
The obsession with “years of research” on residency applications is overrated. What program directors actually respect is proof that you can start something from nothing and finish it. That is exactly what a smart gap-year project can do for you—even if you have zero research experience right now.
You are not going to turn into an NIH-funded scientist in 12 months. Stop chasing that fantasy. You can, however, build a lean, well-designed project that:
- leads to at least one abstract or poster,
- gives you strong talking points for interviews,
- and makes your letters of recommendation much stronger.
Here is how to do it step by step, from zero.
Step 1: Stop Chasing Unicorns and Pick a Realistic Project Type
You do not have time to learn wet-lab bench science from scratch and push out a first-author paper before ERAS. That is the fantasy that wastes most gap years.
You want fast-to-start, low-infrastructure, analyzable in 6–9 months.
Your safest categories:
Retrospective chart review
- Uses existing patient data.
- You are not waiting to recruit subjects.
- Common in IM, EM, Surgery, Neuro, etc.
Survey-based study
- Can be done with medical students, residents, or patients.
- Fast IRB if minimal risk.
- Flexible topics (education, burnout, clinical decision-making).
Quality improvement (QI) project
- Short cycle.
- Very residency-friendly language (PDSA cycles, metrics).
- Often exempt or expedited review.
Education project
- Example: Creating and evaluating a new teaching module for students.
- Works well if you have access to a med school or residency program.
Anything outside these four buckets, as a true beginner in a single gap year, is usually a bad bet.
Quick reality check: Time vs payoff
| Project Type | Setup Speed | IRB Complexity | Chance of Output in 9–12 Months |
|---|---|---|---|
| Retrospective Chart | Medium | Moderate | High |
| Survey Study | Fast | Low–Moderate | High |
| QI Project | Fast | Low | High |
| Education Project | Medium | Low–Moderate | Medium–High |
If you are already connected to a hospital: lean toward retrospective chart review or QI.
If you are totally disconnected: lean toward survey-based study (students, residents, or online) while you hustle to connect with a clinical site.
Step 2: Anchor Yourself to a Mentor (Even If You Don’t Have One Yet)
You cannot do a credible project in medicine without institutional backing. You need:
- Someone with an appointment at a hospital or university.
- Someone who can be PI (principal investigator) or at least sponsor the project.
- Someone who can later write in your letter, “They took ownership and actually got this done.”
If you already have a mentor, skip ahead. If not, here is the blunt playbook.
2A. Target the right people
You want busy, mid-career people with active CVs but not overloaded with prestige projects, for example:
- Assistant or associate program directors.
- Recently hired attendings who are “expected to produce.”
- Subspecialty faculty in your intended field who have a few publications but not 200.
Find them by:
- Searching your med school or local hospital department webpages.
- Looking at authors on recent departmental posters / abstracts.
- Asking residents, “Who actually gets things done around here and is nice to work with?”
2B. Approach with a concrete, low-friction ask
Do not send: “I’m looking for research opportunities, do you have anything?”
Instead, send something like:
Subject: Gap year project – can I help push something across the finish line?
Dear Dr. X,
I am a [recent graduate / PGY-1 taking a research year] interested in [specialty]. I am looking for a focused retrospective or QI project that can realistically lead to an abstract or poster within 9–12 months.
I can commit [X] days per week and I am comfortable with data entry, basic statistics (willing to learn more), and writing.
If you have any partially completed projects (data collected but not analyzed / analyzed but not written up) that need help getting finished, I would be grateful for the opportunity to contribute.
I am also open to starting a new, tightly scoped project if that would be useful.
Best,
[Name, USMLE scores, school, contact]
This tells them:
- You understand time constraints.
- You are focused on finishing.
- You will handle grunt work.
You are solving their problem, not asking them to solve yours.
Step 3: Define a Narrow Question and Lock It Down
Most beginners make the project too big. That kills progress.
Your research question should be:
- Answerable with data you can realistically get.
- Defined in a single, specific sentence.
- Boringly concrete.
Bad:
“Does sepsis management affect outcomes?”
Good:
“In adult ICU patients with septic shock at Hospital X from 2020–2023, is time to first appropriate antibiotic associated with in-hospital mortality?”
You need to pin down, with your mentor:
- Population (who)
- Exposure / Intervention / Predictor (what)
- Comparison (if applicable)
- Outcome (what you measure)
- Timeframe (when)
Write it as a one-line aim and send it to your mentor for sign-off. This becomes the backbone for your IRB and data collection.
Step 4: Map a Brutal, Simple Timeline
A gap year is not really a year. For ERAS, you need results by August–September at the latest if you want it on your application and in your letters.
So your working window is more like 9 months max. Build backwards.

| Category | Value |
|---|---|
| Month 1 | 10 |
| Month 2 | 20 |
| Month 3 | 35 |
| Month 4 | 45 |
| Month 5 | 60 |
| Month 6 | 75 |
| Month 7 | 85 |
| Month 8 | 95 |
| Month 9 | 100 |
Interpretation:
- Month 1–2: IRB / protocol / training
- Month 3–5: Data collection
- Month 6–7: Analysis
- Month 8–9: Abstract / manuscript drafted, submitted
You want clear milestones:
By end of Month 1:
- Mentor committed.
- Research question finalized.
- Draft IRB or QI proposal written.
By end of Month 2:
- IRB submitted (or exemption confirmed).
- Data dictionary complete.
- RedCap / Excel template ready.
By end of Month 4:
- At least 50% of data collected and cleaned.
- One check-in with mentor to review preliminary descriptive stats.
By end of Month 6:
- Data collection complete.
- Primary analysis done (even if rough).
- Draft figures/tables made.
By end of Month 8:
- Abstract drafted and submitted to something (local/regional/national).
- Manuscript first full draft sent to mentor.
You do not adjust these lightly. If someone is slow with IRB or access, you start a second, simpler project in parallel (for example, a survey or education project) so the whole year does not stall.

| Step | Description |
|---|---|
| Step 1 | Define Question |
| Step 2 | Find Mentor |
| Step 3 | Draft Protocol |
| Step 4 | IRB/QI Review |
| Step 5 | Build Data Tool |
| Step 6 | Collect Data |
| Step 7 | Clean & Analyze |
| Step 8 | Draft Abstract |
| Step 9 | Submit to Conference |
| Step 10 | Draft Manuscript |
Step 5: IRB, QI, and Not Getting Stuck in Bureaucracy
The IRB is where a lot of gap years go to die. You avoid this by keeping risk minimal and design simple.
5A. Make your project IRB-friendly
You want:
- Minimal risk: retrospective, de-identified, no vulnerable populations if possible.
- No intervention beyond standard care unless you really know what you are doing.
- A clear statement that:
- Data will be stored securely.
- Only necessary variables will be collected.
- Identifiers will be removed as soon as feasible.
If it is a QI project:
- Many institutions have a separate QI review committee that can declare it “QI, not human subjects research”.
- That can spare you full IRB review.
Your mentor or a research coordinator should give you a prior approved IRB as a template. Reuse structure and wording aggressively. Do not reinvent the wheel.
5B. Do your basic research training fast
Most places require:
- CITI training (Human Subjects Protection, GCP, etc.)
- HIPAA training for chart review.
Block a weekend and get it done. Then send your certificates to your mentor so they can add you to the protocol.
Step 6: Build a Bulletproof Data Collection System (Before You Touch a Chart)
Beginners jump into the EMR and start writing numbers in Excel. That is how you end up with a garbage dataset you cannot analyze.
You need a data dictionary and standardized input tool first.
6A. Make a data dictionary
For each variable:
- Name:
Age,Sex,ICU_LOS - Type: continuous, binary, categorical, date, etc.
- Allowed values / coding scheme:
- Sex: 0=Female, 1=Male, 2=Other/Unknown
- ICU admission source: 1=ED, 2=Ward, 3=OR/PACU
- Source in chart: where you will actually find it (admission note, discharge summary, flowsheet, etc.)
This document prevents your future self from hating you.
6B. Use a proper tool
If your institution has REDCap: use it. If not:
- Use Excel or Google Sheets with data validation for categorical variables (dropdowns).
- Freeze the header row.
- Lock formulas if you use any.
Split into:
- One row per patient (or per visit).
- One column per variable.
- A unique de-identified study ID for each row.
Before full-scale data collection:
- Do a pilot of 10–20 charts with your template.
- Fix anything confusing. Combine or drop variables you are not actually using.
Step 7: Learn Just Enough Statistics to Not Be Dangerous
You do not need to become a biostatistician. But you absolutely need to:
- Know your primary outcome.
- Choose the main statistic before you start.
- Avoid fishing through 50 comparisons with no plan.
For most simple retrospective or survey projects, you are looking at:
- Descriptive stats:
- Mean ± SD or median (IQR).
- Percentages for categorical variables.
- Group comparisons:
- t-test or Mann-Whitney for two groups (continuous)
- Chi-square or Fisher’s exact for categorical.
- Possibly simple regression:
- Logistic for binary outcomes.
- Linear for continuous.
If your project is more complex, lock in a stats consult early (most universities have them). Show them:
- Your research question.
- Planned variables.
- Sample size estimate.
Do this before data collection ends. They can warn you if your plan is nonsense.

| Category | Value |
|---|---|
| Descriptive | 100 |
| Group Compare | 70 |
| Regression | 40 |
Interpretation: Almost everyone uses descriptive stats; fewer correctly plan comparisons; even fewer set up regression properly. You want to be in that third bar if possible.
Step 8: Design for an Abstract or Poster from Day One
Your goal is not “submit to NEJM.” Your goal is concrete output on your CV before ERAS.
You want at least one of:
- Local hospital or med school research day poster.
- Regional specialty meeting.
- National conference (bonus, not mandatory).
8A. Identify your target conferences early
Could be:
- Specialty-specific (ACEP, ACG, AHA, ATS, etc.).
- General resident/medical student research days.
- State or regional chapter meetings (cheaper, higher acceptance).
Look up:
- Abstract deadlines.
- Word counts and format (structured vs unstructured).
Then plan your timeline around those deadlines. You cannot submit if you discover the conference 3 days before the deadline.
| Conference Type | Approx Deadline | Useful For |
|---|---|---|
| Local Research Day | Feb–Mar | First posters |
| Regional Specialty Mtg | Mar–May | Strong CV signal |
| National Specialty Mtg | Apr–Aug | High impact |
8B. Draft your abstract as you build the dataset
Do not wait until all data are analyzed. You can pre-fill:
- Background: 2–3 sentences.
- Objectives / Aim: your question.
- Methods: design, setting, sample, variables.
Then once you have results:
- Plug in numbers to Results.
- Write a conservative Conclusion that does not overreach.
Mentors love trainees who send: “Here is a full first draft; can you edit?” instead of “What should I write?”
Step 9: Parallel-Track a Simpler Win (In Case the Main Project Stalls)
Smart applicants do not put all their chips on one project. Hospitals delay. IRBs drag. People ghost.
So you run a backup project in parallel that:
- Has no IRB (like a review article or case report).
- Or has extremely fast turnaround (basic survey).
9A. Backup options
Case report or small case series
- Watch for unusual or instructive cases.
- Ask attendings early: “Is this publishable?”
- Use target journal templates (Cureus, Case Reports in Medicine, etc.).
Structured review article
- Not as impressive as original research, but shows scholarly effort.
- Do with a mentor in your specialty.
- Tight topic: “Management of X in Y population,” not “All of cardiology.”
Educational product with evaluation
- Create a small teaching module or OSCE case.
- Pre/post-surveys for learners.
- Easy abstract for med-ed meetings.
These give you additional entries under “Research and Scholarly Activity” in ERAS, even if your main project only reaches the “data collected” stage by application time.

| Category | Value |
|---|---|
| Case Reports | 30 |
| Review Articles | 35 |
| Small Surveys | 35 |
They are not earth-shattering. That is fine. You are building a track record of follow-through.
Step 10: Turn the Work into Interview Firepower
A lot of applicants think the real value is the line on the CV. Wrong. The real value is that now when you get the classic interview question—
“Tell me about a project you worked on.”
—you have a clean, compelling story.
Structure your answer around:
- Problem – what was missing or unknown.
- Approach – what you actually did.
- Obstacles – IRB delay, data access, learning stats.
- Outcome – abstract, poster, ongoing manuscript.
- What you learned – skills and mindset, not just results.
Example:
“At Hospital X, we saw a lot of patients with [condition], but no one had looked at outcomes related to [factor]. I worked with Dr. Y to design a retrospective study of about 300 patients over 3 years. I built the data dictionary, pulled the charts, and did the preliminary analysis in R. We found that [key result], and presented the data at our regional meeting. The biggest challenge was cleaning inconsistent documentation in the EMR, which forced me to standardize definitions and build checks into our dataset. It taught me how important precise methods and data quality are—skills I will bring into QI work during residency.”
That answer says:
- You can take initiative.
- You understand methods.
- You finish what you start.
Which is exactly what PDs want.

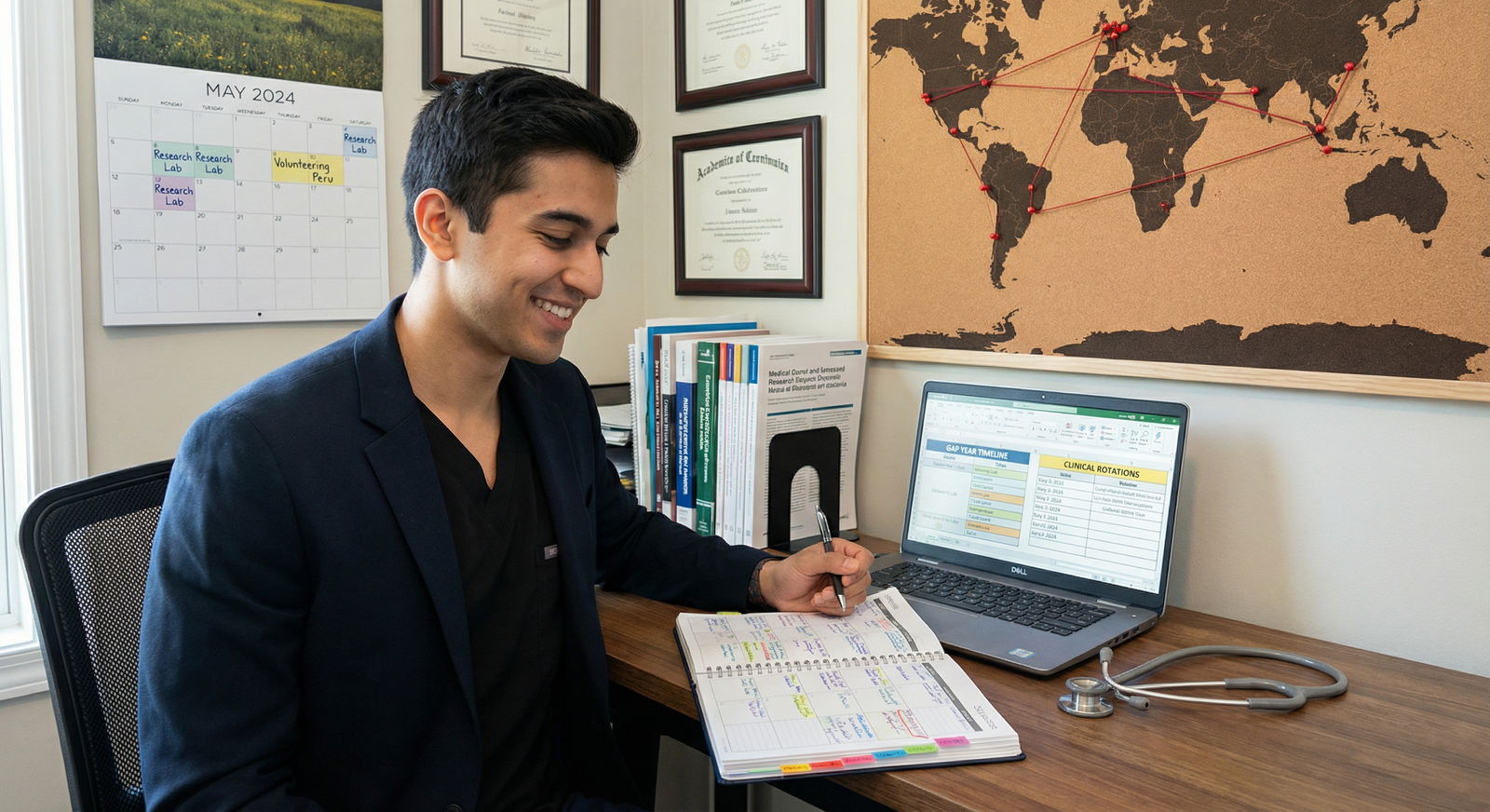
Step 11: Weekly Operating System – How You Actually Spend Your Time
A “gap year” without structure becomes Netflix plus anxiety. You need a weekly operating system.
At minimum:
Two 3–4 hour deep work blocks per week (no phone, full focus).
- One for data / analysis.
- One for writing / reading.
One 30–60 minute check-in with yourself:
- What did I accomplish this week?
- What is blocked?
- What will I do next week?
Biweekly or monthly check-ins with your mentor:
- Send an agenda 24 hours before.
- End with clear next steps and who owns each.
Make it boringly regular. That is how projects move.
Step 12: Package the Year So It Looks Like Strategy, Not Damage Control
When programs see a gap year, they are looking for red flags:
- Burnout?
- Academic trouble?
- Could not match?
You counter that by framing the year as:
- Deliberate skill-building.
- Focused on your chosen specialty.
- Resulting in tangible output.
Your ERAS experiences section for this project should emphasize:
- Your role: “Primary data abstractor and first author.”
- Scope: “N=312 patients,” “Multi-year dataset,” “Interdepartmental QI initiative.”
- Output: “Abstract submitted to [conference],” “Manuscript in preparation,” “Poster accepted and presented.”
Your personal statement can then pull a small part of this as evidence of:
- Curiosity about your specialty.
- Persistence and ownership.
- Maturity after medical school.
Final Reality Check: What Success Actually Looks Like
No, you do not need:
- 10 first-author PubMed papers.
- Multi-center randomized trials.
- R01-level funding.
For a productive gap year from zero, success looks like:
- 1–2 projects where you played a clear, central role.
- At least one poster or abstract accepted somewhere.
- A mentor who is willing to say, in writing, that you were the engine of the project.
- The ability to talk about methods and obstacles like someone who actually did the work.
You start with nothing. You end with:
- Skills.
- A story.
- Evidence of discipline.
That is enough.
Key Takeaways
- Choose a project you can actually finish in 9–12 months: retrospective chart review, survey, QI, or education. Small and focused beats big and unfinished.
- Anchor yourself to a mentor and a timeline early. Get IRB/QI sorted, build a clean data system, and march toward an abstract or poster deadline.
- Use the project to prove who you are. The real value is not the PubMed line; it is the narrative, skills, and strong letter you earn by starting from zero and finishing something real.





















