The Step 1 pass/fail era did not make residency selection kinder. It just pushed the spotlight onto your Dean’s Letter.
Let me tell you what really happened behind the scenes once Step 1 went pass/fail: program directors didn’t suddenly become holistic, zen gatekeepers of fit and wellness. They panicked for a month, opened ERAS, and said the quiet part out loud in committee meetings:
“Alright. If we can’t sort them by Step 1 anymore, we’re going to live in the MSPE now.”
And that’s exactly what they did.
How Programs Actually Used Step 1 Before Pass/Fail
Forget the brochure talk. Before pass/fail, Step 1 was the blunt weapon.
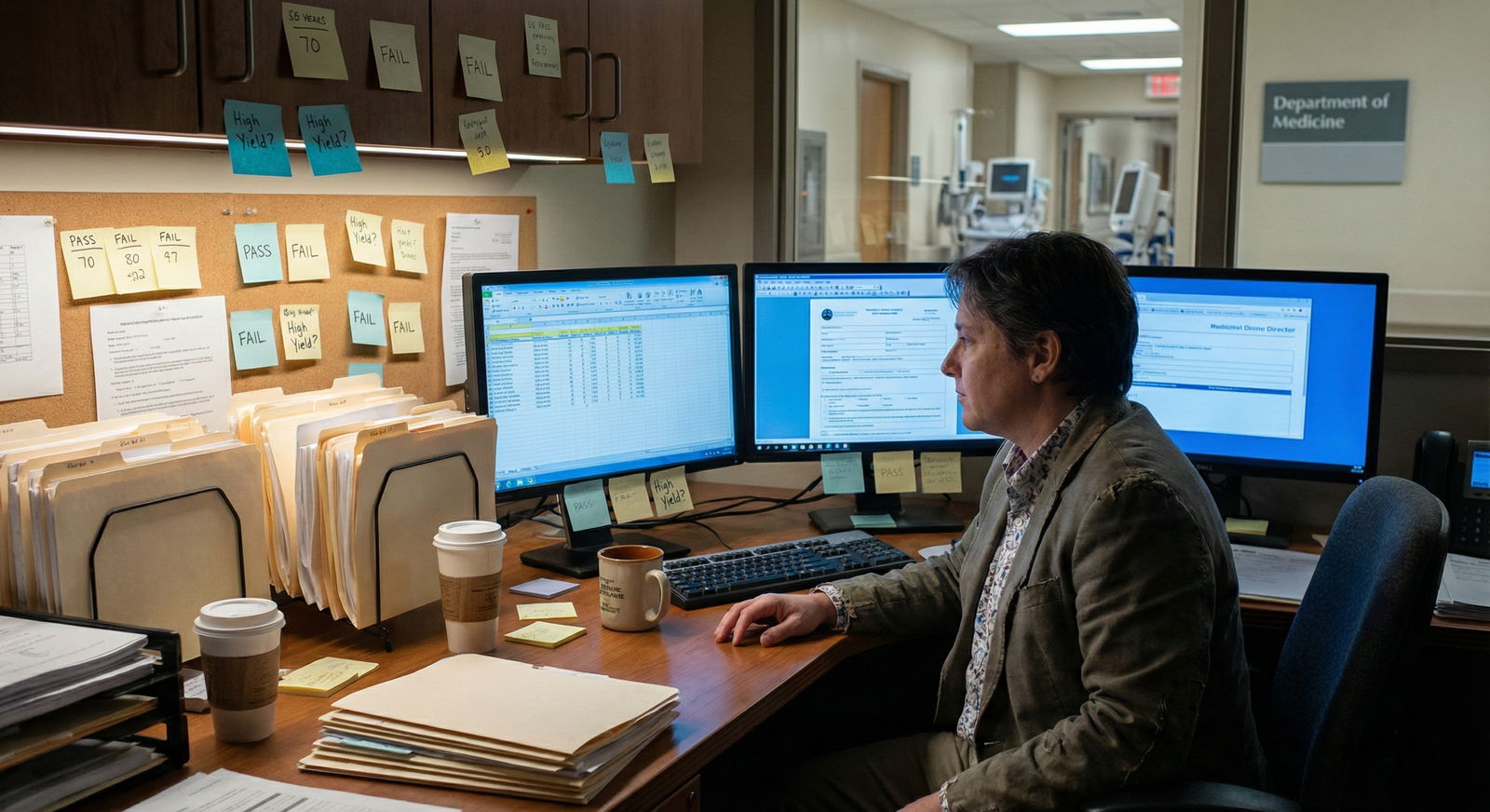
In a lot of programs, the “screen” was a filter set in some ugly internal system or an Excel spreadsheet your chief resident updated every September. I’ve actually watched it happen live:
Program director opens ERAS → exports to CSV → adds a Step 1 column → sets “show only ≥ 230” or “≥ 240” → hits filter → 3,000 apps become 700. Then faculty pretend they “reviewed” everyone.
That was the workflow. No mystery.
Different programs had different numbers, but the function was the same: use one objective score to avoid drowning. Then use Step 2, clerkship comments, research, and letters to stratify that smaller pile.
Once Step 1 went pass/fail, everyone said, “We’ll be more holistic.” On paper. In real life, the committee meeting changed to:
“No Step 1. So what’s our primary screen now?”
The answer: your Dean’s Letter (MSPE), with Step 2 quietly becoming the new hard number behind it.
The Quiet Promotion of the MSPE
The MSPE used to be that long PDF no one actually read unless they were on the fence or looking for red flags.
Now? It’s front and center. And it’s being used in ways most students do not understand.
Here’s how the change really played out at multiple programs I’ve seen:
First year after pass/fail: chaos
Faculty opened apps and instinctively scrolled for Step 1… and found “Pass.” No spread. No sorting. They grumbled, then started scanning MSPEs like radiology reads, looking for patterns that could replace what Step 1 gave them.Second year: systems updated
Internal spreadsheets changed. Filter columns became:- Step 2 CK
- MSPE “summary ranking” or quartile
- Clerkship honors count
Third year and beyond: MSPE became the de facto “academic composite”
PDs use Step 2 plus MSPE to screen in, then the narrative parts of the MSPE to screen out.
The MSPE is now the closest thing they have to a structured, school-endorsed representation of your performance, behavior, and trajectory.
You’re thinking, “But my school says the MSPE is just a ‘summary’ and not evaluative.” Residency folks laugh at that line every year.
What PDs Actually Look At in the MSPE First
Let’s strip it to what people really do when they open that PDF.
The average faculty reviewer does not lovingly read your entire MSPE beginning to end. They skim aggressively, hunting for specific signals. The sequence is surprisingly consistent.

| Step | Description |
|---|---|
| Step 1 | Open MSPE PDF |
| Step 2 | Jump to Summary/Final Paragraph |
| Step 3 | Scan Class Rank/Tier |
| Step 4 | Check Clerkship Grades Table |
| Step 5 | Scan Narrative for Red Flags |
| Step 6 | Look for Superlatives/Praise |
| Step 7 | Keep in Interview Pool |
| Step 8 | Move to Maybe/Reject |
| Step 9 | Any concerns? |
Here’s what they’re keying in on:
The summary or “Dean’s letter” paragraph
This is where your school “codes” you. Programs know the synonyms. They learn the language of each school over time.- “Outstanding” vs “Excellent” vs “Very good” → these are not random adjectives; they map to tiers.
- “She will be a solid resident” often means “not a star, but safe.”
- “He will do well in a program that can provide strong support” sets off alarms. That line has tanked more applications than any single B+.
Explicit or implicit ranking / quartile
Many schools claim, “We don’t rank.” The PDs roll their eyes. They decode your standing anyway using:- Preclinical/clinical comments about “top X%”
- Honors count in core clerkships
- Comparative phrases like “among the strongest students I have worked with in the past several years” (translation: top tier) vs “has met expectations” (translation: middle of the pack at best)
The grades table
That boring grid with “Honors / High Pass / Pass” by clerkship is now heavily weighted.The quick mental math PDs do:
- 5–6 Honors in cores → “Okay, strong student, probably fine clinically.”
- Mostly High Pass with a few Honors → “Average to above-average, depends on narrative.”
- Mostly Passes → “We need an explanation,” especially for competitive fields.
Red flag section or euphemistic phrases
If your MSPE has an explicit “concerns” section? That’s the new radioactive zone. More subtle is the soft-coding:- “Needed closer supervision at times”
- “Struggled with time management early but improved”
- “Responded to feedback over time”
Translation in faculty mind: “There was a problem. We’re not telling you all of it.”
Clerkship narratives
Not every line, but patterns:- Do you repeatedly get called “quiet,” “reserved,” “needed prompting”?
- Or do you get “leader,” “go-to student,” “quickly integrated into the team”?
Once Step 1 went away, all this moved from background noise to first-pass screening material.
The New Screening Stack: How Apps Are Really Sorted Now
Let’s be blunt: Step 1 did not vanish. It fragmented.
Programs now use a stack:
| Priority Order | Screening Signal |
|---|---|
| 1 | Step 2 CK Score |
| 2 | MSPE Summary/Tier |
| 3 | Core Clerkship Grades |
| 4 | Narrative Red/Green Flags |
| 5 | Research / Fit Factors |
And parallel to that, they’re glancing at school name, but less than applicants think.
Step 2 is the new hard numerical gate, but it doesn’t live alone. It’s validated—quietly—by the MSPE. PDs are asking:
- “Does this Step 2 match the level of clinical performance described here?”
- “Is this 250 attached to someone who barely passed rotations, or someone who crushed them?”
Most of you were told “Step 2 will replace Step 1.” Wrong. Step 2 is the number. The MSPE is the context. Both matter more than they did before.
And when there’s no Step 2 yet at application time? The MSPE steps into center stage.
How Different Types of Schools Get Read Differently
This part nobody tells you publicly.
Programs do not read every MSPE with the same baseline assumptions. After years of applicants, they know each school’s pattern. They keep mental (and sometimes literal) cheat sheets.
I’ve watched PDs pull a binder or PDF labeled “School MSPE Key” during review. They know, for example:
- School A (elite private): Honors are scarce. So 2–3 Honors can mean “excellent.”
- School B (newer program): Honors are generous. So 10 Honors may equal “average top-half.”
- School C (state school): Doesn’t officially rank, but “outstanding” in the summary = top 10%; “excellent” = next 20–30%.
They start from those priors, then read your letter.

| Category | Value |
|---|---|
| Well-known School | 30 |
| Moderately Known | 40 |
| New/Unknown | 55 |
That bar chart is essentially the mental weighting. The less they know about your school, the more heavily they lean on the exact language of the MSPE. Because they can’t trust their gut on grade inflation or curve structure, they watch every adjective like it’s a lab value.
For students from less-known schools: that letter isn’t just part of your app. It is your brand.
How This Shift Changes the Game for You (and Where Students Get Burned)
Here’s the ugly realization students come to in late MS4, right before rank lists: what really mattered was being “MSPE-optimized,” and nobody ever said that out loud.
Let me translate that.
1. Your clerkships are now Step 1 + LORs + PS rolled into one
In the old world:
- Step 1 = raw number for screen
- Clerkship grades = “nice to have”
- LORs = variable
- PS = fluff unless extreme
Now the MSPE packages all of those clinical signals and stands in as your core evaluation.
So the student who coasted on strong preclinical grades, planning to “fix it later with a good Step 1,” just lost their safety net. If your third-year performance was inconsistent, that inconsistency is now frozen in institutional amber.
2. Small behavioral issues are now amplified
I’ve seen the same story 100 times:
- Late twice on surgery. Mild conflict with a resident on medicine. A professionalism form that “was handled internally.”
- At your school, people forget by M4. No big scandal.
- But the MSPE holds on to a line like “We counseled her on timeliness, which improved” or “He occasionally required reminders regarding documentation expectations.”
When Step 1 was king, that line might’ve been overlooked if the student had a 260. Now that line is the only “objective” sign of how you behave on a team.
Programs are terrified of problem residents. One vague professionalism hint can move you from “interview” to “maybe later” pile instantly.
3. The middle-of-the-pack student is more exposed
Under the old system, a very average clinical performer could still blast a 250 and ride that into interviews at programs that never looked closely at clerkship comments.
That door is narrower now. PDs don’t have a spread on Step 1, so they’re relying heavily on MSPE tiers and clerkship grades to identify their top third.
The fat part of the bell curve—the “solid but not special” group—is where MSPE language becomes life-or-death:
- “Consistently performed at the expected level for training” can be a kiss of death at a hyper-competitive program.
- “Frequently sought out learning opportunities, well-liked by the team” can be enough to keep you in the pool even if your grades aren’t perfect.
What Faculty Say About MSPEs When You’re Not in the Room
You want the real talk? Here’s the kind of language you’ll hear at an actual selection meeting:
- “This kid’s from a school that inflates. They’re only ‘excellent’? Probably middle-tier.”
- “A lot of ‘quiet but reliable’ comments. Might struggle on our busy service.”
- “Summary says she’s in the top 25%. With this Step 2, that’s a buy.”
- “Two mentions of ‘time management’ across rotations? Hard pass. We don’t have capacity to babysit.”
There’s also a game PDs play: triangulation.
They’ll look at your MSPE, then your individual LORs, then your personal statement, asking one question: “Does the story match?”
- MSPE calls you “quiet and thoughtful,” PS paints you as dynamic leader of everything? That mismatch breeds distrust.
- MSPE narrative says “outstanding fund of knowledge, go-to for peers,” letters echo that, and your Step 2 supports it? That consistency is gold.
How Step 2 and MSPE Interact Now
Step 2 CK is not optional in this era. Programs want a number. But the number is interpreted through the MSPE lens.

| Category | Value |
|---|---|
| Step 2 CK Score | 45 |
| MSPE/Dean Letter | 35 |
| Other Factors | 20 |
Here’s the nuanced part:
- High Step 2 + strong MSPE → green light at most places you’re regionally plausible for.
- High Step 2 + mediocre MSPE → “might be a test-taker, but not a star on the wards.” Risky in procedure-heavy or team-heavy specialties.
- Average Step 2 + strong MSPE (top tier, glowing narratives) → still very interviewable; PDs will say, “Good clinician, maybe not a gunner on exams.”
- Lower Step 2 + mixed MSPE → tough combination unless you’ve got something else extraordinary (major research, unique background, strong connections).
You can’t hide a weak MSPE behind a strong Step 2 anymore the way you could hide mediocre clinical comments behind a 255 Step 1. The Dean’s Letter is simply too prominent now.
The Future: MSPEs Are About to Get More Standardized and More Weaponized
Here’s the next twist you’re not being prepped for.
There’s a quiet movement among PDs: they want more standardization of MSPEs. Translation: more explicit ranking, clearer comparative language, and easier ways to sort you.
Some schools are resisting, but many are already caving in subtle ways:
- Adding explicit “top X%” language
- Creating more detailed grade distributions
- Providing competency-based tables
Programs love this. It gives them more ways to use the MSPE as a sorting tool now that Step 1 is flat.
That means your individual third-year attendings and clerkship directors now effectively write Step 1 plus LOR plus rank all at once, baked into one letter your Dean signs.
You will not get a second chance at that composite.

So What Do You Actually Do With This Information?
I’m not going to insult you with “work hard all the time.” You already know that. This is about strategy, not platitudes.
Think in terms of MSPE impact from day one of clinicals:
- On every core rotation, ask yourself: “If my performance this month had to represent me in one paragraph two years from now, what line would I want that paragraph to contain?”
- Behavior that used to be “fine” now shows up as coded language. Chronic lateness, disengagement, eye-rolling, being “too busy” for scut—all of it gives attendings ammunition that, once written, follows you to every program director in the country.
- Conversely, small positive behaviors get amplified: volunteering for admissions, staying late on a rough day, being the student everyone wants back.
Also, you should know this: some students do strategically request meetings with their Dean’s office when MSPE drafts are being prepared. Politely, not aggressively. They correct factual errors, offer context for outlier events, and sometimes nudge vague negativity into neutral phrasing.
The students who treat the MSPE as sacred and untouchable? They often get blindsided by how those “small comments” read to jaded eyes on the other side.

You are allowed to care how you’re summarized. You should.
And one more uncomfortable truth: your classmates who are savvy about this will quietly ask older students to “translate” MSPE language from your school, so they know the words to aim for. You should too.

Quick Reality Check: Timeline of Where MSPE Hits You
If you’re early in med school, you may not realize when this thing actually matters. Here’s the rough application-year rhythm:

| Period | Event |
|---|---|
| Early Summer - Jun-Jul | School compiles MSPE, integrates clerkship data |
| Application Opening - Sep | Students submit ERAS, MSPE uploading |
| Screening - Oct-Nov | PDs use MSPE plus Step 2 to screen |
| Interview Season - Nov-Jan | MSPE guides borderline decisions and ranking |
By the time you’re obsessing over your personal statement in August, the most powerful document in your file—the MSPE—is already largely fixed. That’s why you cannot think of this as an M4 problem.

FAQs
1. My school says they don’t rank us. Does that protect me?
No. Programs will reverse-engineer your tier from whatever data they can get: honors count, language in the summary, any mention of “top X%,” and historical patterns from prior applicants. “No rank” just forces them to read the MSPE even more closely.
2. Can I actually influence what goes into my MSPE?
Yes, to a point. You cannot rewrite history, but you can (and should) correct factual errors, provide context for outlier events, and respectfully ask about phrasing that implies a professionalism concern if that’s not accurate. Students who engage professionally with their Dean’s office often end up with cleaner, clearer letters.
3. If my MSPE is mediocre, is my application doomed?
Not necessarily, but you lose margin. A strong Step 2, powerful specialty-specific letters, and a coherent track record (research, leadership, fit) can offset a non-glowing MSPE, especially in less cutthroat specialties or at programs that know your school well. But no one is rescuing an application with repeated professionalism hints or a clearly bottom-tier summary. That’s the new gravity in the Step 1 pass/fail era.
The core reality is this: Step 1’s fall didn’t make the game fairer. It just moved the battlefield from a test center to your clinical rotations and your Dean’s office.
Three things to hold on to:
- Your MSPE is now one of the top two screening tools, right next to Step 2.
- Third-year behavior and clerkship narratives live longer than any exam score.
- The people writing and compiling your MSPE are shaping your residency options more than most students realize—until it’s too late.













