tier 2 – Strong Options
- Good training, acceptable location.
- Some minor trade‑offs but overall positive.
- Tier 3 – Acceptable/Backup Programs
- You could see yourself training there but with significant compromises (e.g., location, volume, culture).
- Tier 4 – Programs You Would Not Want to Attend
- If you would be unhappy training there, do not rank them.
If you match to a program you’re sure you don’t want, withdrawing it from your list beforehand is your only way to avoid that outcome.
- If you would be unhappy training there, do not rank them.
C. Check for Bias and Pressure
Ask yourself:
- Am I overvaluing prestige at the expense of wellness, fit, or family needs?
- Am I letting peers’ preferences dictate my choices?
- Am I under‑ranking a program I loved because I think it’s “too competitive”?
Remind yourself: the NRMP algorithm favors applicants. You do not improve your chances by ranking a “backup” before a “reach.” You only reduce your chance of getting the reach program you truly prefer.
D. Seek Feedback from Trusted Mentors
Share your preliminary rank list with:
- A specialty mentor or advising dean.
- A resident in your chosen field.
- A trusted peer who knows your priorities well.
Ask specific questions:
- “Given my goals in [fellowship X or practice Y], does this order make sense?”
- “Are there any programs here whose reputation for training is substantially stronger or weaker than I realized?”
Be open to feedback, but remember: final decisions should align with your values, not someone else’s agenda.
E. Finalize and Certify Your Rank Order List
Before the NRMP deadline:
- Double‑check that:
- Your list reflects your true preferences.
- No program appears on your list that you would be unwilling to attend.
- You have considered dual‑career or couples’ matching needs if applicable.
- Log in early—do not wait until the final hours in case of technical issues.
- Remember: you can revise your list and re‑certify until the official deadline; only the last certified version counts.
Once you’ve certified, step back. Obsessively re‑editing in the final hours rarely improves your outcome and often increases anxiety.
Common Pitfalls in the Residency Ranking Process—and How to Avoid Them
Even strong applicants fall into predictable traps. Being aware of them can help you make clearer, more confident decisions.
Overvaluing Reputation Alone
- Choosing a program solely because it is highly ranked or famous can backfire if the culture is unsupportive or the location is wrong for you.
- Balance prestige with training quality, mentorship, and well‑being.
Ignoring Personal Well‑Being
- Residency is demanding. Programs with chronic understaffing, excessive call, or poor support can lead to burnout.
- Ask about:
- Access to mental health services.
- Policies for sick leave and parental leave.
- Evidence of real responses to wellness concerns.
Trying to “Game” the NRMP Algorithm
- Ranking “safer” programs first because you’re afraid of not matching at your dream program goes against how the algorithm works.
- Rank in true preference order. The applicant‑favorable design means this gives you the best shot at what you want.
Rushing the Decision at the Last Minute
- Waiting until the night before the deadline leads to anxiety‑driven decisions.
- Start building and revisiting your list at least 2–3 weeks before it is due.
Ignoring Honest Red Flags
- If multiple residents privately express dissatisfaction, or you witnessed disrespectful behavior, take it seriously.
- No program is perfect, but chronic systemic issues should not be ignored.
Under‑Ranking Programs with Strong Career Support
- Look beyond call rooms and city appeal. Programs that advocate for you, provide strong letters, and place graduates into fellowships or jobs effectively have long‑term impact on your Career Development.
Frequently Asked Questions About the Residency Ranking Process
1. What factors should I prioritize when ranking residency programs?
Focus on a blend of personal and professional considerations:
- Training quality: Case volume, complexity, supervision, and educational structure.
- Program culture: Resident camaraderie, leadership responsiveness, respect for trainees.
- Career alignment: Fellowship match record, research support, mentorship in your area of interest.
- Location and lifestyle: Cost of living, support systems, commute, family/partner needs.
- Wellness and support: Schedule fairness, mental health resources, call burden, leave policies.
Create your own rubric and score programs across these domains, then let your overall sense of fit guide your final order.
2. How many programs should I rank to maximize my chances of matching?
There is no single “correct” number, but data from NRMP shows:
- Generally, more is safer—provided you would actually attend those programs.
- For competitive specialties, ranking a larger number of programs (often 10–15+ or more) improves match rates.
- For less competitive specialties or strong applicants, fewer programs may be sufficient—but it’s still wise to rank all programs where you would realistically train.
Never rank a program you would be unwilling to attend. It’s better to go unmatched than to spend years in a setting that profoundly harms your well‑being or career goals.
3. Should I rank well‑known or prestigious programs higher, even if I felt lukewarm about them?
Not automatically. Consider:
- If a prestigious program truly aligns with your goals (e.g., academic career, high‑impact research), it may be worth a higher rank.
- If you felt a poor cultural fit, lacked support, or disliked the location, think carefully before placing it ahead of a less famous but better‑fit program.
Prestige can open doors, but fit and daily life matter deeply over the years of residency. A moderately known program where you thrive often positions you better than a famous one where you struggle.
4. How can I tell if a residency program genuinely supports resident well‑being?
Look for concrete evidence rather than slogans:
- Track record of change: Examples of leadership making schedule or systems changes based on resident feedback.
- Transparency: Honest discussions about challenges (e.g., patient volume, staffing) plus clear plans to address them.
- Resident behavior: On interview day, do residents appear approachable, collegial, and willing to answer candidly?
- Policies: Access to mental health services, limits on duty hours, parental leave and sick leave policies.
Ask residents privately: “Do you feel heard when you bring concerns to leadership?” Their response is often more telling than anything on a brochure.
5. If I’m couples matching, how should that change my Residency Ranking Strategy?
Couples matching adds complexity but is very doable with planning:
- Discuss priorities early: Decide what matters most—same city, same institution, or similar region.
- Apply broadly and strategically: Target cities with multiple programs in both specialties.
- Use the couples function correctly: Create paired rank lists that reflect combined preferences (e.g., Program A + Program B in City 1 as a top choice).
- Seek guidance: Talk with advisors who have supported previous couples matches in your specialties.
You may need to accept more compromise (e.g., a slightly less ideal program for one partner) to optimize the overall outcome for both.
Thoughtful preparation, honest self‑assessment, and a disciplined approach to evaluating programs will transform the Residency Ranking Process from overwhelming to manageable. By grounding your Rank Order List in your values, learning needs, and long‑term Career Development goals, you give the NRMP algorithm the best possible information to place you where you can become the physician you aspire to be.




















