
The first 90 days of internship will break you down and rebuild you.
If they don’t feel hard, you’re probably missing something.
This is not a mindset problem. It’s a load problem. The job is too big for one brain until you grow into it. So you don’t “tough it out.” You phase in your capacity.
Here’s a month-by-month, week-by-week, and zoomed-in daily plan for how to adjust to the workload without burning out or becoming unsafe.
Big Picture: Your 90-Day Curve
At this point you should understand the shape of the year: it’s front-loaded misery with a slow ramp to competence.

| Category | Perceived Workload | Self-Rated Competence |
|---|---|---|
| Week 1 | 9 | 2 |
| Week 2 | 9.5 | 2.5 |
| Week 3 | 9 | 3 |
| Week 4 | 8.5 | 3.5 |
| Week 5-6 | 8 | 4.5 |
| Week 7-8 | 7.5 | 5.5 |
| Week 9-10 | 7 | 6.5 |
| Week 11-12 | 6.5 | 7.5 |
Roughly:
- Days 1–7: Survival and orientation
- Days 8–30: Controlled drowning, learning patterns
- Days 31–60: Systems mastery, speed upgrade
- Days 61–90: Owning your list, anticipating problems
Your goal isn’t to feel good.
Your goal is a safe, sustainable upward curve in how much you can handle.
Month 1 (Days 1–30): Controlled Survival Mode
You’re not here to be impressive in Month 1. You’re here to not harm anyone, not implode, and to build reliable habits.

| Period | Event |
|---|---|
| Week 1 - Day 1-2 | System and workflow orientation |
| Week 1 - Day 3-4 | Take partial patient load |
| Week 1 - Day 5-7 | Own full but light list with close oversight |
| Week 2 - Day 8-10 | Learn night float/page workflow |
| Week 2 - Day 11-14 | Standardize prerounding and notes |
| Week 3 - Day 15-18 | Handle admissions with supervision |
| Week 3 - Day 19-21 | Learn cross-cover style for your service |
| Week 4 - Day 22-26 | Increase patient load gradually |
| Week 4 - Day 27-30 | Identify and fix recurring bottlenecks |
Week 1: Systems, Not Speed
At this point you should:
- Stop obsessing about being fast.
- Ruthlessly focus on not missing dangerous stuff.
Daily structure (template)
- 04:45–05:15 – Wake, shower, caffeine
- 05:30–06:30 – Preround: vitals, I/Os, labs, quick exam on sickest 3 first
- 06:30–07:30 – Finish preround + draft plans, one-line summaries
- 07:30–09:30 – Team rounds
- 09:30–12:00 – Orders, pages, discharges, calls
- 12:00–13:00 – Eat. Sit. If you can’t sit to eat, something upstream is broken.
- 13:00–17:00 – New admits, follow-ups, notes
- 17:00–19:00 – Sign out prep, last checks, sign out
First 3–5 days, your only real goals:
- Learn:
- How to place every common order in the EMR (labs, imaging, diet, nursing orders, DVT ppx, insulin).
- Where people actually are: phlebotomy, radiology reading room, case manager, blood bank.
- Build:
- A templated note for your main service (IM, surgery, OB, whatever).
- A pre-round checklist you follow blindly until it’s automatic.
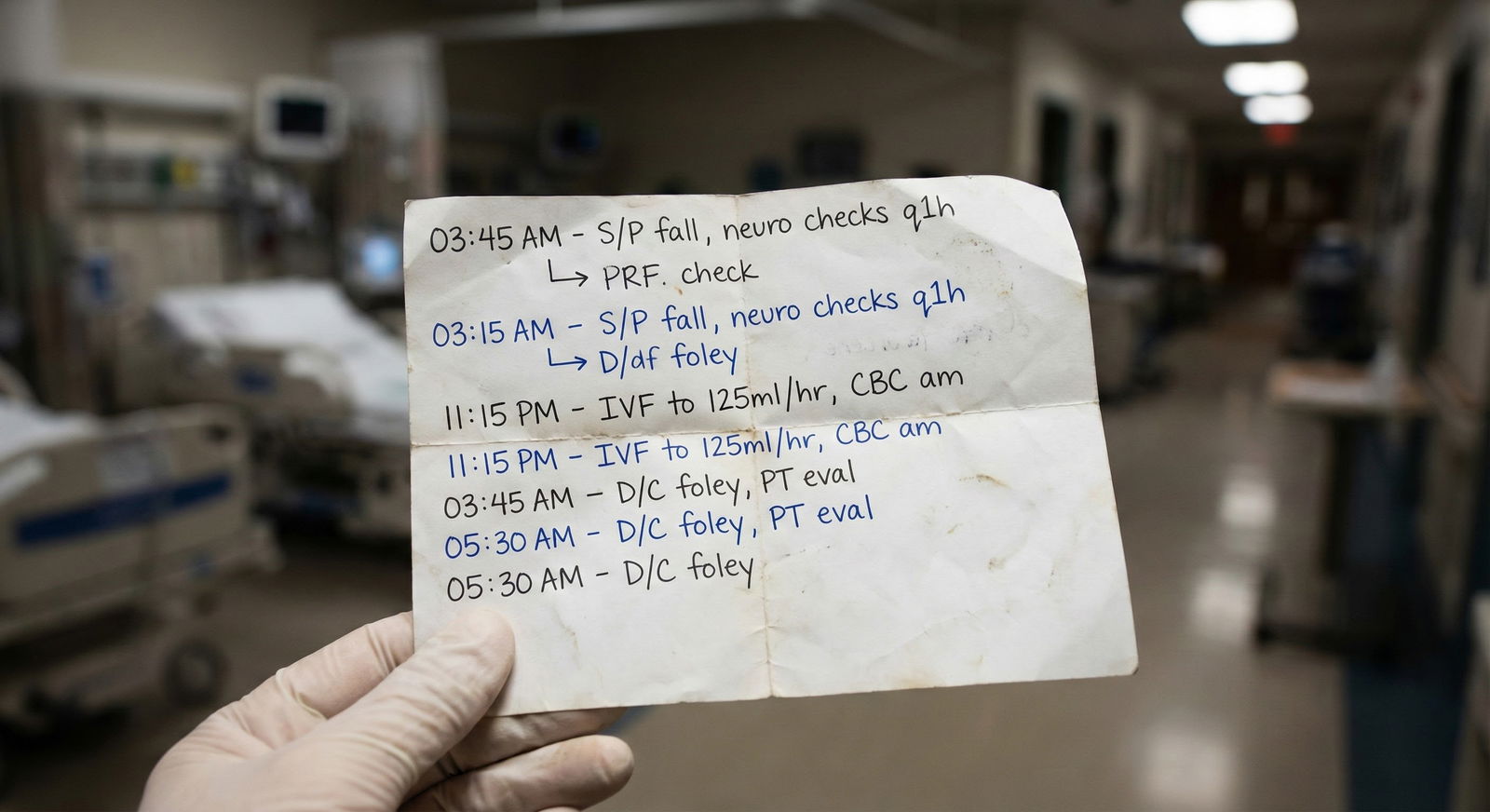
Example AM pre-round checklist (internal medicine style):
- Open patient list
- For each patient:
- Skim overnight events + nursing notes
- Check vitals, pain scores, I/O
- Labs/imaging results and pending
- Med rec: new meds started, any high-risk drugs
- Brief exam focused on: mental status, lungs, heart, edema, abdomen
- One-line summary + 3-bullet plan in your notebook
Do not try to “remember it all.” You won’t. Write it all.
Week 2: Standardizing Your Day
Now that you can basically find things, you shift to making every day look the same.
At this point you should:
- Have a consistent rounding order (by location, then by acuity).
- Be using the same structure in every H&P and progress note.
- Be asking your senior, every single day:
“What did I do today that slowed us down?” and “What can I batch better?”
Common Week 2 upgrades:
- Batch your EMR time
- Don’t click labs 40 times. Open all patients, then check labs for the whole list at once.
- Same for reviewing imaging, placing routine orders, updating problem lists.
- Script your most common calls/pages
Examples:- For “pain uncontrolled”: exact questions + standard order patterns.
- For “patient hypotensive”: focused checklist in your head—confirm vitals, symptoms, recent meds, fluids, lines, bleeding, sepsis flags.
Week 3: Taking Real Ownership
You’re still new, but you’re no longer fragile-new.
At this point you should:
- Be able to present your patients clearly without your senior rescuing you.
- Write most progress notes in 5–7 minutes each, not 20.
- Carry a “normal” intern list for your service (often 6–10 patients dayshift on a busy IM service, more/less depending on specialty).
This is the week to:
- Start anticipating:
- “This person will need SNF → loop case manager early.”
- “This creatinine is creeping up → adjust meds today, not tomorrow.”
- Learn discharge workflows:
- Med reconciliation fast and safe.
- Follow-up appointments.
- Standard instructions for your common diagnoses (CHF, COPD, post-op wounds, etc.)
Week 4: Fixing Your Bottlenecks
By week 4, your weak spots are painfully obvious.
At this point you should:
- Be able to name three specific workflow problems you keep hitting:
- Example: notes always lag until 4 p.m.
- Example: constantly behind on discharges.
- Example: you get crushed by pages between 10–12.
- Have a clear plan with your senior/attending to address them.
Tactical changes you can make now:
- Move discharge planning as early as possible:
- Pre-write discharge summaries the night before when appropriate.
- Put “possible discharge today?” in your morning script.
- Use micro-handoffs:
- Loop in nurses early: “I’m hoping to discharge 12A before noon; anything we can set up now?”
- Protect 30 minutes post-rounds:
- Do not let anyone pull you into something else until:
- All critical orders are in
- All stat labs/imaging are ordered
- Sickest patients rechecked
- Do not let anyone pull you into something else until:
Month 2 (Days 31–60): From Surviving to Efficient
Now your brain isn’t screaming all day. Time to increase capacity and reduce cognitive load.
Weeks 5–6: Deliberate Speed Upgrade
At this point you should:
- Stop adding “more effort” and start adding structure and automation.
- Know your most common 5–10 diagnoses cold for your service.
This is where you introduce standard operating procedures (SOPs) for yourself.
| Scenario | Your Personal SOP Focus |
|---|---|
| New CHF admission | Fixed admission checklist & order set |
| New fever overnight | Workup steps & when to call senior |
| Pre-op clearance | Standard history, labs, consults |
| Hyperkalemia | Stepwise treatment and recheck timing |
| Safe discharge | Med rec, follow-up, red-flag teaching |
You don’t reinvent them every time. You reuse the same pattern, adjust for the person.
Concrete weekly goals here:
- Cut your average progress note time by 25–30%.
- Reduce the number of times your senior has to:
- Correct your plans
- Tell you you missed labs or imaging
- Reorient your presentation
How to do it:
- Time yourself. Literally:
- One day: “How long did morning prerounds take? Notes? Discharge paperwork?”
- Next day: aim to trim 10–15 minutes from the worst chunk by batching and restricting EMR wandering.
- Build 3–5 smartphrases/templates in your EMR:
- For H&P, daily note, discharge summary, post-op check, cross-cover event.
Weeks 7–8: Managing Higher Complexity
This is where you stop thinking in isolated tasks and start thinking in the list.

| Category | Low-complexity tasks | Moderate-complexity tasks | High-complexity tasks |
|---|---|---|---|
| Week 1-2 | 8 | 2 | 0 |
| Week 3-4 | 7 | 4 | 1 |
| Week 5-6 | 5 | 6 | 2 |
| Week 7-8 | 3 | 7 | 4 |
At this point you should:
- Routinely handle:
- Multiple sick patients at once (e.g., one in step-down, one borderline in the ED).
- Admissions during the day while managing a full list.
- Start to triage your own attention:
- Sickest first
- Time-sensitive discharges early
- Stable but complicated tasks later
This is where you refine your list management system:
- One master list (paper or digital), updated:
- Immediately after rounds
- After each significant event (new imaging, code, transfer)
- For each patient:
- 1-liner
- Today’s 3 must-do tasks
- Pending studies + who’s responsible for following them
You should also:
- Start recognizing which things can safely wait:
- Non-urgent med changes
- Chronic issue discussions
- Optimization that won’t change same-day care
- And which never wait:
- New chest pain, new neuro deficit, true hypotension, mental status changes, rapid O2 needs.
Month 3 (Days 61–90): Owning Your List
By Month 3, you’re no longer “the new intern.” The grace period is fading. Expectations go up.
Weeks 9–10: Anticipation and Prevention
At this point you should:
- Be comfortable running the list with minimal prompting.
- Begin predicting which patients might decompensate or need ICU transfer.
- Start calling consults with a clear, concise story.
This is the “see around corners” phase.
Your daily mental checklist for each patient:
- What can go wrong in the next 24 hours?
- What can I do now to make that less likely?
- If things go bad at 2 a.m., what information or orders should already be in place?
Examples:
- Borderline O2 needs?
- Early RT consult, standing nebs, wean plan, clear notify parameters.
- Delirium risk?
- Sleep protocol, minimize lines, reduce restraints, family involvement.
You’re also starting to:
- Teach the medical students or observers (briefly, concisely).
- Handle low-level social friction yourself: difficult families, annoyed nurses, confused consultants.
Weeks 11–12: Running Like a Junior, Not a Student
By the end of 90 days:
At this point you should:
- Present clearly, propose plans, and accept feedback without falling apart.
- Handle a typical call pattern for your service without panicking.
- Know when to call for help, and do it early—not when the BP is 60/40 and the patient is gray.
This is when your seniors start to “trust-but-verify” rather than “hover-and-rescue.”
You’re expected to:
- Pre-round faster but more focused (sickest, newest, most complex first).
- Anchor discharges:
- Identify them early
- Push the process
- Clear obstacles (PT/OT, social work, insurance)
- Maintain personal sustainability:
- You’ve found some rhythm for sleep on your rotations.
- You have a pre/post shift micro-routine that keeps you sane.
Micro-Level: Daily and Weekly Checklists
You don’t grow by vague reflection. You grow by tight feedback loops.
Daily: 10-Minute Post-Shift Reset
At this point, every day, you should take 10 quiet minutes before you leave the hospital (or before bed if you must) and run through:
Three questions
- What did I do today that made the team faster or safer?
- What did I drop or almost drop?
- Where did I feel that “I’m lost” feeling?
Two decisions
- One workflow tweak for tomorrow (e.g., “Check all vitals before leaving the workroom in the morning”).
- One thing to ask your senior about (“Can you watch me call this consult?”).
Weekly: 20–30 Minute Self-Debrief
Once a week—ideally on your lighter day—you do a quick structured review.

At this point each week you should:
- List:
- 2–3 clinical situations you handled well
- 2–3 that felt messy or out of control
- Ask:
- What pattern do these share? Time of day? Type of patient? Specific task (discharges, codes, consults)?
- Plan:
- One learning target for the coming week (e.g., “diabetic ketoacidosis ICU management basics”).
- One workflow target (e.g., “finish all notes by 4 p.m. at least 3 days this week”).
When Things Start to Break (Because They Will)
You will hit a wall. Usually around weeks 3–5, and again around weeks 8–10.
Common signs:
- You’re constantly staying 1–2 hours late just catching up on notes.
- You dread going in, not because of work, but because you feel out of control.
- You’re snapping at nurses or co-interns.
At this point you should not just “try harder.” You should:
- Grab your senior and be explicit:
- “I’m drowning in discharges and notes. Can we walk through my day and see what I should change?”
- Ask for targeted help:
- “Can you show me how you prep for rounds?”
- “Can I shadow you for one admission and then you shadow me for the next?”
- Use your program’s resources:
- Chief residents, mentor faculty, wellness/program director if things are really going sideways.
This is not weakness. It’s the difference between interns who plateau early and interns who keep climbing.
Quick 90-Day Progress Snapshot
Here’s how your responsibilities shift over the first three months.
| Timeframe | Primary Focus | What You Should Be Doing |
|---|---|---|
| Days 1–7 | Orientation & Safety | Learn systems, follow checklists, over-communicate with senior |
| Days 8–30 | Building Habits | Standardize notes, solidify prerounds, handle full but supervised list |
| Days 31–60 | Efficiency & Volume | Faster notes, more admissions, anticipate problems, call smarter consults |
| Days 61–90 | Ownership & Anticipation | Run your list, predict issues, teach students, manage complex days |
Final Thoughts
Three points and you’re done:
- The first 90 days are not about proving you’re brilliant; they’re about proving you’re reliable and safe.
- At every stage—week 1, week 4, week 9—you should be tightening your systems, not just trying to “work harder.”
- When you feel overwhelmed, that’s a signal to change the workflow, not your worth. Adjust the system, ask for targeted help, and keep your curve pointed up.




















