
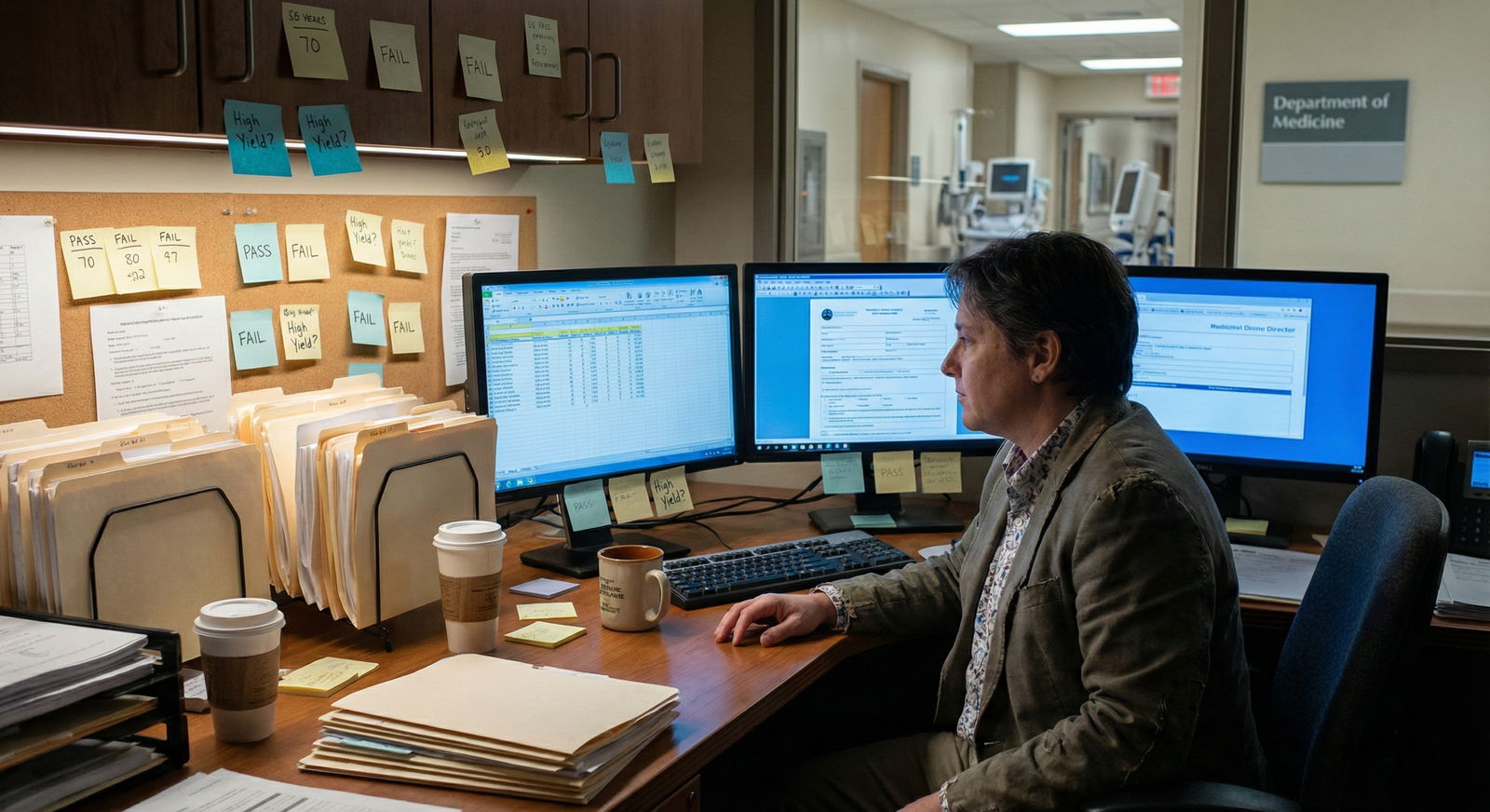
What happens when programs can no longer use Step 1 scores to filter you… but your digital footprint, professionalism, and patterns of behavior are still wide open?
Step 1 going pass/fail did not make residency selection kinder. It made it more opaque. Programs did not suddenly become holistic saints. They just shifted what they watch for.
And a lot of applicants are walking straight into new red flags they do not even know exist.
You are in the Step 1 pass/fail era. That means:
- Your “number” is gone.
- Your patterns are now the metric.
- The lazy belief that “Pass on Step 1 = I’m safe” is going to quietly sink people.
Let me walk you through the mistakes I keep seeing. The ones that get whispered about on Zoom selection meetings instead of shouted in score cutoffs.
1. Assuming “Pass = I’m Fine” While Everything Else Falls Apart
The worst mindset I see now: “Step 1 is pass/fail, pressure’s off, I can relax.”
No. What actually happened is this:
Programs lost a crude, easy filter. So they are making you prove competence in harder ways:
- Step 2 CK performance
- Clinical performance
- Consistency over time
- Evidence you can handle complexity without crumbling
If you treat Step 1 as a low bar and coast, you create a different kind of red flag: trajectory mismatch.

| Category | Value |
|---|---|
| Step 2 CK | 90 |
| Clerkship evals | 80 |
| Letters of rec | 75 |
| Professionalism record | 70 |
| Research/Projects | 60 |
These are the patterns that now scare committees:
- “Barely passed Step 1” followed by “Mediocre or late Step 2 CK”
- Step 1 pass + multiple marginal clerkship grades
- Step 1 pass + no meaningful clinical engagement or initiative
Here is the quiet thought a PD has:
“If this student underperformed when the stakes were high but visible, how will they perform when patients are on the line and no one is handing them a curve?”
Avoid this mistake:
- Treat Step 1 as the foundation of your knowledge, not a checkbox.
- Build a Step 2 CK plan before you even get your Step 1 result.
- Do not let your study discipline collapse the second you see “Pass”. You are setting up your own red flag six months later.
2. Weak or Toxic Clinical Evaluations: The New “Below 220”
In the old world, an ugly Step 1 score was an obvious red flag. Now the red flags are buried in your evaluations, but they carry just as much weight.
I have heard exact phrases in rank meetings:
- “Great CV, but his evals repeatedly mention being late and not receptive to feedback.”
- “This one worries me—three different attendings said ‘needs to work on reliability.’”
Programs are hunting for behavioral patterns, not one-off comments. Here is what quietly kills your application:
- Repeated notes about poor reliability
- “Needs improvement” in teamwork or communication across more than one clerkship
- Comments suggesting entitlement, defensiveness, or lack of insight
- A long chain of “meets expectations” with nothing standing out
Avoid this mistake:
- Ask early and specifically for feedback: “What’s one thing that would make me more useful to the team tomorrow?” Then actually implement it the next day.
- Treat every rotation like an audition, because it is. Not just for that specialty. Your narrative follows you.
- If you get mixed feedback on one rotation, do not shrug. Fix the behavior immediately before it becomes a trend across services.
Programs forgive one weird evaluation. They do not forgive a pattern of the same problem written in five different voices.
3. Mediocre or Late Step 2 CK: The New High-Stakes Number
Step 2 CK used to be an afterthought for many specialties. Not anymore.
Now, when committees cannot see Step 1 scores, they lean aggressively on Step 2 CK to answer one question:
“Can this person handle complex medical decision-making at the level our residents need?”
Let me be blunt:
- A low Step 2 CK in the pass/fail Step 1 era looks worse than the same score would have looked before.
- Late Step 2 CK scores are increasingly treated as risk signals, especially if your school is known for giving grade inflation.

| Category | Value |
|---|---|
| Screening cutoff | 65 |
| Tiebreaker | 25 |
| No impact | 10 |
Common self-sabotage behaviors:
- Scheduling Step 2 CK too close to application season “just in case I need time” and then needing that time
- Underestimating its difficulty because “I passed Step 1, I’ll be fine”
- Not doing enough quality question banks or full-length practice tests
Avoid this mistake:
- Aim for Step 2 CK to be your academic calling card.
- Schedule it with enough buffer to retake if something catastrophic happens.
- Treat your clinical year as Step 2 CK prep—actively reason through every case, not just carry orders.
A solid Step 2 CK can neutralize suspicion about a borderline Step 1 pass. A weak Step 2 CK does the opposite.
4. Personal Statements and ERAS Applications That Scream “Red Flag” Without You Realizing
You think red flags are about scores. Programs know they also live in your words.
I have read personal statements that quietly destroy a candidate’s chances in a single page.
Patterns that scare faculty:
Victim narrative with no growth.
“The school was unfair”… “I did poorly because other people sabotaged me”… “the system is broken.” Everyone knows the system is flawed. What they want to see is what you did despite that, not why you are powerless.Over-sharing trauma with no boundaries.
Disclosing severe mental health crises without any clear stabilization or ongoing support plan makes programs worry (fairly or unfairly) about reliability under stress.Grandiosity disconnected from record.
A 215 Step 2 CK, average clinical comments, and then a statement about “revolutionizing surgery” across continents. That cognitive dissonance sets off alarms.Explaining away every weakness.
One sentence acknowledging a rough period is human. Two paragraphs litigating your preclinical grades reads as defensive and exhausting.

Avoid this mistake:
- Have at least one brutally honest mentor read your personal statement and ERAS entries with one job: circle anywhere you sound like a victim, a hero, or a martyr.
- Treat explanations like medication: minimum effective dose. One clear paragraph, then move on.
- Write like someone who knows medicine is hard and is prepared to share responsibility, not assign blame.
Programs are not looking for perfection. They are looking for people who can identify their own weaknesses without collapsing into self-justification.
5. Professionalism Lapses: Emails, Social Media, and “Small” Incidents
Here is where applicants are getting blindsided in the post-Step 1 world: your unforced errors matter more now, because there is less objective data to hide behind.
I have personally seen these sink or seriously harm applications:
- Emailing program coordinators with rude, demanding, or entitled language
- No-showing for an interview or canceling last-minute with a flimsy excuse
- Social media posts that mock patients, share protected information, or trash talk specific programs or faculty
- Repeated lateness or disappearing during away rotations
| Behavior | Why Programs Care |
|---|---|
| Late or rude email responses | Predicts poor communication |
| No-shows for meetings/interviews | Signals unreliability |
| Gossip or complaints on social | Risk to team culture and patients |
| Disrespect to staff | Bad teammate, hard to remediate |
Selection meetings are full of comments like:
- “Her application is good, but our coordinator said she was very difficult during scheduling.”
- “He was 20 minutes late to the interview and didn’t apologize.”
Avoid this mistake:
- Treat every email, phone call, and Zoom like part of your application file. Because it is.
- If something goes wrong (illness, emergency), communicate clearly, briefly, and with ownership. No long stories, no drama.
- Clean up your public social media. Today. Anything that would look childish, arrogant, or cruel under a program director’s eyes should be gone.
You will not be rejected for a single awkward email. But you can absolutely be ranked lower for looking high-maintenance before you even show up.
6. Letters of Recommendation That Quietly Say “No Thanks”
In the pass/fail era, letters have become much more powerful filters. Programs are reading them more carefully because they are trying to reconstruct the missing score story.
Here are the red-flag signals inside letters that you probably will not see, but they will:
“I recommend this student for a residency position.”
Translation: minimal enthusiasm. Not a disaster, but not a strong yes.No specific anecdotes. Just generic praise.
Signals that you did not stand out or the writer barely remembers you.Damning faint praise:
“She completed all her responsibilities.”
“He was appropriate on the wards.”Inconsistency between your personal narrative and the letter.
You claim to be deeply committed to underserved care, but your letter from that free clinic rotation barely mentions it.

| Category | Value |
|---|---|
| Generic praise | 20 |
| Mildly positive | 40 |
| Strong rec | 75 |
| Enthusiastic must-hire | 95 |
Avoid this mistake:
- Ask for letters only from people who know you well and can speak to specific behaviors: work ethic, team skills, clinical reasoning.
- When you ask, say this out loud: “Do you feel you can write me a strong letter of recommendation?” If they hesitate, walk away.
- Give them a short summary of your work with them and concrete things you did, so they have material beyond clichés.
A single lukewarm letter will not necessarily sink you. But three “meh” letters in a world without Step 1 numbers? That is your new 208.
7. Gaps, Leaves, and “Mystery Time” With No Coherent Story
Life happens during medical school. Illness. Family crises. Burnout. I am not telling you to hide that.
The mistake is thinking, “If I do not mention it, maybe no one will notice.” They will. Then they will fill in the blanks with the worst possible version.
Common red-flag patterns:
- Unexplained gaps in enrollment or between clinical years
- Multiple LOAs without a single clear, cohesive explanation
- Dramatic drop in performance (grades, Step 2 CK, professionalism issues) during a specific year with zero context

| Step | Description |
|---|---|
| Step 1 | See unexplained gap |
| Step 2 | Assume instability or professionalism issue |
| Step 3 | Assume ongoing risk |
| Step 4 | Assess recovery and support |
| Step 5 | Any explanation? |
| Step 6 | Coherent and concise? |
Avoid this mistake:
Work with your dean’s office on an official summary that is honest but bounded. You want:
- Brief cause (e.g., health issue, family responsibilities)
- Clear resolution or current management
- Evidence of successful return to full function
In your application, do not turn it into a drama essay. One paragraph in the “additional information” section is usually enough.
Programs are not allergic to adversity. They are allergic to unpredictability. Show that your difficult period has a clear before, during, and after.
8. Away Rotations and Virtual Interactions That Backfire
Away rotations used to be “auditions.” They still are—but now, for many, they are also the only direct look a program gets at you as a person, since test scores are so flat.
Red flag behaviors on aways:
- Acting like you are competing against the residents instead of joining their team
- Being “on” for attendings but dismissive to nurses, techs, and coordinators
- Vanishing when there is scut work or staying passive in conference
- Overcompensating: too many questions, forced enthusiasm, fake familiarity

Virtual interactions count just as much:
- Logging into virtual interviews from messy, chaotic environments
- Poor eye contact, multitasking, or obviously reading off notes
- Sounding disinterested or burned out
Avoid this mistake:
- On aways: pick one main goal—be the most reliable, low-drama, helpful student on the team. Not the smartest. Not the funniest. The one no one has to worry about.
- For virtual interviews: treat your setup as clinical. Quiet background, decent lighting, tested audio, zero distractions.
A strong away rotation can erase a lot of doubt in the pass/fail era. A bad one sticks in the committee’s memory far longer than a single test score ever did.
9. The Overall Pattern That Programs Now Look For
You keep hearing “holistic review” like it is some warm, fuzzy concept. It is not. It is a pattern-recognition exercise.
Without Step 1 scores, committees are essentially asking:
- Do your knowledge markers line up? (Step 2 CK, school reputation, honors)
- Do your behavioral markers align? (evals, professionalism, interviews)
- Do your narrative markers make sense? (personal statement, letters, gaps)
If those three domains tell the same story—“steady, improving, teachable, reliable”—you are fine. If they conflict, that is the new red flag.
The biggest mistake now? Focusing obsessively on one domain (usually scores) and ignoring the others. That was risky before. It is suicidal now.
FAQ (Exactly 4 Questions)
1. If I barely passed Step 1, am I basically doomed in competitive fields now that it is pass/fail?
No, but you have zero margin for additional question marks. A borderline Step 1 pass puts pressure on you to deliver a strong Step 2 CK, excellent clinical evaluations, and clearly positive letters. You cannot afford professionalism hiccups, unfocused personal statements, or weak aways. Programs will forgive a shaky preclinical exam history if your later trajectory screams “ready and reliable.” They will not forgive a pattern of “barely enough” across everything.
2. Should I explain a low Step 1 or just let the pass/fail label speak for itself?
If your school or transcript hints at a struggle (remediation, extended curriculum, LOA), then yes, give a short, honest explanation. One paragraph. Own what happened, state what changed, and show the proof that you are now stable and effective (Step 2 CK, clinical honors, strong letters). If your record is otherwise clean and there is no visible disruption, you do not need to invent an explanation. Do not turn a quiet footnote into the main story.
3. How many professionalism “incidents” does it take to really hurt my application?
One serious incident, if documented, can follow you for years. But more commonly, it is the accumulation of “small” things that does the damage: chronic lateness, poor email tone, unreliable follow-through, friction with staff. Two or three independent mentions of similar behavior in evaluations, dean’s letters, or coordinator feedback create a powerful negative pattern. Your goal is simple: if you mess up once, correct it aggressively and visibly so it never recurs in another context.
4. What is the single most protective thing I can do right now in the pass/fail Step 1 era?
Align your behavior with the story you want your application to tell. If you want to be seen as steady and improving, act that way: consistent work habits, early Step 2 CK prep, active engagement on the wards, respectful communication, and thoughtful self-reflection in your personal statement. Today, open your latest clinical evaluation and identify one piece of constructive criticism in it. Then write down exactly how you will show evidence over the next two weeks that you are fixing that issue. That conscious correction is what committees are quietly rewarding now.
Open your ERAS or CV draft right now and scan each section for one thing: does anything on the page contradict the kind of resident you claim you will be? If the answer is “maybe,” fix that first—before a program quietly tags it as your new red flag.














