
The Dual Life of an Intern: Balancing Education and Patient Care in Residency
The transition from medical school to residency training is one of the most intense and defining shifts in a physician’s career. The first year—often called the intern year—is where you move from primarily absorbing information to being directly responsible for patient care. You are still a learner, but now you are also part of the frontline of the healthcare system.
This “dual life” of a medical intern—simultaneously a trainee and a practicing physician—creates unique pressures and opportunities. You must build clinical confidence, master Time Management, continue your Medical Education, and deliver safe, compassionate care, often in high-stakes situations.
This guide explores what actually defines the intern year, the concrete responsibilities you will face, and practical strategies to balance education and patient care without burning out. You will find real-world stories, actionable tips, and a structured way to think about your growth during this pivotal year of your Medical Internship.
Understanding the Intern Year: From Student to Doctor on the Front Lines
The intern year is the gateway to residency. You are no longer “just a student,” but also not yet a fully independent resident. This liminal phase is both exhilarating and disorienting.
What Makes the Intern Year Different from Medical School?
In medical school, your primary job was to learn: attend lectures, study for exams, and practice skills under direct observation. During internship:
- You carry your own patients. You are assigned a patient list, and their day-to-day management is your responsibility.
- Your decisions have real consequences. Orders you place—medications, labs, imaging—directly impact patient safety and outcomes.
- Learning is on-the-job and continuous. “Study time” blends into “work time,” and every patient becomes a potential learning case.
- You are embedded in a complex system. You must navigate consultants, nurses, case managers, social workers, and EMR systems—all while learning your specialty.
The emotional shift can be striking: you sign your own notes, introduce yourself as “the doctor,” and may be the first person a nurse calls at 3 a.m. when a patient deteriorates.
Core Clinical Responsibilities of Interns
Although details vary by specialty and institution, most interns share several key responsibilities in patient care:
Patient Admissions
- Conduct comprehensive history and physical exams (H&P).
- Synthesize information into a working diagnosis and differential.
- Present new admissions to senior residents and attendings.
- Communicate the initial plan to the care team and document thoroughly.
Daily Patient Management
- Pre-round, examine patients, and update daily progress notes.
- Review overnight events, new lab results, and imaging.
- Adjust medications, fluids, and monitoring orders as needed.
- Coordinate tests, consults, and disposition planning.
Diagnostic Reasoning
- Decide which labs, imaging, and tests are actually necessary.
- Interpret results in clinical context—not just whether they are “abnormal.”
- Recognize red flags and escalate care promptly.
Developing and Executing Treatment Plans
- Propose initial management plans under supervision.
- Respond to changes in clinical status (hypotension, hypoxia, delirium, etc.).
- Participate in code situations and rapid response teams, depending on training level and specialty.
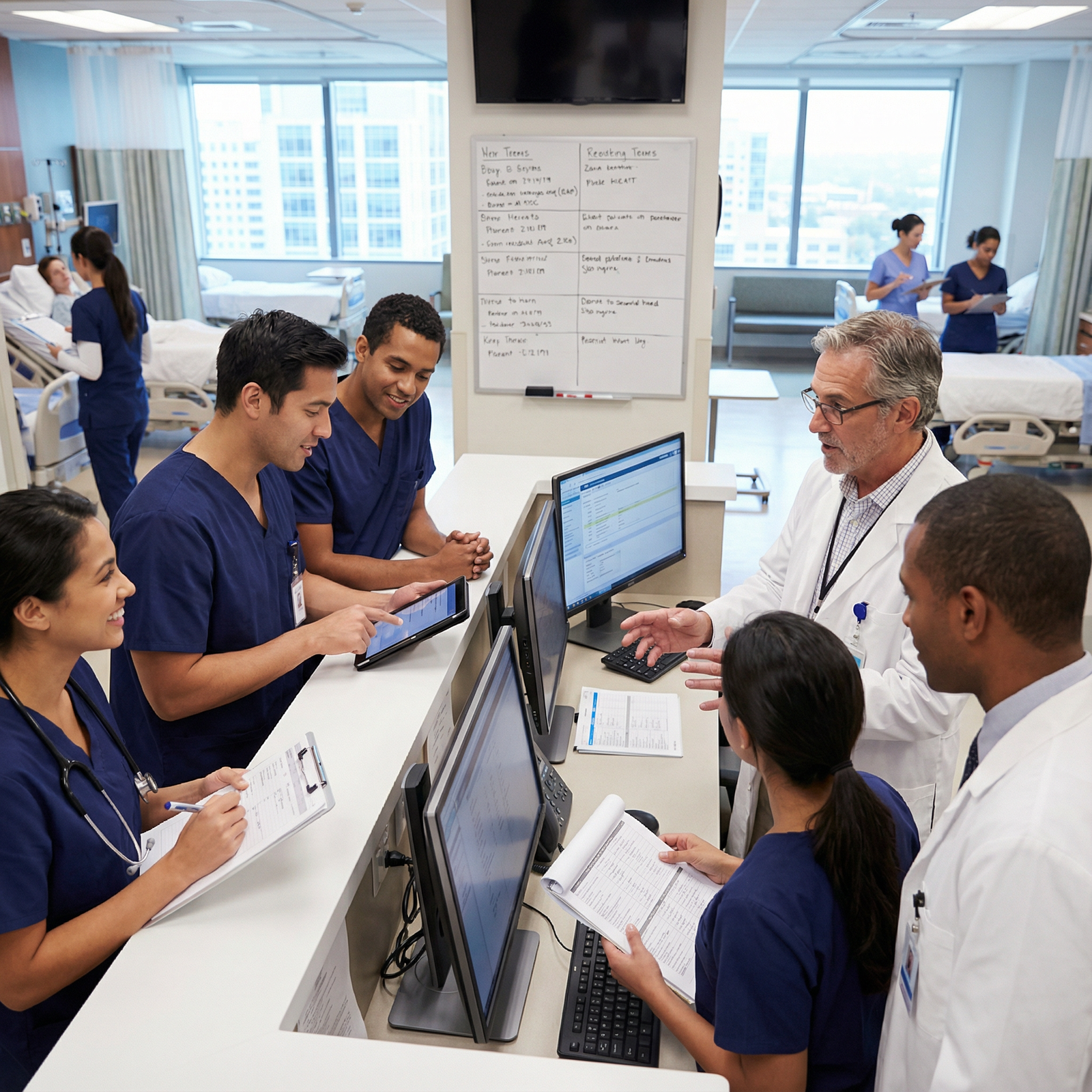
Communication and Teamwork
- Discuss plans with patients and families in clear, empathetic language.
- Update nurses and interdisciplinary team members on evolving plans.
- Present succinctly on rounds, sign-out efficiently during handoffs.
Documentation and Safety
- Write accurate and complete admission notes, progress notes, and discharge summaries.
- Reconcile medications carefully to prevent errors.
- Document critical discussions, goals of care, and shared decision-making.
These responsibilities demand not only clinical knowledge but also maturity, organization, and emotional resilience.
The Core Challenge: Balancing Medical Education with Patient Care Demands
Interns quickly realize that clinic and ward duties will expand to fill all available time unless they protect their education and personal well-being. Balancing both halves of this dual role is not automatic—it requires intentional planning.
At any given moment, you are juggling:
- Immediate clinical tasks (pages, orders, discharges, admissions)
- Short-term educational tasks (reading about current patients, preparing for morning report)
- Long-term professional development (studying for in-service exams, board preparation, building procedural skills)
- Personal needs (sleep, meals, exercise, relationships, mental health)
The goal isn’t to achieve a perfect 50/50 split every day. Rather, it is to integrate learning into patient care and to use structured strategies that prevent one domain from completely eclipsing the other.
Strategies for Balancing Education and Patient Care During Internship
1. Time Management as a Clinical Skill
Effective Time Management is not just an organizational trick; it is a core competency for safe, efficient Residency Training. Poor time management can jeopardize both patient care and your learning.
Build a Daily Workflow
Develop a predictable rhythm to your day, even on variable rotations:
Before Rounds
- Quickly review overnight events in the EMR.
- Pre-round on your patients with focused exams.
- Write or pre-chart progress notes where possible.
- Identify critical issues to discuss on rounds.
During Rounds
- Present concisely and use a problem-based approach.
- Ask 1–2 focused learning questions per patient when time allows.
- Note teaching points to read about later.
After Rounds
- Prioritize tasks using a triage system:
- Stat/urgent: unstable vitals, acute changes, critical labs.
- Time-sensitive: discharges, consult requests, imaging that affects same-day decisions.
- Routine: paperwork, non-urgent follow-ups, non-critical calls.
- Batch similar tasks to minimize switching costs (e.g., write all notes, then call all consults).
- Prioritize tasks using a triage system:
End of Day
- Update your patient list with key issues and contingency plans.
- Give a structured sign-out (e.g., I-PASS format).
- Set one small educational goal for the evening or next morning.
Use Tools Wisely
- Digital calendars and task managers (e.g., Google Calendar, Notion, ToDoist) for deadlines and rotation-specific goals.
- Note templates embedded in the EMR for efficient documentation while ensuring completeness.
- Pocket reference apps (UpToDate, Medscape, MDCalc, specialty-specific apps) to rapidly inform decisions during patient care.
The key is to choose a system you will actually use consistently, not the most complicated one.
2. Embrace Lifelong Learning: Turn Every Patient into a Teacher
Your intern year is the launch of genuine lifelong learning in medicine. Exams are no longer the primary metric; patient outcomes and clinical judgment are.
Set Rotation-Specific Learning Goals
Before each new rotation:
- Identify 3–5 core topics you want to master (e.g., for inpatient medicine: sepsis, heart failure exacerbations, COPD, diabetic ketoacidosis, acute kidney injury).
- Align with your program’s learning objectives and in-service exam content.
During the rotation:
- Pick one “patient of the day” whose condition you will read about in depth.
- Keep a running list of “things to look up later” from rounds or overnight calls.
Make Learning Efficient and Targeted
- Use the “question-driven” approach: when you encounter a clinical problem, articulate a specific question (e.g., “What is the best next test for suspected PE in a pregnant patient?”) and look up the answer.
- Skim guidelines and summaries, then dive into details only for high-yield or confusing topics.
- Apply the 10–15 minute rule: even on busy days, commit to at least 10–15 minutes of deliberate reading.
Leverage Structured Teaching Moments
- Morning report and noon conference: Engage actively, ask clarifying questions, and relate cases back to your own patients.
- Bedside rounds: Observe how attendings gather histories, examine patients, and explain complex issues simply.
- Debriefs and post-call discussions: Reflect on challenging cases, what went well, and what you would do differently.
By linking your study time to real patients, you retain more information and build practical clinical intuition.
3. Master Communication: The Foundation of Safe Patient Care
Interns sit at the center of healthcare communication, bridging patients, families, nurses, residents, and attendings. Strong communication reduces errors, improves patient satisfaction, and makes your day smoother.
Communicating with Patients and Families
- Introduce yourself clearly: “I’m Dr. [Name], the intern working with Dr. [Attending] and the team taking care of you.”
- Practice active listening:
- Let patients speak without interruption initially.
- Reflect back what you’ve heard to confirm understanding.
- Ask open-ended questions before yes/no clarifiers.
- Explain plans in plain language:
- Avoid jargon like “acute coronary syndrome” without explanation.
- Use analogies and visuals when appropriate.
- Set expectations:
- Inform patients when you’ll likely return with updates.
- Share what tests are being done today and why.
This not only improves patient care but also builds trust, which becomes essential when complications or difficult decisions arise.
Communicating Within the Healthcare Team
With nurses:
- Be approachable, respectful, and responsive.
- Ask for their observations; they often detect early signs of deterioration.
- Clarify orders and be explicit about parameters (e.g., when to call you overnight).
With residents and attendings:
- Present succinctly using a structured format (e.g., SOAP, problem-based).
- When calling an attending at night, lead with the “headline” (reason for call and patient risk).
- Summarize decisions at the end of a conversation to prevent misunderstandings.
Seeking and Using Feedback
Feedback is one of the most powerful tools in your Medical Education during internship:
- Ask for specific feedback (e.g., “How can I improve my daily presentations?” instead of “How am I doing?”).
- Request feedback at predictable times (end of rotation, end of week, after a procedure).
- Write down key points and turn them into actionable goals (e.g., “Next week I will ensure all my presentations include a prioritized problem list”).
Feedback might feel uncomfortable at times, but it accelerates your growth and increases your confidence in Patient Care.
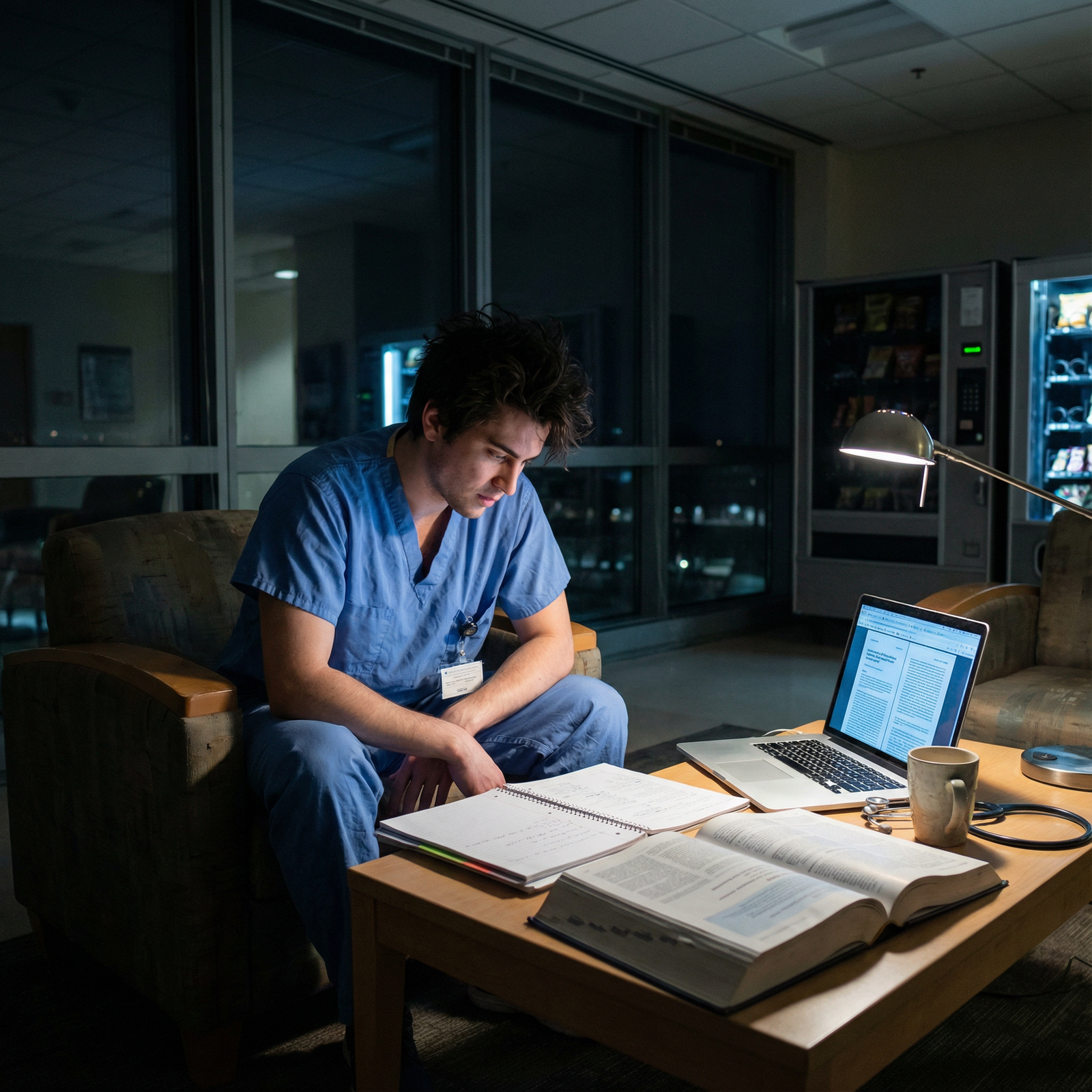
4. Protecting Your Health: Self-Care as a Professional Responsibility
The culture of medicine often glorifies exhaustion, but chronic sleep deprivation and burnout harm both you and your patients. Sustainable performance in Residency Training requires intentional self-care.
Sleep and Fatigue Management
- Aim for consistent sleep windows whenever possible, especially on non-call days.
- After night shifts:
- Use blackout curtains, eye masks, and white noise for daytime sleep.
- Avoid heavy meals, caffeine late in the shift, and long drives when overly fatigued.
- Learn to distinguish normal tiredness from signs of burnout or depression, such as persistent hopelessness, emotional numbness, or loss of interest in things you normally enjoy.
If you notice worrisome signs, reach out early—to a trusted attending, program leadership, mental health services, or employee assistance programs.
Physical and Mental Health Habits
- Nutrition: Keep portable, healthy snacks (nuts, protein bars, fruit) in your bag or locker to avoid skipping meals.
- Movement: Even 10–15 minutes of walking stairs or stretching between pages can improve mood and alertness.
- Stress management: Experiment with:
- Short mindfulness apps (5 minutes of guided breathing).
- Journaling brief reflections after particularly intense days.
- Debriefing tough cases with peers or mentors.
Build a Support System
- Connect with co-interns—they are your closest allies, sharing similar stressors.
- Maintain contact with friends and family outside of medicine when possible; they help maintain perspective.
- Seek a mentor (or several)—someone a few years ahead who remembers what it was like and can normalize your struggles.
Self-care is not selfish; it is an ethical obligation that sustains your capacity to provide consistent, high-quality patient care throughout your career.
Real-World Stories: The Dual Life of an Intern in Action
Case Study 1: The Balancing Act in a Surgical Rotation
During a demanding general surgery rotation, one intern routinely began the day at 4:30 a.m., pre-rounding on a full list of post-op patients before 6:00 a.m. cases. The days blended into a pattern of:
- Early morning rounds
- Long hours in the operating room
- Late-night documentation and discharge summaries
Initially, education felt like an afterthought. However, the intern shifted strategy:
- Between cases, they used 10–15 minute windows to:
- Review upcoming procedures on an anatomy app.
- Skim key guidelines on antibiotic prophylaxis and post-op pain control.
- They asked attendings one focused question per case, such as:
- “What are the early signs of an anastomotic leak we should be watching for?”
- They kept a small notebook of practical pearls from attendings and senior residents.
Over time, surgeries became not just tasks but structured learning experiences, and they finished the rotation more confident in both procedural steps and perioperative care.
Case Study 2: The Transformative Power of Feedback
Another intern struggled with patient communication, especially delivering bad news and discussing serious diagnoses. They felt rushed, anxious, and unsure if patients understood the plan.
Instead of avoiding the issue, the intern:
- Asked a senior resident to observe and critique a family meeting.
- Invited their attending to provide feedback specifically on:
- Structure of the conversation
- Tone and body language
- Clarity of explanations
The attending suggested:
- Using the “Ask–Tell–Ask” framework:
- Ask what the patient understands.
- Tell the information clearly and in small chunks.
- Ask what questions they have and check understanding.
- Pausing intentionally for silence and emotional processing.
Within a few weeks, the intern noticed:
- Smoother family meetings
- Fewer misunderstandings
- Better patient satisfaction comments mentioning that “the doctor explained things clearly”
Regular, specific feedback turned an area of anxiety into a genuine strength.
Case Study 3: Learning from a Documentation Error
An intern once admitted a complex, elderly patient with multiple comorbidities. In the rush of a busy call night, they missed a critical allergy in the medication history. The result:
- A medication was ordered that triggered an allergic reaction.
- The patient required close monitoring, additional treatment, and an extended hospital stay.
The situation was emotionally overwhelming. However, with guidance from the supervising team, the intern:
- Participated in the case review to understand exactly where the process broke down.
- Reflected on personal factors (fatigue, rushing, distractions).
- Developed a new personal safety checklist when admitting patients:
- Always verify allergies verbally and cross-check with prior records.
- Review home medications carefully and reconcile at admission.
- Pause for 10–15 seconds before signing complex orders.
The outcome was a powerful lesson: mistakes, though distressing, can become pivotal growth points if approached with humility and a commitment to change. This experience reshaped the intern’s approach to documentation and patient safety for the rest of their training.
FAQs: Common Questions About the Dual Life of a Medical Intern
1. How many hours do interns typically work during residency?
Intern schedules vary by specialty, institution, and country, but in many U.S. programs, interns often work 60–80 hours per week, within duty-hour regulations. Certain rotations (e.g., inpatient medicine, surgery, ICU) may feel especially intense. Nights, weekends, and 24–28 hour call shifts (where permitted) are common.
What matters most is how you manage those hours—using effective Time Management, prioritizing tasks, and preserving rest when off duty.
2. What is the most challenging aspect of being an intern?
Many interns describe a combination of challenges:
- Emotional load of patient care: Bearing witness to suffering, delivering bad news, and dealing with loss.
- Fatigue and sleep disruption: Long shifts and night work affecting concentration and mood.
- Constant learning curve: Feeling like you “don’t know enough” while being responsible for real patients.
- Competing demands: Trying to balance Medical Education, administrative tasks, and personal life.
These challenges are normal. Over time, experience, mentorship, and structured support from your residency program can make them more manageable.
3. How can interns keep learning effectively while managing heavy clinical responsibilities?
Some practical strategies:
- Integrate study into real patient cases instead of reading in isolation.
- Use small pockets of time (10–15 minutes) for targeted reading, rather than waiting for large uninterrupted blocks.
- Set specific, achievable learning goals each week (e.g., “Understand initial management of sepsis”).
- Attend conferences and teaching sessions consistently, even when tired, and engage actively.
- Seek mentors who can recommend high-yield resources for your specialty and training level.
The goal is not to read everything, but to read strategically, guided by your daily clinical experiences.
4. Is it normal to feel overwhelmed or inadequate during the intern year?
Yes. Feeling overwhelmed, anxious, or like an “imposter” is extremely common in the first year of Residency Training. You are not alone if you:
- Worry about missing something important.
- Compare yourself unfavorably to your co-interns or seniors.
- Feel emotional after difficult patient encounters.
What’s important is to:
- Talk openly with peers and mentors.
- Seek support early if stress feels unmanageable.
- Recognize that growth in medicine is incremental and continuous.
Most interns look back at the end of the year and are surprised by how far they have come in clinical confidence and judgment.
5. How can interns realistically make time for self-care?
Self-care during internship doesn’t mean spa days and long vacations; it’s about small, consistent habits:
- Protect sleep windows whenever you’re not on call; avoid unnecessary late-night screen time.
- Plan ahead with simple, healthy snacks and meals to prevent going all day without food.
- Set boundaries when off duty—allow yourself truly non-work time.
- Incorporate micro-activities: a 10-minute walk, a brief meditation, a phone call to a friend.
- Use days off intentionally—some for rest, some for relationships, some for personal interests.
Remember: you perform better in Patient Care when you are rested, nourished, and emotionally supported.
Balancing education and patient care during your Medical Internship is challenging—but it is also what shapes you into a capable, compassionate physician. By investing in Time Management, embracing continuous learning, honing communication skills, and committing to self-care, you can navigate this transformative year with purpose and resilience, laying a strong foundation for the rest of your residency and your career in medicine.



















