
The popular narrative about burnout by specialty is wrong in all the ways that matter.
People argue endlessly about whether surgery, emergency medicine, or family medicine is “the worst.” The data tell a more uncomfortable story: nearly every major specialty is losing a disturbing percentage of its workforce to burnout, and the ranking changes once you stop looking at vibes and start looking at numbers, trends, and risk factors.
Let’s walk through what the data actually show.
1. What the Numbers Say: Burnout by Specialty
The most cited quantitative source on physician burnout is the annual Medscape National Physician Burnout & Depression Report, backed up by other surveys (Mayo Clinic, AMA, ACP). Results vary year to year, but the same pattern keeps repeating: certain fields cluster at the top, others at the bottom, and a surprisingly narrow gap separates “worst” from “average.”
To ground this, I will use recent Medscape survey figures (rounded, and aggregated over the last few years to smooth single‑year noise). These are approximate but directionally accurate.

| Category | Value |
|---|---|
| Emergency Med | 60 |
| Internal Med | 55 |
| Ob/Gyn | 55 |
| Family Med | 52 |
| Pediatrics | 48 |
| Anesthesiology | 46 |
| Psychiatry | 45 |
| Radiology | 40 |
| Dermatology | 35 |
| Pathology | 34 |
At a glance:
- Emergency Medicine: around 55–60%
- Internal Medicine: around 50–55%
- Obstetrics/Gynecology: around 50–55%
- Family Medicine: around 50–52%
- Pediatrics: around 45–50%
- Anesthesiology, Psychiatry: mid‑40s
- Radiology: around 40%
- Dermatology, Pathology: low‑ to mid‑30s
So the simplistic claim “derm has no burnout” is false. A one‑third burnout rate would be a crisis in any other industry.
But you and I both know you want the ranking. Here is a simplified snapshot.
| Specialty Cluster | Burnout Rate (Approx.) |
|---|---|
| Emergency Medicine | 58–60% |
| Internal Med / ObGyn | 52–56% |
| Family Med / Hospitalist | 50–53% |
| Pediatrics / Critical Care | 45–50% |
| Anesthesia / Psych / Surgery | 42–48% |
| Radiology / Neurology | 38–42% |
| Dermatology / Pathology | 30–36% |
The gap from “highest” to “lowest” is roughly 25 percentage points. That is not the difference between heaven and hell; that is the difference between “coin flip you burn out” and “one‑in‑three chance you burn out.”
The real question is not “which specialty is safe?” but “which risk profile are you willing to manage?”
2. Why Some Specialties Burn Out More: The Risk Equation
Burnout is not random. The data repeatedly highlight a small set of structural drivers:
- Workload and hours
- Control/autonomy
- Admin burden and EHR overhead
- Emotional intensity and exposure to trauma
- Perceived fairness and respect
- Misalignment between values and daily work
Different specialties combine those variables in different ratios. Think of it as a risk score.
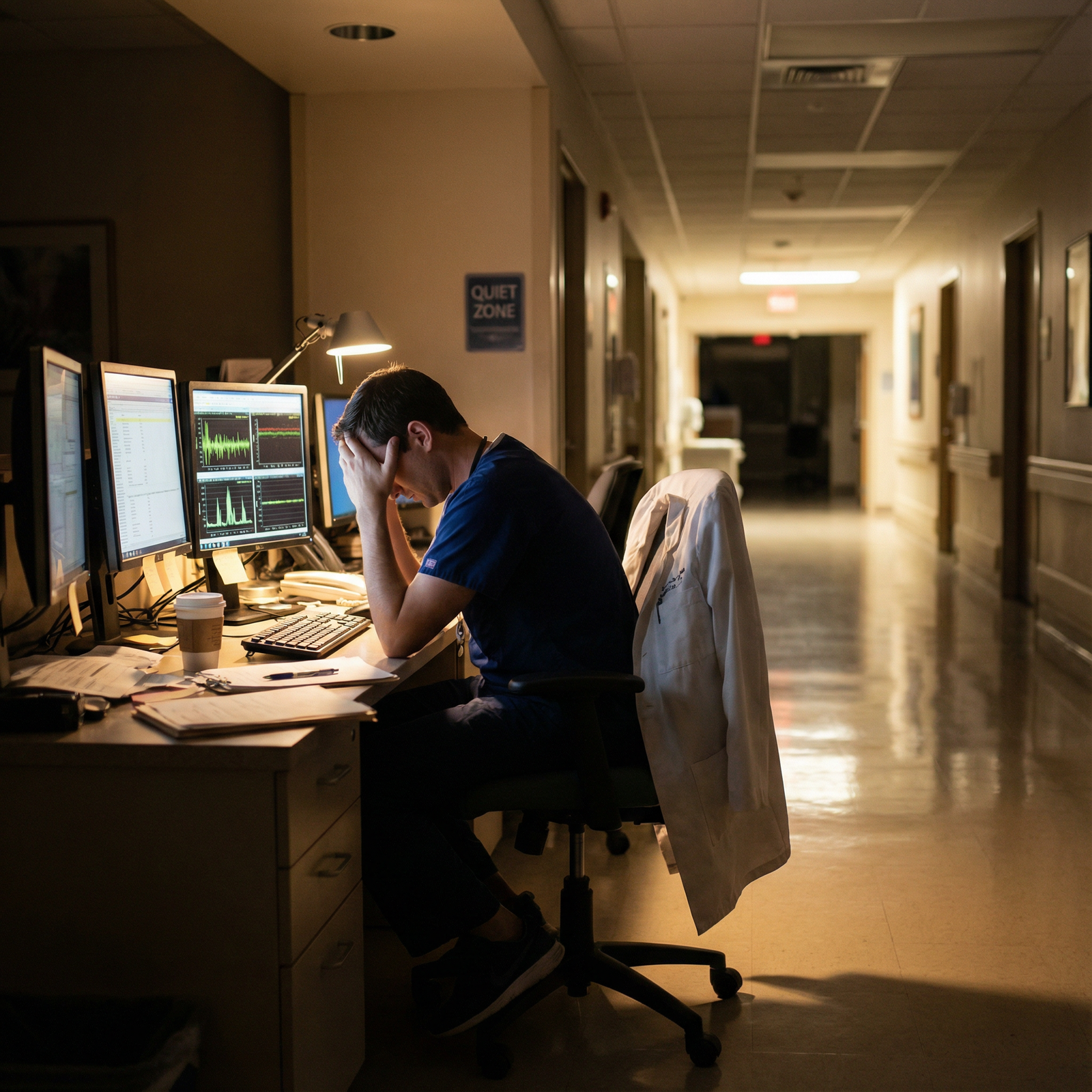
Emergency Medicine: High Volume, Low Control
Emergency medicine almost always tops the burnout charts. The data line up with what ED corridors look like at 3 a.m.
Key factors:
- Schedule: nights, weekends, holidays. High circadian disruption.
- Unpredictable volume: surges, boarding, hallway beds.
- Low control: You cannot pace your day or pick your patients.
- High acuity and trauma: resuscitations, codes, violence, drug use.
- Constant interruptions: alarms, consults, rapid decisions.
Quantitatively, EM physicians report some of the highest rates of:
- Feeling “lack of control” over workload
- Emotional exhaustion scores on Maslach Burnout Inventory
- Intention to reduce clinical hours or leave the field
In multiple survey waves, around 1 in 4 emergency physicians reported serious thoughts of leaving their job within 2 years. That is a pipeline problem, not a lifestyle inconvenience.
Internal Medicine & Family Medicine: Death by a Thousand Clicks
Internal medicine, primary care, and hospitalist roles sit just below EM, but their pattern is different. Less trauma, more grind.
Drivers:
- Large patient panels with chronic, complex disease.
- High documentation and quality metric burden.
- Prior authorizations, refill management, portal messages.
- Lower perceived institutional support vs procedural subspecialties.
The data routinely show that primary care physicians report:
- High “time spent on EHR after hours” (1–2 hours per day is common).
- High rates of feeling that “too many bureaucratic tasks” are the top burnout driver (often >60% citing this).
I have seen outpatient internists finish clinic at 5:30 p.m., then sit in their office until 8:00 p.m. signing notes and reviewing lab results. That after‑hours work rarely shows up on the official “FTE” or RVU count, but it shows up in burnout scores.
OB/Gyn: High Stakes at 3 a.m.
Obstetrics and gynecology persistently land high on burnout lists.
The risk blend:
- Unpredictable hours due to labor and deliveries.
- High malpractice pressure.
- Emotional highs and lows: healthy births vs fetal demise, hemorrhage, maternal complications.
- Frequent night call and in‑house coverage.
From survey data, OB/Gyn physicians commonly report:
- High emotional exhaustion.
- High depersonalization (the “treating patients like objects” dimension).
- Low work‑life balance satisfaction relative to many non‑procedural fields.
When you are managing a shoulder dystocia at 2 a.m. for the third night this week, the theoretical joy of bringing life into the world does not fully insulate you.
Pediatrics: Lower Pay, High Emotional Load
Pediatrics usually lands in the middle range (~45–50% burnout). That does not mean it is safe.
Risk elements:
- High emotional exposure: sick children, chronic disease, non‑accidental trauma.
- Lower compensation relative to workload, which feeds into perceived unfairness.
- Intensive family dynamics and conflict.
In the data, pediatricians often rate “lack of respect from patients/parents” and “too many bureaucratic tasks” as key drivers. Add to that the moral injury of seeing kids who are sick because of social determinants (poverty, housing, food insecurity), and the score goes up.
“Lifestyle” Fields: Not a Free Pass
Dermatology, pathology, radiology frequently sit at the lower end of burnout prevalence. But “lower” still means a third to two‑fifths of physicians are burned out.
Why not zero?
- Radiology: production pressure, RVU volume targets, teleradiology commoditization, isolation from team.
- Pathology: being invisible to patients and leadership, high stakes in cancer diagnoses, staffing shortages.
- Dermatology: business pressures in private practice, cosmetic vs medical mix, insurance complexity.
The data clearly show that good hours plus high pay reduce burnout risk. They do not eliminate it. Burnout is about control, meaning, and fairness at least as much as raw time.
3. Beyond the “Which Specialty” Question: Hidden Risk Modifiers
If you only look at specialty, you miss half the variance. Several variables substantially shift burnout risk within the same field.

| Category | Value |
|---|---|
| Workload/Hours | 30 |
| EHR/Admin Burden | 25 |
| Lack of Control | 20 |
| Work-Home Conflict | 15 |
| Organizational Culture | 10 |
Think of those percentages as rough contributions to the overall “burnout risk budget.”
Practice Setting: Academic vs Community vs Employed vs Private
Surveys consistently report higher burnout among:
- Employed physicians in large systems compared with small independent groups.
- Physicians in high‑volume, productivity‑driven settings vs those with more academic or salaried models.
Academic medicine is not a paradise, but the combination of teaching, research, and more flexible job crafting can buffer burnout. In contrast, a high‑RVU outpatient mill will push burnout up in almost any specialty.
Schedule Structure: Nights, Call, Control
Shift work with nights and weekends (EM, hospitalist, ICU) raises risk, but the degree of schedule control matters.
Example I have seen play out:
- Group A EM: predictive schedules, 8‑hour shifts, protected recovery days, stable team.
- Group B EM: variable shift lengths, self‑scheduling “hunger games,” frequent last‑minute changes.
Same specialty. Burnout rates very different.
Surveys show physicians rating “lack of control over schedule” as one of the strongest predictors of burnout, independent of specialty.
Stage of Career: Training vs Attending
Residents and fellows often show equal or higher burnout rates than attendings. Particularly in:
- Surgery
- IM and subspecialties
- EM
The combination of long hours, limited autonomy, and exam pressure inflates risk. Specialty burnout numbers you see in national reports are mostly attendings; residency can be significantly worse.
Gender, Parenting, and Role Strain
Female physicians, especially those with young children, consistently report higher burnout. Across specialties.
Data highlights:
- Higher rates of work‑home conflict.
- More time spent on non‑RVU tasks (teaching, mentoring, committee work).
- More patient‑requested visits that are not always recognized in compensation.
This effect is not static. Within high‑burnout specialties like EM, OB/Gyn, and IM, the female subgroup can have burnout rates 5–10 percentage points higher than male peers.
4. Work–Life Balance by Specialty: What the Data Actually Show
Burnout is one outcome. Work–life balance is its close cousin, and physicians self‑report these slightly differently. Some high‑burnout fields still report decent satisfaction with life outside medicine, usually because of income and scheduling flexibility.
Here is a simplified comparison of approximate self‑reported satisfaction with work–life balance (again, aggregated across recent survey years, directional not exact).

| Category | Value |
|---|---|
| Dermatology | 80 |
| Radiology | 75 |
| Psychiatry | 70 |
| Anesthesiology | 68 |
| Pediatrics | 60 |
| Family Med | 55 |
| Internal Med | 50 |
| Ob/Gyn | 48 |
| General Surgery | 45 |
| Emergency Med | 40 |
Read this like an index (% satisfied or very satisfied):
- Dermatology: ~80%
- Radiology: ~75%
- Psychiatry: ~70%
- Anesthesia: high 60s
- Pediatrics: around 60%
- Family medicine: mid‑50s
- Internal medicine: about 50%
- OB/Gyn, surgery, EM: often below 50%
Now notice something important: Even in dermatology, about 1 in 5 are not satisfied with their work–life balance. That is not trivial.
Again, the question is not “Which specialty makes burnout impossible?” There is no such field. It is “Which combination of hours, emotional load, and compensation gives you a tolerable risk profile?”
5. Specialty Profiles: Where Burnout Really Bites
Let me give you a more practical, data‑driven summary of which fields truly struggle the most, and why.
| Specialty | Burnout Level | Main Drivers |
|---|---|---|
| Emergency Med | Very High | Shifts, volume, low control, trauma |
| Internal Med | High | Admin/EHR, complexity, volume |
| Ob/Gyn | High | Call, liability, high stakes nights |
| Family Med | High | Panel size, admin, reimbursement |
| Pediatrics | Moderate-High | Emotions, admin, lower pay |
| Surgery | Moderate | Hours, hierarchy, call |
| Psychiatry | Moderate | Emotional load, access pressures |
| Anesthesiology | Moderate | OR pressures, vigilance fatigue |
| Radiology | Lower-Mod | RVU pressure, isolation |
| Dermatology | Lower | Business pressure, expectations |
If you force me to rank “who truly struggles the most” from a burnout and work–life strain perspective, based on the weight of recent data:
- Emergency Medicine
- Internal Medicine (including hospitalists)
- Obstetrics/Gynecology
- Family Medicine
- Pediatrics / Critical Care
After that, you get more heterogeneous patterns: individuals doing fine or badly based on local culture, practice type, and personal boundaries.
6. How to Use This Data for Your Own Career Decisions
You are not a regression coefficient. You are one data point with your own risk modifiers and preferences.
Here is the practical way to use these numbers.
Step 1: Identify Your Tolerance Profile
Be honest about:
- Circadian tolerance: Nights and shifts wreck some people, others adjust.
- Emotional bandwidth: Trauma, death, and chronic suffering hit people differently.
- Bureaucratic tolerance: Some can grind through EHR and prior auths; some cannot.
- Need for control: Can you handle unpredictability, or do you need routine?
I have seen students who swore they loved the ED flame out after 4 years of night shifts. And quiet introverts who thrived in pathology after realizing they hated emotional confrontation.
Step 2: Map Yourself Against the Data
If you hate:
- Nights
- Unpredictability
- Violence or trauma
You are stacking risk by choosing EM, ICU, or certain surgical paths. Not guaranteed burnout, but you are swimming upstream.
If you hate:
- Long‑term follow‑up
- Chronic disease management
- Paperwork and portals
Then primary care internal medicine or outpatient family medicine will likely grind you down, unless you are in a particularly well‑designed practice.
On the flip side:
- If you crave procedures, clear end‑points, and less longitudinal attachment, anesthesia or some surgical subspecialties may distribute your emotional load more sustainably.
- If you value control over schedule and high income per hour, procedural outpatient fields (GI, cards, dermatology, some radiology models) statistically look better.
Step 3: Look at Environment, Not Only Specialty
I cannot emphasize this enough: there is more variation between good and bad jobs inside a single specialty than between two specialties on paper.
Same specialty, two realities:
- Hospitalist Group X: capped census, strong APP support, smart night coverage model, collegial consultants. Burnout moderate.
- Hospitalist Group Y: uncapped census, frequent cross‑cover, minimal staffing, adversarial admin. Burnout off the charts.
The national burnout data tell you baseline risk. Your job search and boundary setting determine the actual outcome.
7. Ethical Dimension: Burnout Is Not Just a Personal Problem
The category you specified—work‑life balance, personal development, and medical ethics—points to an uncomfortable truth: burnout is both an individual and a systems‑level ethical issue.
Data from multiple studies are blunt:
- Burned out physicians are more likely to make medical errors.
- Burnout correlates with lower patient satisfaction.
- Burnout predicts early retirement, reduced clinical hours, and career change.
So when a system builds a model around:
- “Do more with less staffing.”
- “Maximize RVUs at all costs.”
- “Shift all nonclinical tasks onto clinicians.”
…it is not just creating unhappy doctors. It is degrading patient care. That has ethical weight.
The specialties that “truly struggle the most” are, not coincidentally, the ones that have become pressure valves for systemic failures:
- EM: boarding, lack of inpatient beds, primary care access gaps.
- IM/FM: poor outpatient funding, administrative bloat.
- OB/Gyn: fragmented maternal care systems, liability climate.
If you go into those fields, you are signing up not only for local job strain, but for absorbing the consequences of policy and payment failures. That is moral injury territory, not just burnout.
8. What Actually Helps: Data‑Backed Mitigations
There is a lot of fluff about resilience and wellness. Most of it does not move the numbers by much. But some interventions do show measurable benefit.
From the data, the strongest levers are:
- Reducing workload and after‑hours EHR time (scribes, better templates, realistic panel sizes).
- Increasing physician control over schedule and clinical work.
- Improving team‑based care (APPs, RNs, care coordinators).
- Aligning compensation with work done (including non‑RVU contributions).
- Building a culture where raising safety and workload concerns is not punished.
Those interventions reduce burnout across nearly all specialties. EM and primary care benefit the most because they start in the deepest hole.
On the personal side, the most protective behaviors in survey data:
- Setting hard boundaries on work hours and availability.
- Limiting FTE or shifting to part‑time when possible.
- Diversifying professional identity (teaching, QI, admin) rather than 100 percent RVU‑driven clinical.
You cannot yoga your way out of a 1.5 FTE job crammed into a 1.0 FTE slot. The data on that are clear.


| Category | Value |
|---|---|
| Emergency Med | 58,40 |
| Internal Med | 53,50 |
| Ob/Gyn | 54,48 |
| Family Med | 51,55 |
| Pediatrics | 48,60 |
| Psychiatry | 45,70 |
| Dermatology | 35,80 |

| Step | Description |
|---|---|
| Step 1 | Specialty Choice |
| Step 2 | Workload and Hours |
| Step 3 | Emotional Load |
| Step 4 | Admin Burden |
| Step 5 | Burnout Risk |
| Step 6 | Work Life Balance |
| Step 7 | Practice Setting |

FAQ
1. Which single specialty has the highest burnout rate right now?
Across multiple recent surveys, Emergency Medicine consistently shows the highest burnout rates, often around 55–60 percent. The combination of shift work, trauma exposure, overcrowded EDs, and low control over workload drives that number higher than most other specialties.
2. Are “lifestyle” specialties like dermatology and radiology safe from burnout?
No. They are relatively lower risk, not risk‑free. Dermatology and pathology often report burnout rates in the 30–35 percent range, radiology around 40 percent. Better hours and higher pay help, but factors like RVU pressure, isolation, and business stress still push a significant fraction into burnout.
3. Is burnout more about specialty choice or workplace environment?
Both matter, but environment has more variance. Specialty sets your baseline risk profile; workplace and schedule structure can then double or halve that risk. Within a single specialty, I have seen burnout rates vary wildly between organizations depending on staffing, EHR support, culture, and leadership.
4. How should a medical student factor burnout data into choosing a specialty?
Use the data as a risk map, not a verdict. Identify what you personally tolerate poorly (nights, EHR, emotional trauma, income uncertainty) and avoid specialties where those are baked into the core job design. Then focus on finding practice settings that give you schedule control, team support, and reasonable workload within that field.
Key points:
- No specialty is “safe”; even the lowest‑burnout fields still have about one‑third of physicians affected.
- Emergency Medicine, Internal Medicine, OB/Gyn, Family Medicine, and Pediatrics consistently show the highest burnout burden, but environment and schedule often matter more than the field’s name.
- Treat burnout risk as a quantifiable part of career planning, the same way you would consider income, training length, or match competitiveness.



















