
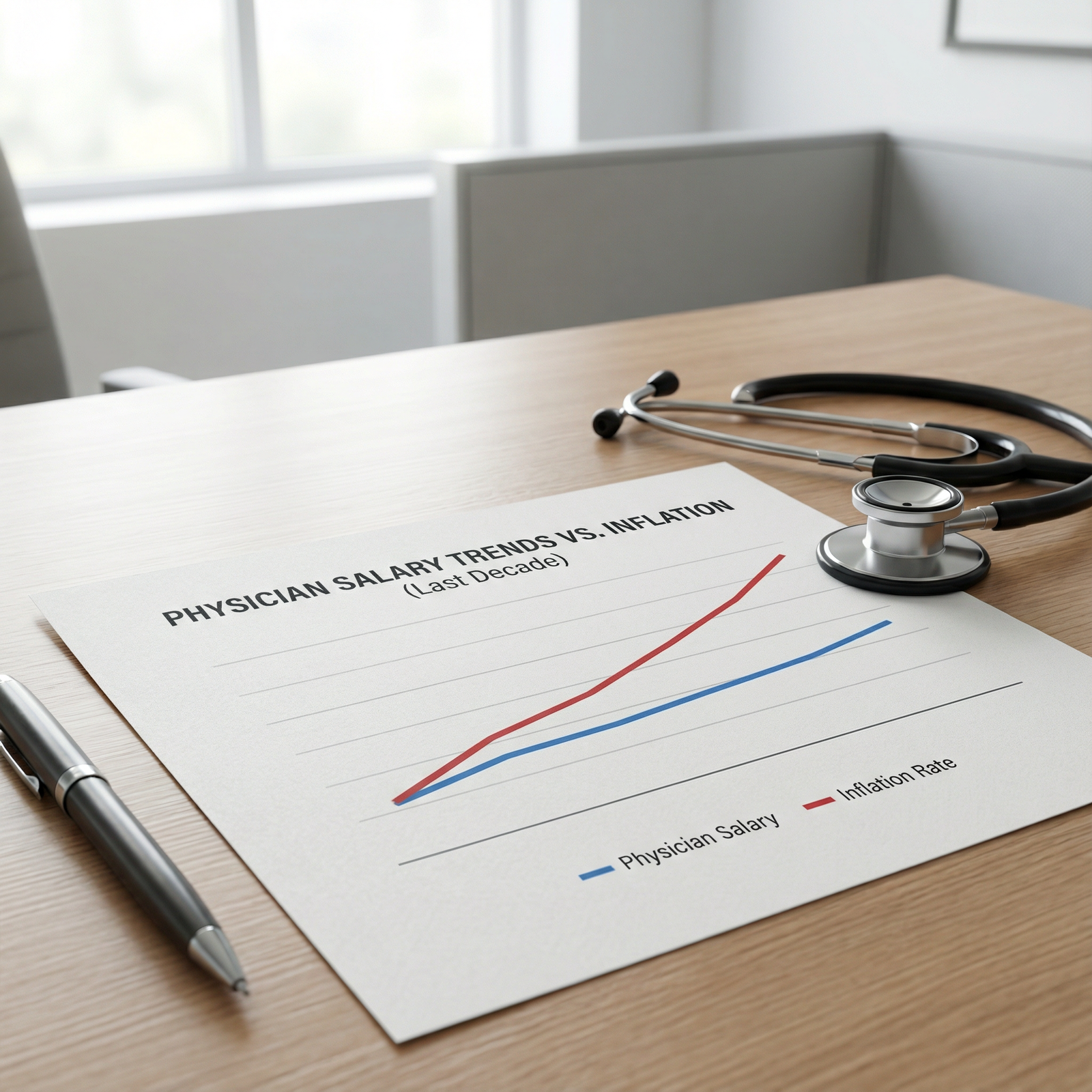
The myth that physician salaries only go up is wrong. The data from the last decade shows clear cycles: spikes, plateaus, and quiet cuts hidden behind “productivity adjustments” and “revised compensation models.”
If you are a physician or about to be one, you are not operating in a straight-line market. You are in a cyclical labor market tied to reimbursement, private equity cycles, residency bottlenecks, and payer mix shifts. The numbers are brutally clear once you line them up.
Below I am going to walk through what the data shows about salary peaks and troughs from roughly 2013–2024, how those cycles differ by specialty, what drives the swings, and what this means for your next contract negotiation.
1. The Decade in Four Hiring Cycles
You can cut the last decade into four distinct compensation cycles. Not vibes. Quantitative shifts in median pay and signing behavior across surveys like MGMA, Medscape, AMGA, and multiple large recruiter datasets.

| Category | Value |
|---|---|
| 2013 | 100 |
| 2015 | 108 |
| 2017 | 116 |
| 2019 | 125 |
| 2021 | 138 |
| 2023 | 145 |
| 2024* | 147 |
(*2013 = index 100; 2024 projected based on partial-year reports.)
Cycle 1: Post‑ACA Expansion (2013–2016)
Data pattern:
- Overall median compensation growth: roughly +3–4% per year nominal.
- Primary care: stronger relative gains (often 4–6% per year) as systems scrambled to build outpatient access and “population health” capacity.
- Procedural subspecialties: still rising, but slower, often just outpacing inflation.
Mechanisms:
- Medicaid expansion in many states increased volume for hospital systems.
- Large systems pushed employed models; independent practices sold.
- Demand strongly favored FP/IM/hospitalists in community and rural settings.
You see it in the numbers: family medicine comp moving from the low $180Ks to the low/mid $200Ks, internal medicine pushing from low $200Ks to ~230K–240K by 2016 in many regions, while hospitalist total comp often crossed $250K in community settings.
Cycle 2: Tightening and Plateau (2017–2019)
Median compensation still went up. But the growth rate fell.
- Typical year-over-year overall growth: closer to 1.5–2.5%.
- Many primary care roles saw flat base salaries with slightly higher RVU or quality bonuses.
- Rural and underserved markets still paid aggressively; metros started to plateau.
The pattern I kept seeing in data and contracts:
- Signing bonuses for standard IM/FM in mid‑tier metros narrowed to $10K–$20K after having been $25K–$40K in early expansion years.
- Relocation assistance stayed, but less “sweetener” money.
- More offers shifted to heavy productivity—RVU multipliers up, but base kept modest.
Cycle 3: COVID Shock and Bidding War (2020–2022)
This is where the charts kink.
- 2020: short-term pain (furloughs, elective shutdowns) followed by a rapid rebound.
- 2021–2022: pronounced jump in median comp, especially for hospital-based and high-demand specialties.
The drivers are obvious once you look at vacancy and locums rates:
- Systems were desperate for hospitalists, anesthesia, EM, intensivists, pulm/critical care.
- Telemedicine spiked, expanding some outpatient and urgent care demand.
- “Danger pay” effect: retention bonuses, crisis stipends, and aggressive locums rates.
Between 2019 and 2022, composite survey data shows:
- Primary care medians jumping ~12–18% total.
- Hospitalists up closer to ~15–20% in some regions.
- Anesthesia, radiology, GI, cardiology: many reports of 10–15% gains, more in shortage markets.
Cycle 4: Post‑COVID Hangover and Quiet Softening (2023–2024)
The current phase is more subtle. Base salaries on paper rarely fall. But the total economics are clearly softening in multiple specialties.
Patterns I see repeatedly in recent data and contracts:
- Nominal medians still inch up ~1–2%, which is negative in real (inflation-adjusted) terms.
- RVU thresholds are nudged upward; conversion factors flattened.
- Call pay and extra shifts reduced or moved to “rotation expectations.”
- EM and some hospitalist positions restructured, especially after overstaffing corrections.
So yes, the spreadsheet still says you are making $10K more. Your actual effective hourly compensation, adjusted for workload and inflation, often says otherwise.
2. Peaks and Troughs by Specialty: Who Rode the Cycle Best?
The market did not treat everyone equally. The spread between “winners” and “laggards” in this decade is huge.
A simple comparative snapshot
These are approximate, directional figures based on aggregating multiple national reports; real numbers vary by region, practice type, and experience.
| Specialty | 2013 Median ($k) | 2019 Median ($k) | 2023 Median ($k) |
|---|---|---|---|
| Family Medicine | 185 | 225 | 260 |
| Hospitalist IM | 230 | 280 | 330 |
| Emergency Med | 270 | 350 | 380 |
| General Surgery | 330 | 380 | 430 |
| Anesthesiology | 340 | 400 | 470 |
Again, these are ballpark, not regional guarantees. The ratios are the point.
Primary care: slow burn, then COVID pop
Over the decade:
- Cumulative increase roughly 35–45% nominal for FM/IM.
- Real (inflation-adjusted) gains are smaller but still positive.
You see two mini‑cycles:
- 2013–2016: Steady gains as systems build outpatient and coverage networks.
- 2020–2022: COVID workload and retention driven raises and stipends.
The trough was around 2017–2019 when base offers stagnated and more comp was pushed into RVUs or quality metrics. Many new grads complained of “same salary as residents five years ago,” and they were not far off in real terms.
Hospitalists: from must‑have to “how many do we really need?”
Hospitalists were the poster child for the COVID spike. I have seen:
- Shift rates that jumped from ~$150/hour to $200–225/hour in hot markets during 2021.
- Annual comp offers climbing from high $200Ks to mid $300Ks, with aggressive bonuses.
Then systems did the obvious: once staffing stabilized, they recalibrated.
- Newer offers in 2023–2024 have kept “headline” salaries high but:
- More shifts per month required.
- Extra-shift rates quietly cut.
- Night coverage redesigned (e.g., combining tele‑nocturnist with in-person backup).
On paper: peak likely 2022. In practice: peak “earnings per shift” also 2022, with a trough forming now for new grads in saturated markets.
Emergency medicine: clearly past a peak in many markets
If you want a clean example of a visible peak and then softening, you look at EM.
Trend:
- 2013–2018: robust growth as ED volume and payer complexity drove demand.
- 2019: peak confidence, strong hourly rates, plenty of locums.
- 2020–2021: chaos. Short-term spikes for COVID surges, but also volume volatility.
- 2022–2024: oversupply warnings come true; more grads, corporate groups rebasing contracts.
Common data points from recent years:
- Hourly rates in some regions shaved from $220–250 down to $180–210.
- Fewer full partnership-track options; more employed or contract roles with limited upside.
- Shift counts per FTE creeping up.
Median comp statistics can lag. Locally, many EM physicians will tell you 2018–2021 was the true income peak.
Procedural subspecialties and anesthesia: still strong, but more uneven
Specialties like GI, ortho, cardiology, radiology, and anesthesiology have stayed at the top of the pay distribution. But they are not immune to cycles.
Anesthesiology: acute shortage in many regions, especially when CRNA supply is tight.
- I have seen offers move from low $400Ks to high $400Ks / low $500Ks plus large sign‑ons.
- Some markets, though, have seen rebasing when groups lose hospital contracts to larger entities.
Radiology: teleradiology changed the game. Huge range now.
- High-comp remote roles during peak COVID and post‑COVID surge.
- Some flattening more recently as more telerad players enter and groups consolidate.
Ortho/GI/Cardiology: often tied to procedural volume and private equity moves.
- PE roll‑ups drove aggressive short‑term compensation (salary + distributions).
- When acquisitions slow or reimbursement is pressured, net income can compress quickly.
3. Regional and Practice-Type Cycles: Not One Market, Many
Talking about “the” physician job market is lazy. The data point to at least three overlapping markets: rural/underserved, second‑tier metros/regional systems, and major metros/academic centers.

| Category | Rural / Underserved FM | Metro FM |
|---|---|---|
| 2014 | 210 | 190 |
| 2017 | 230 | 210 |
| 2020 | 260 | 230 |
| 2023 | 290 | 250 |
Rural and underserved: persistent premium, cyclical sweeteners
The data show a stable pattern:
- Base salaries 10–25% higher than comparable metro roles for primary care, hospitalist, general surgery, and psychiatry.
- Richer sign‑on bonuses: $40K–$100K is not rare in truly hard‑to‑staff locations.
- Loan repayment often stacked on top (state + federal + employer).
The cycle effect: during tight labor periods (post‑ACA expansion and COVID years), these premiums spike further. When the overall market softens, rural areas still pay above metros, but the gap narrows slightly or sweeteners get more structured (e.g., retention bonuses instead of up-front cash).
Metro and academic: prestige discount and slower cycles
Academic centers and desirable metros show a different curve:
- Smaller amplitude. You do not see +20% jumps overnight.
- Slower response to both booms and busts; budgeting cycles and hierarchies dampen changes.
- Persistent “prestige discount” or “lifestyle discount” compared to private practice and rural.
Over 2013–2023, median academic salaries have lagged private practice by 15–30+% in many fields. COVID did not fully erase that, though some centers used retention raises and bonuses to keep core staff from walking.
Private practice vs employment: different exposure to cycles
Employed physicians feel the cycles in their contracts. Private practice owners feel it on their P&L and K‑1s.
Patterns:
Employed:
- Peaks show up as higher base, richer sign‑ons, retention bonuses.
- Troughs show up as higher RVU thresholds, tighter bonuses, new “productivity expectations,” and more aggressive non‑competes.
Private practice:
- Peaks show up as strong collections, fat partner distributions, and aggressive hiring.
- Troughs show up as slower collections, lower partner draws, higher buy‑in risk, and sometimes practice sales.
In 2020–2022, many private groups enjoyed record years once elective volumes returned and relief funds stabilized hospitals. In 2023–2024, as inflation hit overhead (staff, rent, supplies) and payers tightened, net income flattened or slipped even when top-line collections looked decent.
4. What Actually Drives These Compensation Cycles?
The narrative explanations (“doctors are burned out,” “healthcare is changing”) are useless without quantification. The underlying drivers that actually show up in the numbers are more specific.

1. Reimbursement and payer mix shifts
Whenever CMS tweaks RVU values or conversion factors, or commercial plans renegotiate, the downstream effect hits physician comp with a lag.
Typical chain:
- Reimbursement compression in a specialty → hospital/practice margin squeezed → new contracts emphasize productivity and tighten bonuses → median comp growth slows or flattens.
On the other side:
- New billable services (e.g., certain telehealth codes) or higher RVUs → more room for generous comp models.
Data reality: After adjusting for inflation, many specialties have seen flat or declining reimbursement per unit of work over the decade. Compensation cycles partly represent attempts to keep physicians motivated in a worsening payer landscape.
2. Training pipeline vs demand
Residency and fellowship slots are a slow-moving variable. Demand can surge or fall within 2–3 years; supply takes a decade to respond.
So you get:
- Shortages and spikes:
- Psychiatry, anesthesiology, certain surgical subspecialties, and rural primary care have recurring shortage conditions. Results: high sign‑ons, loan repayment, partnership offers.
- Oversupply and softening:
- Emergency medicine has been the classic story here recently: residency expansion + corporate staffing models + volume shifts → downward pressure on new‑grad offers.
Whenever a specialty adds a lot of residency positions without a proportional increase in funded positions or patient demand, expect compensation troughs for new entrants.
3. Corporate and private equity cycles
You can almost overlay private equity roll‑up waves on compensation swings in some outpatient specialties: dermatology, ophthalmology, GI, anesthesia, radiology.
The pattern:
- Acquisition / roll‑up phase:
- Aggressive offers, large buy‑ins or buy‑outs, higher short‑term comp to lock in volume.
- Consolidation / harvest phase:
- Pressure to meet EBITDA targets, cost cutting, standardized comp tables, more RVU productivity, less upside sharing.
For employed doctors inside these structures, your salary may keep rising 1–2% annually. The real peak and trough live in your bonus potential and in how much ownership or profit sharing exists for physicians versus investors.
4. System-level shocks: COVID is the obvious one
COVID did three things simultaneously:
- Collapsed elective volume initially (temporary trough).
- Triggered massive acute demand for hospital-based care and coverage (spike in urgency).
- Pushed burnout from background noise into a measurable attrition factor.
The result: a short but dramatic “bidding war” phase for certain specialties and locations.
You can see it clearly in locums data:

| Category | Value |
|---|---|
| 2018 | 145 |
| 2019 | 150 |
| 2020 | 165 |
| 2021 | 190 |
| 2022 | 200 |
| 2023 | 175 |
The 2021–2022 spike is not a rumor. It is what happens when systems must fill shifts at any cost. The 2023 drop is what happens once staffing stabilizes and budgets reassert themselves.
5. How to Use These Cycles in Your Own Negotiations
Knowing that cycles exist is not just trivia. You can actually use this information in contract timing, structure, and risk management.

Time your moves when possible
You cannot fully time the market like a stock, but you can avoid obviously bad moments.
- Trying to negotiate an EM salary peak in 2024 the way you might have in 2018 is fantasy.
- Switching hospitalist jobs at the height of a surge (e.g., 2021) gave massive leverage; switching after volume and staffing normalize gives less.
Look at:
- Locums rates in your specialty and region as a leading indicator of desperation.
- Vacancy postings over time. If listings are shrinking and response times to your CV are slower, leverage is weaker.
Focus on structure, not just headline salary
Cycles express themselves first in structure before they touch base pay.
Red flags that you are entering a softening phase for your niche:
- Higher RVU thresholds for the same base as last year’s cohort.
- Quality/bonus tied to system-level metrics you do not control.
- Longer guarantee period required before full productivity model (and then a steep drop).
- “Market adjustment” if collections fall, written into contract.
During a soft market, you push for:
- Longer guarantee periods.
- Clear RVU conversion factors and thresholds locked in for several years.
- Reasonable expectations for panel size or shift counts.
- Specific, numeric bonus criteria.
Geographic arbitrage is real
The data is monotonous on this point: the same specialty and seniority will earn more in:
- Rural / smaller cities vs coastal major metros.
- Private / community systems vs large academic centers.
You do not have to stay there forever. One high‑earning cycle in a rural environment can dramatically accelerate debt payoff and savings, especially if you catch the upswing of a shortage-driven spike.
6. Where We Are Likely Headed Next
No one can model this perfectly, but current data supports a few directional bets for the next 3–5 years.

| Period | Event |
|---|---|
| 2024 | Mild softening, slower nominal growth |
| 2025 | Continued pressure in oversupplied specialties |
| 2026 | Selective spikes in shortage areas psych, rural primary care, anesthesia |
| 2027 | New equilibrium, more heavily productivity-based comp |
| 2028 | Next policy or funding shock likely resets some trends |
Likely trends:
Real income pressure
Nominal salaries might still inch up, but inflation and overhead will erode real gains unless reimbursement sees a structural improvement. Expect more “work harder for the same real pay” offers.Divergence by specialty
High‑need areas (psychiatry, certain surgical subspecialties, anesthesia, rural IM/FM, geriatrics) are likely to see localized spikes when shortages become painful. Oversupplied fields (EM in some markets, certain IM subspecialties) will keep feeling downward pressure on new‑grad offers.Heavier use of variable comp
Systems have figured out that base salary increases are sticky. Bonuses and RVU structures are not. More comp tied to productivity, quality, and system metrics is almost guaranteed.Less tolerance for “COVID premium” contracts
Any temporary hazard-pay policies or inflated locums rates are being walked back. If your current contract was negotiated at or near the 2021–2022 peak, expect renewal friction.
Key Takeaways
- Physician compensation over the last decade has been cyclical, not linear—distinct peaks around 2021–2022 and quieter troughs around 2017–2019 and emerging again post‑COVID.
- The size and timing of those cycles differ sharply by specialty, geography, and practice type; primary care, EM, hospitalists, and procedural subspecialties have all ridden very different curves.
- You can use these cycles to your advantage by watching locums rates and vacancy patterns, prioritizing contract structure over headline salary, and being willing to shift geography or practice setting when the data show your leverage is highest.


















