The Do's and Don'ts of Applying for U.S. Clinical Experiences as an IMG
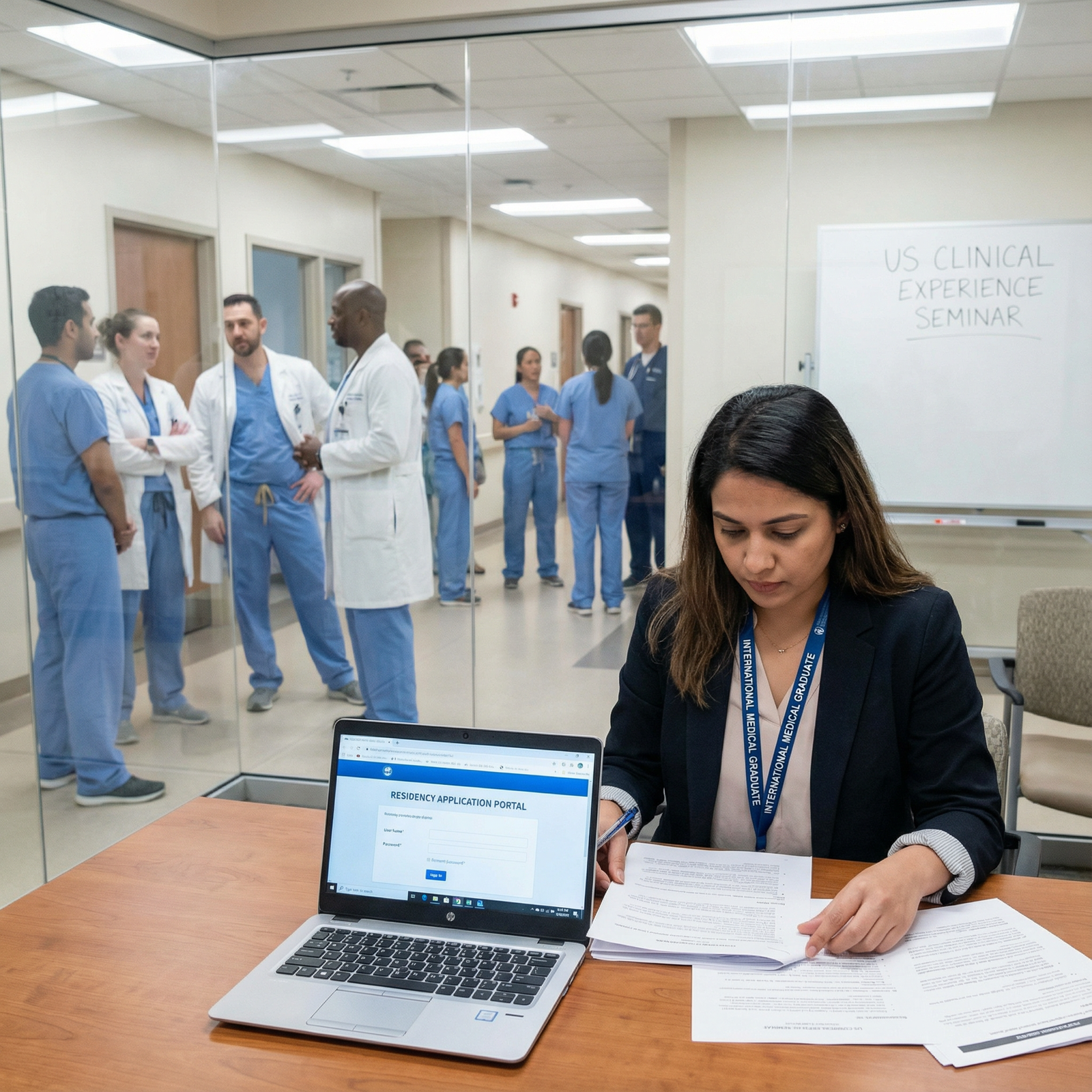
International Medical Graduates (IMGs) face a distinct mix of challenges and opportunities in the world of U.S. medical education and practice. One of the most strategic steps in your journey is securing U.S. clinical experience—whether through observerships, externships, electives, research rotations, or volunteer clinical roles.
These experiences do far more than fill a line on your CV. They can transform your understanding of the U.S. healthcare system, strengthen your residency applications, and jump-start your long-term career development in medicine. But the way you apply—and how you present yourself—matters just as much as the experience itself.
This enhanced guide walks through the critical do’s and don’ts of applying for clinical experiences as an IMG, with practical, step-by-step advice to help you avoid common pitfalls and position yourself for success.
Why U.S. Clinical Experience Matters for IMGs and Residency Applications
Before you invest time, money, and energy in applications, it’s essential to understand why U.S. clinical experience is so heavily valued in residency applications—and how to choose experiences that truly help you.
Understanding the U.S. Healthcare System in Real Time
- System differences: The U.S. healthcare system is complex—insurance-driven, multidisciplinary, and highly protocol-based. Even if you trained in a high-resource setting abroad, the workflows, documentation, and medico-legal environment will likely be very different.
- Electronic Medical Records (EMR): Most U.S. institutions use EMRs extensively. Exposure to EMR workflows (even in observer roles where you cannot enter orders) signals that you can adapt quickly.
- Team-based care: Clinical experience helps you understand how teams interact—attendings, residents, fellows, advanced practice providers, nurses, pharmacists, social workers, and case managers. This understanding is crucial for successful U.S. medical education and residency performance.
Building Networks and Strong Letters of Recommendation
- Mentorship and sponsorship: Rotations let you form real relationships with attendings and residents who can advise you on specialty choice, study strategy, and applications.
- U.S. Letters of Recommendation (LoRs): Many residency programs strongly prefer or require LoRs from U.S. clinicians who know your clinical abilities, work ethic, and professionalism. High-quality U.S. clinical experience is one of the best ways to earn these letters.
- Future connections: A good impression can lead to research collaborations, interview tips, informal advocacy during rank meetings, or even direct program recommendations.
Demonstrating Clinical Skills and Professionalism
- Clinical reasoning in the U.S. context: Even in observerships (where hands-on work is limited), discussions during rounds and case presentations allow you to demonstrate your reasoning and communication.
- Professionalism and reliability: Showing up prepared, on time, and engaged signals that you will be a safe and effective resident.
- Cultural and communication competence: U.S. programs need to know that you can communicate effectively with diverse patient populations and multidisciplinary teams.
Strengthening Your Residency Application Competitively
U.S. clinical experience is a key differentiator for International Medical Graduates because it:
- Shows you are serious about practicing in the U.S. and have invested in understanding the system.
- Helps explain any gaps or transitions in your application (e.g., time since graduation spent in U.S. clinical or research experience).
- Allows you to tailor your personal statement and interviews with concrete examples of patient care scenarios in U.S. settings.
The Do’s of Applying for U.S. Clinical Experiences as an IMG
Do Thorough, Strategic Research
Many IMGs start by googling “U.S. clinical observerships” and applying randomly. That approach wastes time and money. Instead, be deliberate.
Understand Types of U.S. Clinical Experiences
- Observerships: You observe but generally do not provide direct patient care or write notes/orders. Often the most accessible type of experience for IMGs after graduation.
- Externships / hands-on experiences: More structured roles that may allow supervised patient interaction, notes, and case presentations. These are often most valuable for LoRs but may be harder to secure and sometimes costly.
- Electives (for current students): If you are still in medical school, 4th-year electives at U.S. academic centers are often considered the gold standard of experience.
- Research rotations: While not purely clinical, clinical research positions at U.S. hospitals can give hospital exposure and relationships with faculty who also work clinically.
- Volunteer/clinic roles: Free clinics, community health centers, and health fairs can demonstrate commitment to patient care and adaptability.
Target Programs That Align With Your Goals
Before applying, ask yourself:
- What specialty am I realistically targeting (e.g., internal medicine, family medicine, pediatrics, psychiatry)?
- What kind of experience will be most persuasive for those fields?
- Do I need academic vs community exposure—or both?
Use sources such as:
- ECFMG and AMA websites
- Individual hospital and university department pages (often under “Education” or “International Programs”)
- IMG-focused organizations and forums (but verify all information)
- Your own network: alumni from your medical school who matched in the U.S.
Document your research in a spreadsheet:
- Program name, contact, requirements, fees, deadlines, eligibility (e.g., years since graduation, USMLE status), and application materials needed.
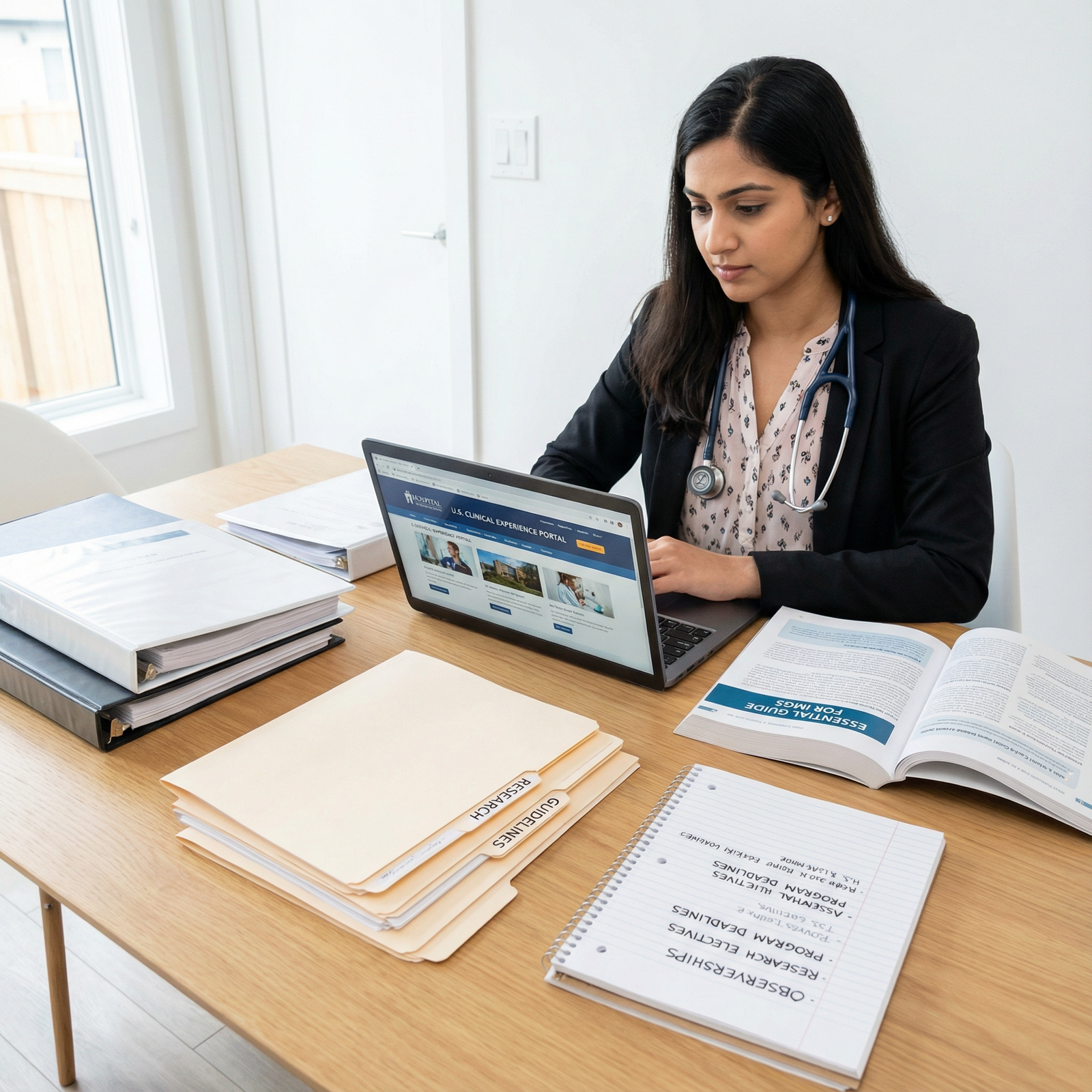
Do Build a Competitive, U.S.-Style CV and Application Package
Your CV, personal statement (if requested), and emails form your first impression. Treat them with the same seriousness as a residency application.
Highlight Relevant Clinical and Academic Experience
- Place clinical experience high on your CV, especially anything that shows responsibility, leadership, or continuity of care.
- Include:
- Rotations and internships, with key duties and patient populations
- Research projects, publications, and presentations
- Teaching or tutoring experience (demonstrates communication and professionalism)
- Volunteer work, especially in healthcare contexts
- For each entry, briefly describe your role and skills gained, not just titles and dates.
Tailor Materials to Each Program
Avoid generic, copy-paste statements. Instead:
- Emphasize what you can contribute to that setting: e.g., language skills, experience with similar patient populations, or background in public health.
- Clarify what you hope to learn: e.g., managing chronic disease in resource-rich settings, working with EMRs, U.S. style of documentation and handoffs.
- If the program emphasizes underserved care, research, or primary care, highlight experiences that match those priorities.
Do Network Early and Intentionally
Networking is not about asking for favors; it’s about building genuine professional relationships.
Use Multiple Professional Channels
- LinkedIn: Update your profile to reflect your U.S. career goal. Connect with:
- Alumni from your school in U.S. training
- Physicians in your target specialty
- Former observers or research fellows at your target institutions
- Conferences and webinars:
- Attend virtual and in-person specialty conferences.
- Ask thoughtful questions and follow up with speakers or panelists by email.
- Institution-based connections:
- If your medical school has a partnership with a U.S. institution, leverage it.
- Contact international offices or graduate medical education offices for structured opportunities.
Seek Mentors, Not Just Opportunities
A good mentor can:
- Help you refine specialty choices based on your academic profile.
- Recommend programs or specific attendings open to working with IMGs.
- Review your CV and emails for U.S.-style expectations.
- Potentially open doors to clinical or research roles later.
Do Prepare Thoroughly for Interviews and Initial Interactions
Some programs will formally interview you; others may simply schedule an introductory call or email exchange. Treat all of these as professional interviews.
Practice Common Clinical and Behavioral Questions
Prepare to discuss:
- Your medical education and clinical strengths.
- Why you want U.S. clinical experience and how it fits your career development.
- Cases that challenged your clinical reasoning, communication, or ethics.
- How you respond to feedback, manage stress, and work in a team.
Practice with:
- Peers also applying for U.S. experiences.
- Residents, fellows, or faculty mentors who know the U.S. system.
- Mock interviews—record yourself and adjust your communication style.
Demonstrate Professionalism in Every Detail
- Test your internet connection and audio if the interview is virtual.
- Dress professionally (even for Zoom).
- Be punctual—log in 10–15 minutes early.
- Follow up with a brief, specific thank-you email that references something you learned about the program.
Do Follow Up and Maintain Relationships
Your relationship with a program or physician does not end with a single application or rotation.
- Post-interview: Send a concise thank-you email within 24–48 hours.
- After rejection or waitlisting: Consider a polite note expressing continued interest or asking if there are future opportunities or ways to strengthen your candidacy.
- After a rotation: Stay connected with attendings through:
- Occasional updates (e.g., exam success, other achievements)
- Holiday greetings or short notes expressing gratitude for their mentorship
- Requests for advice when applying to residency
Long-term relationships can lead to research projects, future rotations, or stronger LoRs.
The Don’ts of Applying for U.S. Clinical Experiences as an IMG
Understanding what to avoid can save you from damaging your reputation or wasting time and financial resources.
Don’t Rush or Mass-Apply Without Strategy
It is tempting to send the same email or application to dozens of programs within a day. This approach is often counterproductive.
Avoid Generic, Low-Quality Applications
- Coordinators and attendings quickly recognize mass emails.
- Mistakes such as using the wrong program name, wrong specialty, or poor formatting can lead to immediate rejection.
- Instead, set a weekly target (e.g., 5–10 well-researched applications) and ensure each one is individually tailored.
Don’t Ignore Red Flags
If a “program”:
- Has no clear affiliation with a hospital or university,
- Requests large upfront fees without transparency,
- Makes unrealistic promises like “guaranteed residency”,
then step back and research more. Reputable programs focus on education, not guaranteed outcomes.
Don’t Ignore Legal, Visa, and Compliance Requirements
Even the best application will fail if you cannot legally participate in the experience.
Understand Visa and Status Requirements
- Check whether the program accepts:
- B1/B2 visas (many observerships do),
- J-1 or F-1 visas,
- Or requires particular visa statuses.
- Clarify:
- Whether they provide documents to support your visa application.
- How long you are allowed to stay for the rotation.
Always allow enough time—often several months—for visa processing.
Keep Certifications and Credentials Updated
Programs may require:
- BLS and/or ACLS certifications from recognized organizations (e.g., American Heart Association).
- ECFMG certification status, or at minimum certain USMLE steps completed.
- Immunization records, titers, TB testing, and sometimes drug screening.
- Background checks or health clearance from occupational health.
Ignoring or delaying these can cause you to lose a spot even after acceptance.
Don’t Be Unprofessional or Disrespectful
Your behavior during application and after can spread quickly through networks—positively or negatively.
Avoid Inappropriate or Casual Communication
- Use professional language, proper salutations, and a clear subject line.
- Don’t send multiple follow-up emails in a short time; wait at least 1–2 weeks before a polite inquiry.
- Never complain about prior rejections, coordinators, or other programs in your communication.
Never Burn Bridges
Even if you are rejected:
- Send a polite thank-you for their time and consideration.
- Ask if you can reapply in the future or if they can recommend similar programs.
- Remember: today’s rejection could be tomorrow’s opportunity if you leave a positive impression.
Don’t Underestimate Cultural and System Differences
Technical knowledge alone is not enough; cultural competence is a core part of U.S. clinical training.
Be Open to Different Communication Styles and Hierarchies
- U.S. teams may encourage trainees to ask questions and challenge ideas respectfully. This may differ from more hierarchical systems.
- Shared decision-making with patients is emphasized; you may need to adjust how you explain risks, benefits, and options.
Respect Diversity and Inclusion Norms
- You will encounter patients from varied backgrounds in terms of race, ethnicity, language, gender identity, sexual orientation, and socioeconomic status.
- Avoid assumptions. Ask open-ended questions about preferences and beliefs.
- Familiarize yourself with U.S. patient privacy rules (HIPAA) and boundaries in patient–provider interactions.
Don’t Give Up Too Soon—or Let Gaps Go Unexplained
Many successful IMGs faced multiple rejections before securing strong clinical experiences.
Expect Setbacks and Learn from Them
- Track your applications and outcomes.
- After multiple rejections, ask a mentor to review your CV, emails, and strategy.
- Adjust your target programs if needed—consider starting with community programs or smaller cities, then building up to more competitive centers.
Use Alternative Paths When Needed
If you cannot immediately secure a formal clinical experience:
- Seek volunteer roles in clinics, health fairs, or community health organizations.
- Look for research assistant positions in departments related to your desired specialty.
- Use online case-based learning, U.S. guideline review, and EMR tutorials to stay clinically sharp.
These can fill gaps and demonstrate ongoing commitment to career development and patient care.

Practical Tips to Maximize the Value of Your U.S. Clinical Experience
Securing the position is only half the battle; how you perform matters even more.
Be Prepared Before Day One
- Review common U.S. abbreviations, documentation styles, and note templates.
- Refresh core topics in your target specialty using U.S. guidelines (e.g., ACC/AHA, USPSTF, IDSA).
- Understand basic hospital etiquette: when and how to page, how rounds are structured, and expectations around HIPAA/privacy.
Behave as if You’re Already a Resident—Within Your Role’s Limits
- Be punctual every single day.
- Show initiative: pre-read about patients, research questions, and volunteer for presentations.
- Ask for feedback and incorporate it visibly.
- Always stay within the scope of your allowed duties; never perform clinical tasks you are not authorized or competent to do.
Intentionally Work Toward Strong Letters of Recommendation
- Identify attendings who have directly observed your work and can comment on your:
- Clinical reasoning,
- Work ethic,
- Communication skills,
- Professionalism.
- Near the end of the rotation:
- Politely ask whether they feel they know your work well enough to write a strong letter.
- Provide your CV, personal statement draft, and a summary of your goals.
- Maintain contact and update them when you begin your residency applications.
FAQ: Applying for U.S. Clinical Experiences as an IMG
1. What are the most valuable types of U.S. clinical experience for International Medical Graduates?
For residency applications, experiences that involve close interaction with U.S. physicians and real patient care are most valuable. For current students, final-year clerkships or electives at U.S. academic centers are ideal. For graduates, well-structured externships or observerships in your target specialty—especially at programs that also sponsor residencies—are highly beneficial. Research positions in clinical departments can also be powerful if they lead to publications and mentorship from U.S. faculty.
2. Is U.S. clinical experience absolutely required for residency applications as an IMG?
Not all programs list it as an explicit requirement, but many strongly prefer U.S. clinical experience. It can be especially important if:
- You graduated more than a few years ago,
- You are switching specialties,
- Your home-country training environment differs significantly from the U.S.
At minimum, some exposure helps you speak convincingly in interviews about U.S. healthcare, and it enables you to secure U.S.-based Letters of Recommendation, which many programs consider essential.
3. How can I financially plan for U.S. clinical experience as an IMG?
Costs can include application fees, program tuition, visa expenses, travel, housing, and daily living. To manage this:
- Research low- or no-cost hospital-based observerships (often at teaching hospitals with formal IMG programs).
- Look for scholarships or small grants offered by IMG organizations, alumni associations, or charitable foundations.
- Consider staying with relatives or friends in the U.S. to reduce accommodation costs.
- If already in the U.S. on a visa that permits work, consider part-time, non-clinical work that does not violate visa rules. Always confirm eligibility with an immigration advisor.
4. How long should U.S. clinical experiences last to be meaningful on a residency application?
Programs often value depth over sheer number of short experiences. A common pattern is:
- 1–3 months in your target specialty at one or two institutions, plus
- Additional shorter observerships or research experiences if possible.
Even a 4-week rotation can be valuable if you are consistently present, engaged, and able to develop a meaningful relationship with an attending who can later write a detailed LoR.
5. Can I apply for U.S. clinical experiences while still in medical school, and how early should I start?
Yes. Many U.S. schools welcome final-year international medical students for electives. Ideally:
- Start researching 12–18 months before your desired rotation date.
- Check eligibility: some require that you be in your final year and have completed core rotations.
- Make sure your home institution approves the elective and that it doesn’t conflict with required coursework or exams.
Early planning gives you a better chance at your desired specialty, institution, and timing—especially if you want clinical experience that aligns with the upcoming residency application season.
Thoughtful planning, strategic applications, and professional behavior at every step can turn U.S. clinical experiences into a powerful foundation for your U.S. medical education, residency match, and long-term career development as an IMG.





















