
Why Backup Specialty Planning Matters for MD Graduates in Neurosurgery
For an MD graduate targeting neurosurgery, few topics are as emotionally charged—and as strategically important—as backup specialty planning. Neurosurgery remains among the most competitive fields, and even outstanding applicants from an allopathic medical school match pool face real uncertainty each cycle.
Thinking through a backup specialty or even dual applying residency strategies is not an admission of weakness; it is a hallmark of maturity and risk management. Your goal is to maximize your chances of training in a fulfilling career while giving yourself a genuine shot at a neurosurgery residency or brain surgery residency.
This article walks you through a structured, step-by-step approach to backup specialty planning specifically tailored to MD graduates in neurosurgery: how to assess your competitiveness, how to select realistic and satisfying plan B specialties, how to implement a dual-apply strategy, and how to communicate your intentions honestly and professionally.
Step 1: Understand the Risk Landscape in Neurosurgery
Before choosing a backup, you must have a clear-eyed understanding of neurosurgery match dynamics for an MD graduate residency.
Why Neurosurgery Is So High-Risk
Factors that make neurosurgery uniquely competitive:
- Limited number of positions compared to applicant volume
- Rigid training structure (7+ years, integrated, few prelim options)
- Heavy emphasis on neurosurgery-specific research and letters
- Programs favoring strong home or away-rotation performance
- High expectations for board scores, clerkship grades, and professionalism
Even among MD graduates from allopathic medical schools, strong applicants can end up unmatched due to sheer numbers, limited interview offers, or a poor interview season.
Key Competitiveness Indicators
As an MD graduate, you should analyze your objective and subjective profile honestly. Consider:
USMLE/COMLEX Performance
- Step 1 is now Pass/Fail but still matters indirectly (e.g., how quickly you passed, number of attempts).
- Step 2 CK remains a crucial discriminator.
- Below-average Step 2 CK for matched neurosurgery often pushes applicants toward serious backup planning.
Research Productivity
- Neurosurgery is research-heavy.
- Competitive applicants often have multiple neurosurgery-related publications, abstracts, and presentations.
- If your research is limited, not neurosurgery-focused, or very recent, that increases risk.
Clinical Evaluations and Honors
- Honors in surgery and neurology, strong Sub-I (acting internship) evaluations, and excellent professionalism comments are key.
- Any red flags (disciplinary action, professionalism issues, poor evaluations) significantly escalate risk.
Neurosurgery-Specific Mentorship and Advocacy
- Strong letters from neurosurgeons who are nationally known or strongly connected help open doors.
- If you lack advocates deeply embedded in neurosurgery networks, you may face a quieter interview season.
Application Cohesiveness
- A clear neurosurgery narrative: longitudinal involvement, leadership in neurosurgery interest groups, relevant research, and clear commitment.
- If your CV is diffuse or late-converting to neurosurgery, programs may perceive uncertainty.
When Backup Planning Becomes Essential
While everyone should at least think about it, robust backup specialty planning is especially critical if:
- You have a Step 2 CK score below the average for matched neurosurgery applicants.
- You have no neurosurgery home program or limited access to away rotations.
- You are internationally trained (IMG) but now holding an MD from a US allopathic bridge program.
- You carry any red flags (exam failures, remediation, professionalism concerns).
- You are geographically constrained or require a specific location.
If any of these resonate, you should treat backup planning as a parallel priority, not a last-minute patch.
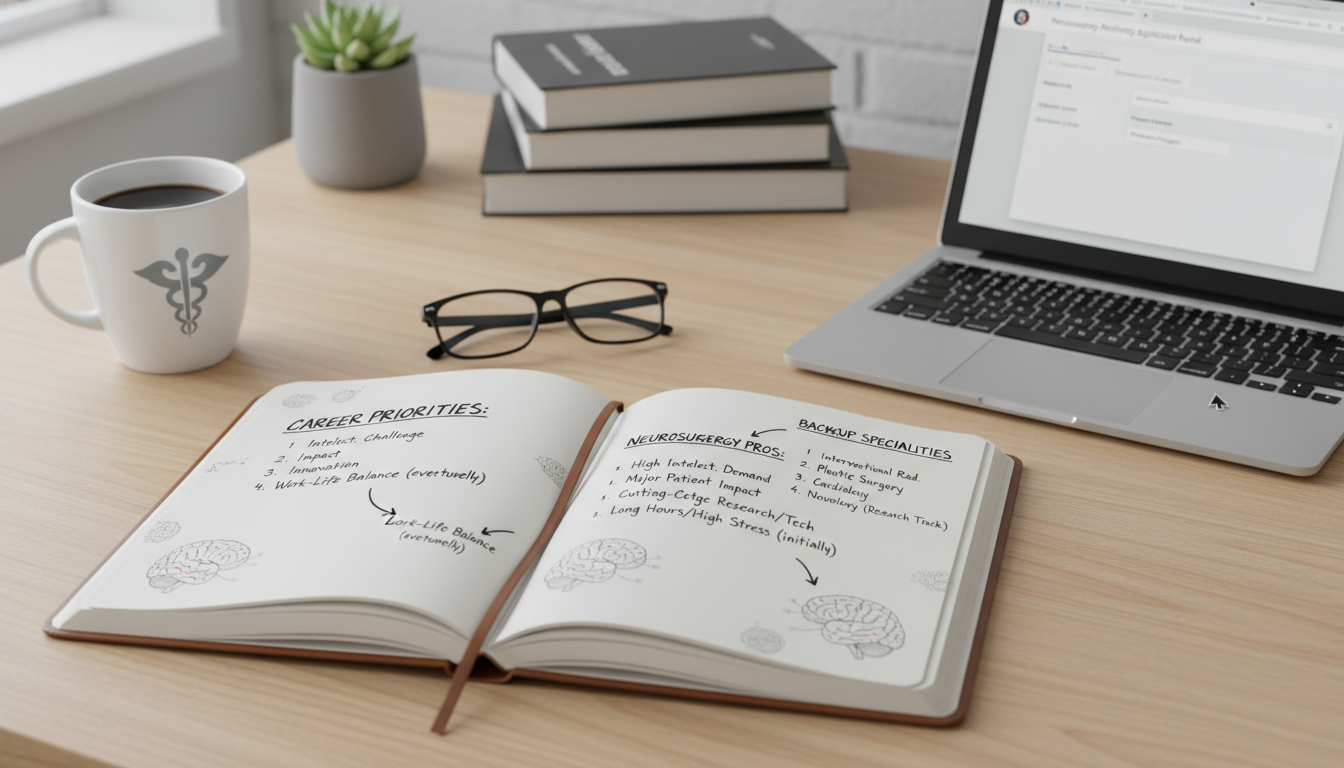
Step 2: Clarify Your Core Career Priorities
Backup specialty planning isn’t just about “what can I get into?”—it’s about “what can I live with for 30+ years?” You must translate your interest in neurosurgery into underlying attributes that drive your career satisfaction.
Identify What You Love About Neurosurgery
Commonly cited reasons MD graduates pursue neurosurgery include:
- Operating on the nervous system and direct, high-impact interventions
- Complex decision-making in critically ill patients
- Longitudinal patient relationships in some subspecialties (e.g., spine, functional neurosurgery)
- High-intensity, team-based hospital work
- Engagement with cutting-edge technology (stereotactic systems, intra-op imaging, neuromodulation)
Write down your top 3–5 elements that truly excite you about brain surgery residency training.
Example:
- High-acuity, OR-based care
- Complex anatomy and imaging
- ICU management and rapid decisions
- Long operative cases and technical challenges
These elements will guide your choice of a backup or plan B specialty that still aligns with your intrinsic motivations.
Identify Non-Negotiables and Flexibles
Consider:
- Lifestyle and work hours: Are you willing to accept another high-intensity field (e.g., general surgery) or do you want something more predictable?
- Procedural vs. cognitive work: Must you operate, or could you be fulfilled interpreting imaging or performing less invasive procedures?
- Patient population: Adult vs. pediatric, inpatient vs. outpatient, oncology vs. trauma, etc.
- Desired future flexibility: Would you be happy in academic practice, private practice, or both?
Classify each as:
- Non-negotiable
- Strong preference
- Flexible
This thinking helps prevent you from choosing a backup specialty that you match into but later resent.
Step 3: Choosing a Realistic and Satisfying Backup Specialty
The best backup specialty for a neurosurgery-focused MD graduate residency balances three things:
- Reasonably higher match probability than neurosurgery
- Genuine career fit based on your interests
- Strategic overlap in experiences, letters, and skills with your neurosurgery application
Common Backup Options for Neurosurgery Applicants
Below are frequently considered plan B specialty options, with pros, cons, and ideal applicant profiles.
1. Neurology
Why it fits:
- Strong overlap in neuroanatomy, neurophysiology, and neuroimaging
- Allows subspecialization (neurocritical care, epilepsy, stroke, neuromuscular, movement disorders)
- Offers opportunities to work closely with neurosurgeons in many settings
Pros:
- Often less competitive than neurosurgery, depending on program tier and geographic preference
- Your neurosurgery-related research may still be relevant (e.g., tumors, spine, functional outcomes)
- Familiar neurology rotations and letters are easier to obtain
Cons:
- Primarily a cognitive specialty; operative opportunities are extremely limited
- Workflow and lifestyle differ significantly from neurosurgery
- Some neurosurgery applicants may struggle with the shift away from the OR
Best suited for:
Applicants who love neurologic disease and complex diagnostic reasoning and can be satisfied focusing on medical management rather than surgery.
2. Diagnostic Radiology (with possible Neuroradiology focus)
Why it fits:
- Deep engagement with neuroimaging, cross-sectional anatomy, and technology
- Many neurosurgeons work closely with neuroradiologists in tumor boards and surgical planning
Pros:
- Generally more attainable than neurosurgery at a wide range of programs
- Intellectually rich and technology-heavy; strong lifestyle potential
- Your neurosurgery imaging research or anatomy background can be an asset
Cons:
- No direct surgery; patient interaction is often limited
- Requires comfort with long periods of desk/computer-based work
- Requires re-framing your personal brand from “surgeon” to “diagnostician”
Best suited for:
Applicants who enjoy imaging, anatomy, and pattern recognition, and who value a more controllable lifestyle in the long-term.
3. Anesthesiology (with potential Neuroanesthesia focus)
Why it fits:
- Continued work in the OR, including neurosurgical cases
- Involvement in critical care, physiology, and perioperative medicine
Pros:
- Many programs have neuroanesthesia fellowships, keeping you close to neurosurgical cases
- Procedural, acute care, team-based environment
- Broader number of positions across the country
Cons:
- Different professional identity and scope compared to operating surgeon
- Less direct ownership of surgical decision-making and post-op management
Best suited for:
Applicants who prioritize operating room environment, procedures, and acute physiology over being the primary surgeon.
4. General Surgery (with possible later subspecialization)
Why it fits:
- Still a surgical career with complex operative cases
- Potential to sub-specialize (surgical oncology, vascular, trauma) in areas of high acuity
Pros:
- You maintain a surgeon identity
- Some surgical programs are less competitive than neurosurgery, though top-tier general surgery remains selective
Cons:
- Long hours and demanding lifestyle can rival neurosurgery
- Training path may be equally lengthy (5+ years plus fellowship)
- Less overlap with neurosurgery-specific research unless you have broader surgery projects
Best suited for:
Applicants committed to being in the OR above all, and who are open to other complex surgical fields if neurosurgery is not an option.
5. Physical Medicine & Rehabilitation (PM&R) with Neurorehab
Why it fits:
- Neurorehab focus allows continued engagement with stroke, spinal cord injury, traumatic brain injury
- Longitudinal care and functional outcomes in neurologic patients
Pros:
- Generally more accessible than neurosurgery
- Allows strong patient relationships and interdisciplinary team leadership
- Better lifestyle in many practice settings
Cons:
- Very different from intra-operative surgical work
- Focus is on function and recovery, not on primary surgical intervention
Best suited for:
Applicants drawn to neurorecovery, disability, and functional medicine, with less emphasis on acute operative care.
How to Narrow to One or Two Backup Choices
To avoid diluting your application, you should typically identify:
- One primary backup specialty (e.g., neurology or radiology)
- Possibly one secondary, compatible backup if your risk is very high
Use these filters:
- Fit with your core priorities (from Step 2)
- Geographic flexibility: More flexible applicants can target a wider range of programs in their backup field.
- Overlap in your existing experiences: Choose a field where your current CV can be reframed effectively without starting from zero.
Step 4: Structuring a Dual Applying Residency Strategy
Dual applying means applying simultaneously to neurosurgery and at least one backup specialty. For an MD graduate in neurosurgery, this can be logistically complex but highly protective.
Decide Early: Single vs. Dual Application
Ask yourself:
- Does my competitiveness profile suggest I can reasonably match into neurosurgery without a backup?
- If not, am I willing to invest extra time and money into two strong applications rather than one mediocre one?
In many cases—especially if you are not in the top tier of applicants—dual applying residency is a rational safeguard.
Application Logistics for Dual Applying
ERAS Application Strategy
- You may submit different personal statements and tailored experiences sections for each specialty.
- Consider editing your experiences descriptions to highlight:
- Surgical leadership, OR work, and procedural interest for neurosurgery and surgical backups
- Cognitive neurology, imaging, or critical care experiences for cognitive/diagnostic backups
Letters of Recommendation (LoRs)
- Aim for 3–4 strong neurosurgery letters (home program, away rotations, research mentors).
- For the backup specialty, obtain at least 2 specialty-specific letters (e.g., from neurologists, radiologists, anesthesiologists).
- Use ERAS to assign letters strategically:
- Neuorsurgery programs: majority neurosurgery LoRs
- Backup specialty programs: majority letters from that specialty, plus possibly one neurosurgery letter that speaks generically to your work ethic and intellect
Personal Statement Customization
- Neurosurgery PS: straightforward—your passion for neurosurgery, longitudinal commitment, research, and career goals.
- Backup specialty PS: must be authentic and specialty-specific. Avoid copy-paste from neurosurgery with superficial tweaks.
- Explain your interest in the backup field positively (not as a consolation prize), focusing on what genuinely draws you to that specialty.
Program Lists and Tiers
- For neurosurgery: apply broadly, especially to mid- and lower-tier programs if you are not a top-of-the-class applicant.
- For backup: aim for a balanced list with programs where your MD graduate profile is realistically competitive.

Step 5: Building a Strong Backup Application Without Undermining Neurosurgery
The art of backup planning lies in strengthening your plan B specialty standing while maintaining the integrity of your neurosurgery candidacy.
Integrating Backup Experiences Into Your Fourth Year
Electives/Sub-I’s
- Preserve key neurosurgery Sub-I’s if possible; these are crucial.
- Add 1–2 rotations in your backup specialty (e.g., neurology ward, neuroradiology elective) early in the year for letters and exposure.
Research Continuity
- If time allows, consider a small project in your backup specialty (e.g., stroke outcomes for neurology, imaging outcomes for radiology) that builds bridges rather than shifting focus entirely.
- Do not abandon your neurosurgery projects; instead, frame your academic interest as “neurological disease and intervention” broadly defined.
Mentorship in Both Fields
- Maintain your neurosurgery mentors—they will be crucial regardless of outcome.
- Identify at least one mentor in your backup specialty who can:
- Provide specialty-specific advising
- Write a strong letter
- Offer insight into how your neurosurgery profile will be perceived
How to Talk About Dual Interest on Rotations
On neurosurgery rotations:
- Be unequivocal about your commitment to neurosurgery—residents and attendings need to feel you are genuinely invested.
- You do not need to lead with your backup planning unless directly asked about it.
On backup specialty rotations:
- You can be transparent that you are passionate about neurological disease and are strongly considering their specialty.
- If asked directly about neurosurgery:
- Acknowledge your interest in neurosurgery historically.
- Emphasize what specifically attracts you to their specialty (e.g., the cognitive side of neurology, imaging in radiology).
- Avoid presenting them as a “second choice” in a way that might weaken your letter.
Example response:
“I’ve been very involved in neurosurgery research and clinical work, which drew me deeply into neurological disease overall. Over time, I’ve realized how much I enjoy the diagnostic side and longitudinal medical management, which is why I’m strongly considering neurology as a career path.”
Step 6: Interview Season and Ranking Strategy
Handling Interview Questions About Specialty Choice
On neurosurgery interviews:
- Focus on your commitment to neurosurgery, experiences in the field, and your understanding of its demands.
- If pressed about backup plans, you can say:
“I’ve thought carefully about the risks of this match, but my primary goal is to train as a neurosurgeon. I’ve worked hard to make myself as competitive as possible and would be honored to match at a program like yours.”
On backup specialty interviews:
- Highlight your authentic interest in that field.
- If asked directly, “Are you also applying to neurosurgery?”:
- Be honest, but concise and forward-focused:
“Earlier in my training I was strongly considering neurosurgery and remain passionate about neurologic disease. This year, I am focusing my applications on [backup specialty] because I see a strong fit with my interests in X, Y, and Z, and I’m excited about a career in this field.”
- Be honest, but concise and forward-focused:
Your goal is to reassure them that you can be fully committed and satisfied in their specialty if you match there.
Rank List Construction
A rational approach for an MD graduate with strong neurosurgery aspirations and a realistic backup specialty:
- Rank all neurosurgery programs where you would genuinely be willing to train, in order of preference.
- Then rank your backup specialty programs, again in genuine order of preference.
This structure ensures:
- If any neurosurgery program is willing to rank you high enough, you will match into neurosurgery.
- If not, you still match into a backup program you would be satisfied with rather than going unmatched.
If you find yourself ranking a backup specialty program above certain neurosurgery programs, that is a signal you may have emotionally shifted toward the backup field; discuss this with mentors before finalizing.
Step 7: If You Do Not Match into Neurosurgery
Despite careful planning, some applicants do not match into neurosurgery—even with a thoughtful brain surgery residency application. Your backup strategy determines whether this becomes:
- A pivot into a fulfilling alternative specialty, or
- A launchpad for a re-application year
If You Match into Your Backup Specialty
- Allow yourself to fully embrace your new field.
- Seek out neuro-related niches within it:
- Neurohospitalist or neurocritical care tracks in neurology
- Neuroradiology in radiology
- Neuroanesthesia in anesthesiology
- Neurorehab in PM&R
Many physicians who initially considered neurosurgery ultimately find that these plan B specialties align with their skills and values while better suiting their preferred lifestyle or practice style.
If You Go Unmatched Altogether
You will likely face choices such as:
- Neurosurgery re-application after a dedicated research year
- Pursuing a transitional year or prelim surgery spot and reassessing
- Switching to a different specialty in the following cycle with a stronger application
Your prior backup planning still helps, because:
- You have already built connections and some experience in another field.
- You can pivot more easily into a new specialty application if you decide neurosurgery is not the right long-term path.
Final Thoughts: Backup Planning as Professional Maturity
Backup specialty planning for an MD graduate in neurosurgery is not about diluting your ambition. It is about:
- Respecting the realities of allopathic medical school match statistics
- Protecting your long-term professional and financial stability
- Aligning your career with your core interests, even if the specific specialty label changes
By assessing your competitiveness honestly, clarifying what you truly value about neurosurgery, and constructing a deliberate dual applying residency strategy, you maximize your odds of ending up in a specialty where you can thrive—whether that is neurosurgery or a carefully chosen plan B specialty.
FAQ: Backup Specialty Planning for MD Graduate in Neurosurgery
1. As an MD graduate, do I really need a backup if my neurosurgery application is strong?
You may not need a backup if you are at the very top of the applicant pool: excellent Step 2 CK, strong neurosurgery research, multiple high-impact letters, outstanding Sub-I performance, and broad geographic flexibility. However, neurosurgery remains inherently high-risk due to low position numbers. Even highly competitive applicants should at least discuss backup options with trusted neurosurgery mentors and understand what plan B would look like if interviews are fewer than expected.
2. What is the most common backup specialty for neurosurgery applicants?
There is no single “standard,” but commonly chosen backups include neurology, diagnostic radiology, anesthesiology, and general surgery, sometimes PM&R with a neurorehab focus. The “best” choice depends on your interests: if you love diagnostic reasoning, neurology; if you love imaging and anatomy, radiology; if you want the OR environment, anesthesiology or general surgery. Your backup should not just be easier to match into, but also aligned with your long-term preferences.
3. Will dual applying hurt my chances in neurosurgery?
Used wisely, dual applying does not necessarily hurt your neurosurgery chances. Programs know the field is competitive and many applicants consider backups. Problems arise if your application appears inconsistent, if your neurosurgery letters or statement seem lukewarm, or if you explicitly tell neurosurgery faculty that you are “probably going to do something else.” The key is to present a cohesive, genuine neurosurgery narrative while quietly preparing a robust backup in parallel.
4. How many programs should I apply to in my backup specialty?
This depends on your risk profile, geographic constraints, and which backup you select. As a rough starting point:
- If neurosurgery is your clear priority and your risk is moderate, some applicants apply to 20–40 programs in a single backup specialty.
- If your risk is high (significant red flags, low Step 2 CK, limited neurosurgery support), you may need to apply to a broader set of backup programs (40–60+).
Final numbers should be tailored in consultation with mentors in both neurosurgery and the backup specialty, who understand the competitiveness of your specific application.
By approaching backup specialty planning strategically and early, you give yourself the best chance to transition smoothly into a fulfilling medical career—whether in neurosurgery or a carefully chosen plan B specialty.





















