Step 1 going pass/fail did not make residency selection kinder or more holistic. It just forced programs to weaponize everything else.
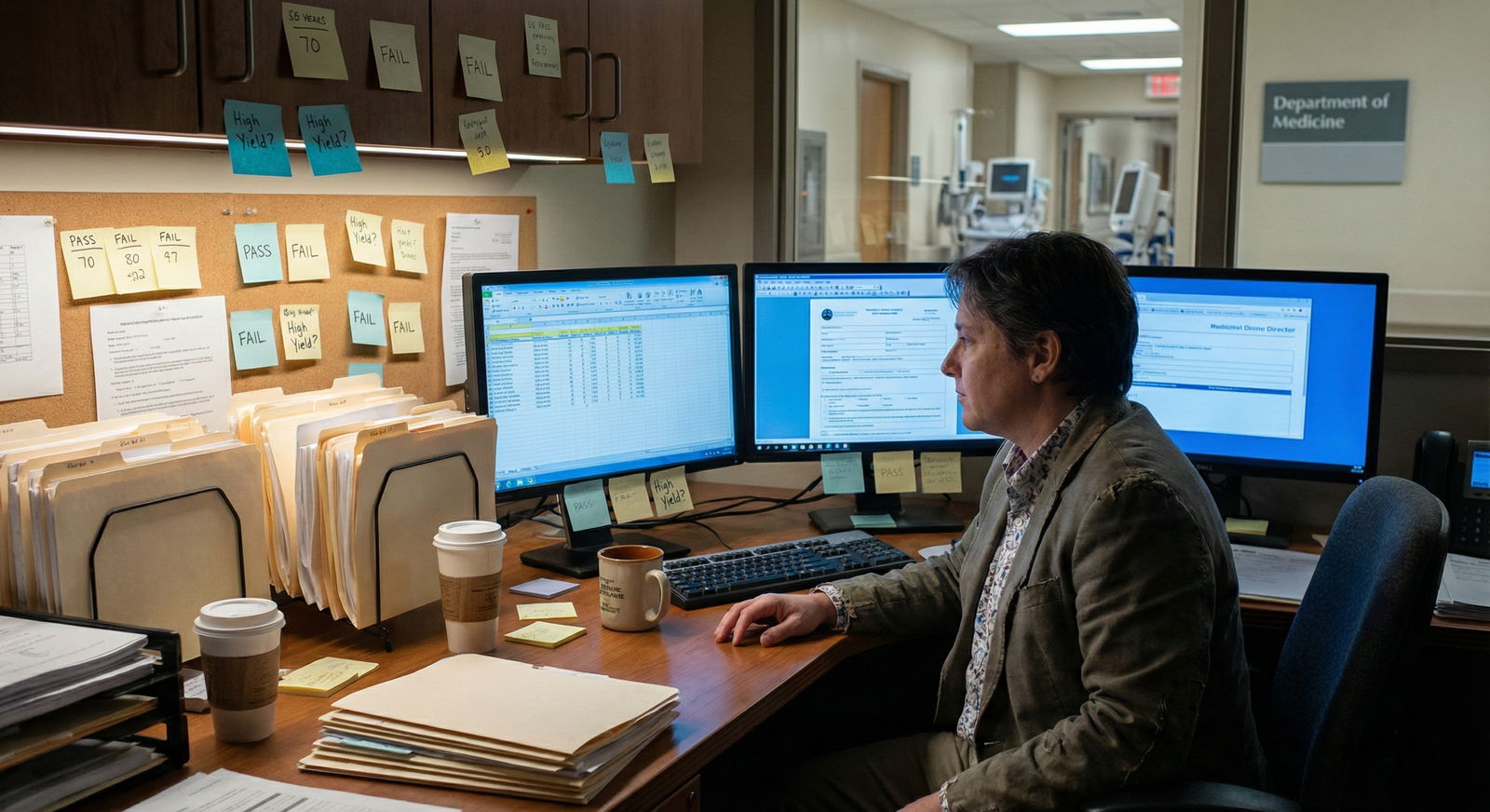
I sat in those rooms when the change hit. Faculty were not suddenly excited to read 8,000 personal statements. PDs did not wake up and decide, “Let’s really get to know each applicant as a whole person.” They said, almost verbatim: “We’ve lost our blunt instrument. What can we use now that’s fast?”
Here’s what they use now. And how ruthlessly.
The New Gatekeepers: What Actually Replaced Step 1
Step 1 didn’t disappear. It just stopped being useful as a filter. Committees immediately shifted to a different short list:
- Step 2 CK score
- School reputation / Dean’s letter signal
- Clinical grades and honors (especially core rotations)
- SLOEs / letters from known faculty
- Research output – and where it was done
- A surprisingly aggressive screen on “professionalism flags”
The honest version: very few programs meaningfully “holistic review” thousands of files. They build a quick filter, auto-screen a big chunk, then only “get holistic” with the survivors.
Let’s break down the hierarchy as it’s actually applied.
Step 2 CK: The New Blunt Instrument
The day Step 1 went pass/fail, Step 2 CK quietly became the new Step 1. Anyone telling you otherwise is selling something.
I heard a PD in a competitive surgical subspecialty say this the first cycle after the change:
“We used to cut at 240 Step 1. We’ll just move that expectation to Step 2.”
They meant it.

| Category | Value |
|---|---|
| Step 1 Score | 90 |
| Step 2 CK | 20 |
| Clerkship Grades | 40 |
| Letters | 30 |
| Research | 30 |
Before: Step 1 score was king.
After: Step 2 CK sits on the throne, but now it has more advisors.
Here’s how PDs actually use Step 2:
First-pass screen.
They export an ERAS spreadsheet, sort by Step 2, and start drawing lines. The exact number varies by specialty and region, but the behavior is the same: “We have 2,000 apps. We’re not reading 2,000 files. Where can we cut?”“What’s their ceiling?” question.
Without Step 1, Step 2 is the only standardized academic marker across schools. Committees know clerkship grades are inflated. They don’t trust your school’s “Honors” rate. But a 262 is a 262 everywhere.Tie-breaker for borderline files.
Say you’re from a mid-tier school, average research, generic letters. A 255 Step 2 suddenly buys you a second look. A 225 does not.
If you want to understand how programs roughly think now, it’s something like this (this is not published anywhere; this is back-room talk):
| Specialty Type | Soft Screen Zone | Comfortable Zone | Red Flag Zone |
|---|---|---|---|
| Ultra-competitive (Derm, Ortho, ENT, Plastics) | 240–245 | 250+ | <235 |
| Competitive (Anes, EM, Rads, Urology) | 235–240 | 245+ | <230 |
| Mid (IM, Gen Surg, OB/GYN at solid programs) | 230–235 | 240+ | <225 |
| Less competitive (FM, Psych, Peds at many programs) | 220–225 | 230+ | <215 |
These are not hard rules. But they’re frighteningly close to how preliminary shortlists get made.
Two more ugly truths:
- If you delay Step 2 so your score isn’t out when applications go out, many programs will just skip you for interview invites. They want something numerical in hand.
- If you bomb Step 2, committees will dissect your whole file looking for an explanation. If they do not find a credible story, you quietly slide into the “no” pile.
School Name & The Dean’s Letter: The Signal Nobody Admits They Use
When Step 1 was scored, a 260 from a no-name school could punch into elite programs. That still happens, but less. The school’s brand has quietly become a stronger filter now that one major objective number is gone.
Here is what PDs say when the applicants are not in the room:
- “I know what ‘Honors’ means at UCSF. I have no idea what it means at Midwestern Regional College of Medicine.”
- “If they did well at X top-20 school, I’m comfortable their training is legit.”
- “We don’t have time to decode grade inflation at every school.”
Translation: your institution’s reputation is their heuristic for academic rigor and professionalism. Especially in less-known or brand-new schools, this hurts.
Then there is the MSPE (Dean’s letter). Most students think nobody reads it. Wrong. Faculty on committees absolutely read it—specifically three parts:
The “Noteworthy Characteristics” section.
They scan for any hint of problems or for unusually strong praise. Over-the-top generic fluff, they ignore. Concrete descriptions of leadership, resilience, or unique path stand out more now than before.The comparative language.
Deans can’t use exact class rank, but they absolutely use coded language. Things like- “Outstanding student” = top tier
- “Strong student” = fine but not stellar
- “Solid performance” = middle
Committees have decoded their regular feeder schools. If you think they haven’t, you’re naïve.
Professionalism comments.
Any whisper of concerns? They treat it like smoke from a fire. I watched an otherwise strong file get killed in 90 seconds because the MSPE alluded to “needing reminders about timely documentation.” The PD said, “We don’t need that headache.”
With Step 1 gone as a numerical equalizer, those subtleties in your Dean’s letter now carry more weight than most students realize.
Clerkship Grades & Honors: The New Academic Currency
The other big shift: core clinical performance now matters more than preclinical performance ever did.
Step 1 used to hide mediocre clinical stories. Not anymore. Committees pick your file apart in this order:
- Medicine
- Surgery
- OB/GYN
- Pediatrics
- Psych
- Family medicine (varies by specialty)
They look for patterns:
- Consistent Honors in core clerkships = strong signal
- Mostly High Pass with one or two Honors = acceptable for most fields
- Mostly Pass with no clear explanation = academic concern, especially for competitive programs
Here’s the mindset:
“If Step 1 is pass/fail, and Step 2 is one snapshot, how do we know if they can perform day after day? Look at their clerkships.”
I’ve watched internal medicine committees literally pull up the grade distribution from specific schools. Why? Because they know:
- Some schools give Honors to 15% of students.
- Some give Honors to 50–60%.
So a PD who knows School A vs School B will interpret “High Pass” very differently. That’s the quiet backchannel work they do now, instead of staring at a Step 1 column.
Two hidden factors with clerkship grades:
Surgery and IM comments are dissected.
The narrative sections matter more now. Words like “independent,” “trusted,” “calm under pressure” are gold.
Phrases like “with appropriate supervision” or “benefited from close guidance” are yellow flags when repeated.Timing of rotations.
If your weaker grades are early and stronger grades come later, committees are more forgiving, especially if your Step 2 trend matches that upward trajectory. If the opposite is true, it raises eyebrows.
Letters & SLOEs: “Who Wrote It” Now Matters Almost More Than “What It Says”
When Step 1 was numeric, a PD could justify an interview on that score alone. Those days are gone. Letters stepped into that gap—but only the right letters from the right people.
Here’s the part students don’t see. During selection meetings, faculty say things like:
- “Oh, that’s a Dr. X letter. She is tough. If she says they’re good, they’re very good.”
- “This is from a community doc we’ve never heard of. I’m going to discount it.”
- “That PD is an easy grader. Their ‘outstanding’ is everyone else’s ‘fine.’”
So you’re not just being evaluated. Your letter writers are too.
For EM and a few other fields that use SLOEs, the shift has been brutal. SLOEs became functionally more important than Step 1 for many programs:
- Standardized SLOEs give side‑by‑side comparisons—exactly what Step 1 used to do.
- Committees flip to the global assessment section before they even look at your narrative.
- If you’re not in the top couple of tiers on those SLOEs, your odds at top programs plummet, no matter how good your generic narrative letter sounds.
Pay attention to this: vague, lukewarm letters hurt more now than they used to. A generic “hard-working, punctual, pleasant” with no concrete example is code for “not special.” In a pile of 1,000, “not special” is essentially a no.
Research: Now a Sorting Hat, Not Just “Nice to Have”
Research used to be a “nice bonus” for a lot of fields. In the pass/fail era, it quietly morphed into a differentiator, especially when Step 2 clusters applicants tightly.
Programs use research for three things:
Signal of interest in the field.
Derm with derm research. Ortho with ortho research. Anesthesia with anesthesia projects. It’s lazy but true: “They did research here, so they must actually want this.”Proxy for mentorship and network.
This is the hidden game. When your name is next to big institutions or famous faculty, committees notice.
“They worked in Dr. X’s lab? Let me text them.” That happens constantly in competitive specialties.Tie-breaker at the top.
Once you’re in the “we like them” pool, research can flip you from “maybe” to “yes.” Especially if you’ve presented nationally or published with recognizable groups.
Let me be blunt: a mountain of low-quality posters from random conferences does not carry the same weight as one or two serious, mentored projects with known faculty in the specialty. Committees know how easy it is to churn out fluff. They’re not impressed by numbers alone.
Professionalism & Red Flags: Hyper‑Sensitive, Post‑Pass/Fail
With one big objective metric gone, committees leaned harder into the risk-avoidance game.
Nobody wants the resident who:
- Needs remediation meetings
- Fights with nurses
- Disappears on call
So any hint of that in your file becomes magnified. What used to be a “concern” can now quickly become a “do not rank” with less buffer from a strong Step score.
Here’s what gets scrutinized far more than students expect:
- Leaves of absence without a clear, straightforward explanation
- Course or clerkship failures or repeats, especially in clinical years
- Unexplained gaps in training
- Documented professionalism incidents – even “minor” ones
Programs aren’t asking, “Can they score well?” anymore. They’re asking, “Will they finish our program without creating misery and paperwork?”
And yes, stuff you think is buried sometimes gets surfaced. Background chatter between schools, informal emails from faculty who know each other, “Do you know anything about this student?” That still exists. Especially in small specialties.
The New Holistic Review (The Real Version, Not the Brochure)
Everyone loves to say “holistic review” now. Let me decode what it actually looks like at many places in the Step 1 pass/fail era:
- Auto-filter by Step 2 CK and sometimes school.
- Among survivors, sort by:
- Core clerkship performance
- Known institutions / letter writers
- Research, if the specialty cares
- Only after this slicing: look at personal statement, extracurriculars, and unique life story… for the top ~20–40% of that smaller pool.
That’s the real “holistic” order of operations. Not the pretty version on the department website.
What’s changed versus the old days is this: if your numbers are not elite, you’re not automatically dead if the story, letters, and clerkship trajectory create a coherent, compelling picture. There is slightly more room for late bloomers and nontraditional applicants—if they can still prove competence with Step 2 and clinical work.
But do not confuse “more holistic” with “less competitive.” It’s more chaotic. More dependent on networks and subtle signals. And less forgiving of sloppiness.
Strategy: How You Play This New Game
You can’t wish Step 1 back into existence. The game changed. You adapt or you get filtered.
If I had to give you a sharp, prioritized strategy in this era:
Crush Step 2 CK.
Take it when you’re ready, not early for ego. Build your calendar around it. In many specialties, it’s now the single most actionable number in your file.Maximize Medicine and Surgery clerkships.
Treat them like high-stakes auditions. Because they are. Those grades and narratives are now front-page material for committees.Curate your letters like your life depends on it.
Because, professionally, it does. Choose writers who actually know you, are known in the field, and will write specific, strong narratives. Ask residents quietly who writes “real letters” versus generic paragraphs.If you’re aiming competitive, get field-specific research at a place with a name.
Not just any project. Aim for known mentors, collaborators who present nationally, groups that your target programs recognize.Clean file, clear explanations.
If you have gaps, repeats, or LOAs, work out a concise, honest, non-dramatic explanation that frames growth and trajectory. Do not let committees have to “guess” what happened.

| Step | Description |
|---|---|
| Step 1 | ERAS Submitted |
| Step 2 | Step 2 Screen |
| Step 3 | School Name Proxy |
| Step 4 | Auto Reject |
| Step 5 | Academic Review |
| Step 6 | Clerkship Grades and MSPE |
| Step 7 | Letters and SLOEs |
| Step 8 | Research and Fit |
| Step 9 | Rank List Consideration |
| Step 10 | Step 2 CK Available |
| Step 11 | Above Internal Cutoff |
| Step 12 | Known Strong School |
| Step 13 | Invite to Interview |
FAQ: What Committees Now Scrutinize Instead of Step 1 Scores
1. If Step 1 is pass/fail, does my Step 1 performance matter at all?
Not numerically. Nobody sees your three-digit score anymore. But if you failed Step 1, committees will see that, and it absolutely matters. A single fail is a yellow flag that forces them to dissect Step 2, clerkships, and your explanation. A clean pass with no issues is mostly neutral now—just a box checked.
2. Should I delay Step 2 CK to improve my score, or will that hurt my chances?
If you’re on track to score solidly and can take it before applications are reviewed, do it early enough that the score is in ERAS. Many programs are hesitant to offer interviews without a Step 2 score. Delaying into late fall without a strong reason can quietly kill a big chunk of your opportunities, even if your eventual score is good.
3. How much do committees really care about the personal statement now?
They don’t use it to filter the bulk of applicants. It becomes relevant once you’re through the first cuts. At that stage, a thoughtful, specific statement can reinforce your story and help borderline files. A generic or sloppy one can hurt you. But no program is saying, “The scores are mediocre but the essay is so beautiful, let’s interview.” That’s fantasy.
4. Can strong research make up for a mediocre Step 2 score?
In ultra-competitive specialties, serious research with famous names can keep you in the conversation slightly longer—but it doesn’t erase a weak Step 2. Programs still have to trust you’ll pass boards. In less research-heavy fields, research is rarely powerful enough to compensate for a clearly low Step 2; it’s more of a bonus than a rescue.
5. I go to a lesser-known school. What can I do to compete now that Step 1 is pass/fail?
You have to overperform on everything you can control: Step 2 CK, core clerkships (especially IM/Surgery), and letters from recognizable names in the specialty. Away rotations at target programs matter more for you. So does getting into research or clinical experiences at better-known centers. You can’t change the school name in your header, but you can stack enough signals underneath it that a PD is forced to take you seriously.
Remember: In the pass/fail Step 1 era, committees did not get less selective—they just shifted their weapons. Step 2 CK, core clerkships, and letters from known people are the new battleground. If you’re smart, you stop wishing Step 1 still counted and start playing the game that actually exists.














