Choosing a backup specialty as an MD graduate targeting urology residency can feel like planning to “fail.” In reality, thoughtful backup planning is a strategic way to protect your career, finances, and long‑term goals—without undermining your primary pursuit of a urology match.
This guide walks you step‑by‑step through how to think about backup specialties, how to decide if dual applying in residency is right for you, and how to execute a smart, realistic plan that keeps urology in play.
Understanding Your Risk in the Urology Match
Before choosing a backup specialty, you need a realistic sense of your competitiveness and risk profile for the urology match.
The Structure of the Urology Match
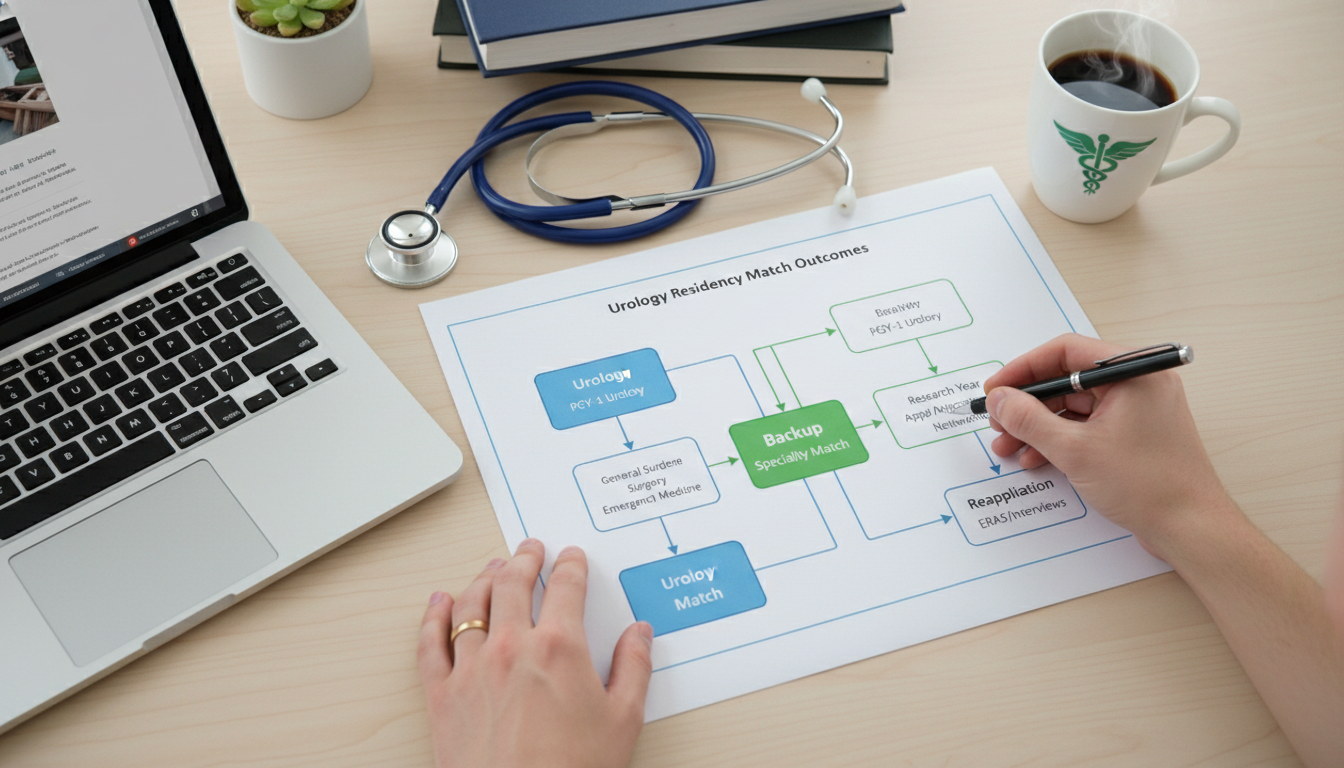
Urology uses a specialty‑specific matching process (the American Urological Association match) that runs earlier than the NRMP Main Residency Match. This timing has both advantages and implications for backup planning:
- Earlier application and interview season
- Earlier match results, leaving time to:
- Enter the NRMP for a backup specialty
- Pivot to a research year or other plan if unmatched
As an MD graduate from an allopathic medical school, you already have a relative advantage compared to some other applicant groups. However, urology is still highly competitive.
Key Competitiveness Factors
Assess your profile honestly across these domains:
- USMLE/COMLEX scores
- Step 2 CK is increasingly important, especially with Step 1 pass/fail.
- Scores below the national urology applicant mean don’t eliminate you but do increase risk.
- Clerkship performance
- Honors in surgery, urology electives, and strong narrative comments are very helpful.
- Urology‑specific experience
- Urology rotations (home and away/audition rotations)
- Strong letters from urology faculty
- Demonstrated interest over time, not just last‑minute
- Research and academic output
- Urology‑related projects, abstracts, posters, or manuscripts
- A research year can be a positive, especially if it’s clearly productive
- Personal background and story
- Career changers, non‑traditional backgrounds, or leaves of absence aren’t fatal, but should be well‑explained and framed constructively.
Who Should Strongly Consider a Backup Plan?
While everyone benefits from some level of contingency planning, a formal backup specialty or dual applying residency strategy is particularly important if you:
- Are applying without any home urology program
- Have no urology research and limited exposure to the field
- Have Step 2 CK below the typical urology applicant average
- Have failed a Step exam or repeated a year
- Have weak or generic letters from urologists
- Are applying late, with minimal time in specialty before ERAS submission
If several of these apply, you are at higher statistical risk and should take backup specialty planning seriously.
Core Principles of Backup Specialty Planning
A backup plan is not just “pick another specialty and hope.” It should be deliberate, realistic, and aligned with your long‑term goals.
Principle 1: Urology First, But Not Urology Only
If urology is your top choice, structure your efforts to maximize your chances there. That means:
- Prioritizing urology rotations during M4 (or PGY‑1 preliminary year)
- Securing high‑quality letters from urologists
- Completing urology‑specific research when feasible
- Crafting a strong urology‑focused personal statement
However, don’t let urology preparation completely crowd out your ability to create a viable plan B specialty if you know you’re in a high‑risk category.
Principle 2: Align Your Backup with Your Core Interests
Choosing a backup only because it is “easier to match” can set you up for dissatisfaction or burnout. Instead, identify what you like about urology and map those interests to a backup specialty.
Common themes that attract applicants to urology:
- Procedural/surgical work with fine motor skills
- Mixture of clinic and OR
- Longitudinal patient relationships (cancer survivorship, chronic conditions)
- Oncology and reconstructive care
- Use of technology (endoscopy, robotics, lasers)
We will later map these to logical backup and plan B specialty options.
Principle 3: Understand the Logistics of Dual Applying
Dual applying means applying to urology and a non‑urology residency in the same cycle. This increases options but has complexities:
- Different timelines: Urology (AUA) vs NRMP Main Match
- Different personal statements and letters
- Risk of appearing unfocused if your documents are not tailored
- More applications, interviews, and costs
Dual applying residency only makes sense if:
- You’re willing to rank and actually attend the backup specialty
- You have enough time to do both applications well
- Your school or mentors support the plan and help you sequence it correctly

Common Backup and Plan B Specialties for Urology Applicants
There is no single “correct” backup specialty for urology residency applicants. However, certain specialties align particularly well in terms of skill set, lifestyle, and long‑term satisfaction.
1. General Surgery (Categorical or Preliminary)
Why it fits:
- Heavy operative exposure and procedural skill development
- Similar OR environment, call structure, and acuity
- Foundation for surgical thinking and intraoperative decision‑making
- Some urology programs look favorably on applicants who did well in a surgery prelim or categorical year before re‑applying to urology
Pros:
- Strong overlap with the technical and cognitive skills used in urology
- Many patients with oncologic, acute care, or reconstructive needs
- After one year of general surgery, you can reapply to urology with:
- New letters from surgical mentors
- Additional clinical experience
- Demonstrated resilience and commitment
Cons:
- Very demanding hours and call
- If you don’t match into urology later, you must be content with a general surgery career (or its subspecialties)
- Match competitiveness is also moderate‑high
Best fit: MD graduates who genuinely like major surgery, acute care, and are open to a long‑term surgical career independent of urology.
2. Internal Medicine (Categorical)
Why it fits:
- Overlaps with urologic oncology, chronic disease management, nephrology, and complex medical decision‑making
- Good option for those drawn to thoughtful diagnostic work and long‑term patient relationships
- Internal medicine opens doors to many fellowships (oncology, nephrology, palliative care, etc.) where you might still work extensively with urologic patients.
Pros:
- Broad medical base and excellent career flexibility
- Widely available positions, often with more predictable matching than some surgical fields
- Lifestyle is variable and can be optimized with practice choice
Cons:
- Less hands‑on procedural work compared to urology
- For highly procedure‑oriented personalities, may feel too cognitive
- You must be willing to truly embrace IM as a career if urology does not work out
Best fit: Applicants who enjoy oncology, complex medical management, and longitudinal care, and who are open to subspecialty paths.
3. Radiation Oncology (Context‑Dependent)
Why it fits:
- Strong connection with urologic malignancies (especially prostate, bladder, and testicular cancers)
- Heavy use of technology, imaging, and long‑term cancer care
Caveats:
- Radiation oncology has faced volatile job market concerns and shifting applicant numbers.
- It is not always a straightforward “backup,” and in some years it is very competitive.
This route is reasonable only if:
- You are authentically interested in cancer care and radiotherapy
- You’ve discussed the current job market and landscape with radiation oncologists
- You understand it is its own distinct long‑term career, not merely a temporary compromise
4. Transitional Year + Re‑Apply Strategy
This is not a separate specialty, but a structural plan:
- Match into a transitional year (TY) or a preliminary internship (often medicine or surgery)
- Spend that year doing:
- Strong clinical work
- Additional urology research
- Networking with urology faculty
- Re‑apply to urology with a stronger application
This pathway can be a good “bridge” if:
- You’re committed to re‑applying to urology
- You can secure a supportive internship where program leadership encourages your re‑application
- You’re aware there is still no guarantee of matching into urology on re‑application
However, for TY or prelim paths, it’s still wise to have a contingency within that field (e.g., being open to continuing in categorical internal medicine or surgery if further urology attempts are unsuccessful).
5. Emergency Medicine (Selective Fit)
Some urology‑interested students also consider emergency medicine as a backup:
Why it might fit:
- Fast‑paced environment with procedures and acute care
- Frequent exposure to urologic emergencies (stones, retention, trauma)
Concerns:
- Very different long‑term practice pattern from urology
- Recent job market and workforce concerns in emergency medicine in some regions
- Limited continuity and longitudinal care
EM is best considered only if you’ve had strong clinical rotations in EM, genuinely enjoy the environment, and have realistic expectations about its evolving landscape.
How to Decide: A Structured Process for MD Graduates
Instead of picking a backup specialty based on hearsay, walk through a systematic decision‑making process.
Step 1: Clarify What You Want in Your Career
List your top 5–7 priorities. For example:
- High volume of hands‑on procedures
- Long‑term patient relationships
- Primary interest in oncology, reconstructive care, or men’s health
- Predictable schedule vs. comfort with nights/weekends/trauma
- Academic vs community practice goals
- Geographic flexibility
Rank these priorities. This ranking should guide which backup specialties make sense.
Step 2: Map Your Interests to Specialties
Create a simple table (on paper or your computer):
| Core Interest | Urology | Gen Surg | IM | Rad Onc | EM |
|---|---|---|---|---|---|
| High procedural content | High | High | Low | Medium | High |
| Longitudinal relationships | Medium | Medium | High | High | Low |
| Oncologic focus | High | High | High | High | Low |
| Lifestyle control potential | Medium | Low | High | Medium | Medium |
| Use of technology | High | Medium | Low | High | Medium |
Then reflect: if urology disappeared tomorrow, which column would you pick?
Step 3: Consult Mentors—Both Urology and Non‑Urology
You should have at least two layers of mentorship:
- Urology faculty or residents
- Honest assessment of your chances in the urology match
- Suggestions about whether a research year, TY, or prelim year makes sense
- Non‑urology mentors (e.g., internal medicine, general surgery, student affairs dean)
- Perspective on your fit for other fields
- Guidance on how the allopathic medical school match works in those specialties
- Help with dual applying residency strategy and ERAS planning
Bring specific questions, such as:
- “If I submit this application as‑is, what is my realistic match probability in urology?”
- “If I do a research or prelim year, how much would that change my prospects?”
- “Based on working with me, do you see me as a better fit for surgery, IM, or another specialty?”
Step 4: Run Scenario Planning
Sketch 3–4 concrete scenarios for the coming 2–3 years:
- Scenario A: Match in urology this cycle.
- Scenario B: Don’t match in urology → match in backup specialty (e.g., IM).
- Scenario C: Don’t match in urology or backup → take research year or TY/prelim and re‑apply.
- Scenario D: Re‑apply again and still don’t match urology.
Ask yourself:
- In which scenarios would I still feel content and professionally fulfilled?
- Are there any scenarios I would absolutely not accept? If so, adjust your backup plan now.
Practical Execution: How to Implement a Backup or Dual Applying Plan
Once you’ve chosen a backup strategy, you’ll need to align your application documents, interview approach, and rank lists.
Application Materials: Keeping Stories Straight
If you’re dual applying, you’ll typically prepare:
- One personal statement for urology
- One personal statement for your backup specialty
- Sometimes a generic version (e.g., for preliminary or transitional spots)
Key tips:
- Do not reuse your urology statement for internal medicine (or vice versa).
- Each statement should clearly articulate why that field is your true interest, not why it is a consolation prize.
- It’s acceptable for there to be overlapping themes (e.g., love of oncology, continuity of care, team‑based practice), but:
- Avoid language that clearly references urologic procedures or the urology match in your other specialty statement.
- Be honest but not self‑sabotaging: you don’t need to state “my first choice was actually urology” in your backup specialty materials.
Letters of Recommendation
For urology:
- Prioritize 3–4 strong letters from urologists who know you well.
- Include at least one from your home institution (if possible).
For backup specialties:
- Secure 2–3 letters from faculty in that specialty (e.g., internal medicine attendings for IM applications).
- A generic “surgery” letter might be acceptable for prelim positions but is weaker for categorical spots if it is not specialty‑specific.
Coordinate with letter writers:
- Let them know you are dual applying if appropriate and if you trust them. Many faculty appreciate the transparency and will help you tailor letters.
- Ensure your ERAS assignments are correct for each program so they receive the right set of letters.
Interview Strategy
During interviews:
For urology interviews, present yourself as fully committed to a urology career. Programs expect genuine interest and clear reasons for choosing the field.
For backup specialty interviews, also present authentic enthusiasm for that specialty. If asked directly:
- You can acknowledge an interest in multiple fields early in training.
- Emphasize what you find compelling about their specialty.
- Avoid framing them as your “backup.” Instead, say something like:
“I explored both urology and internal medicine during medical school. Over time, I realized how much I value longitudinal relationships and complex diagnostic work, which is why I’m excited about training in internal medicine.”
Do not lie, but you also don’t need to share your entire application history if not asked.
Ranking and Timeline
Because urology uses the AUA match:
- Submit urology applications first, interview, and rank.
- When the urology match results are released:
- If you match into urology:
- You can withdraw from backup applications or update programs politely.
- If you do not match:
- Decide immediately whether you’re still aiming for a urology career (via research year or prelim) or if you’re ready to commit to your backup specialty.
- Use the remaining time before the NRMP rank list deadline to refine your backup rank list and potentially add programs if feasible.
- If you match into urology:
Carefully discuss this timing with your school’s dean’s office or career advisor, as institutional policies and support processes can vary.
Long‑Term Career Considerations: If Urology Doesn’t Work Out
It is emotionally difficult to consider the possibility that you might never match urology, especially after preparing for years. However, planning for that possibility can reduce anxiety and improve decision‑making.
Re‑application vs. Committing to Backup Specialty
Factors supporting a re‑application to urology:
- You came close to matching (good number of interviews, strong feedback).
- You identified fixable weaknesses (late letters, no research, fewer audition rotations).
- You have access to an excellent research year or a supportive prelim/TY that specifically bolsters your urology candidacy.
- You have strong emotional resilience and financial capacity to manage another application cycle.
Factors suggesting you should commit fully to the backup specialty:
- You received very few urology interview invitations, despite a broad application strategy.
- Multiple urology mentors advised that your profile is unlikely to change enough with another year.
- You discover that you genuinely enjoy your backup specialty, with good performance and mentor support.
- You feel burned out by the uncertainty and want a stable, forward‑moving path.
Neither path is “failure.” Many outstanding physicians found their true fit after an initial pivot.
Identity and Professional Fulfillment
If urology has been central to your identity, not matching can be painful. But remember:
- Your motivations—helping patients, working on complex problems, engaging in procedural or cognitive work—are not unique to urology.
- You can still work closely with urologic patients in oncology, nephrology, internal medicine, or palliative care.
- Leadership, research, teaching, advocacy, and innovation exist in every specialty.
Give yourself time and, if needed, seek support (peers, mentors, counseling services) to process any disappointment and to rebuild a positive narrative around your chosen field.
FAQs: Backup Specialty Planning for Urology‑Bound MD Graduates
1. As an MD graduate from an allopathic medical school, do I really need a backup if I’m applying to urology?
It depends on your individual competitiveness. Some allopathic MD graduates with strong metrics, robust urology research, and home‑program support can apply to urology without a formal backup and still have high probability of success.
However, if you have score concerns, limited urology exposure, or no home program, a backup or at least a structured plan B (e.g., research year, TY/prelim) is very wise. Even for strong candidates, having a contingency reduces stress and provides options if circumstances change (illness, family needs, or personal reassessment).
2. Will dual applying hurt my chances in the urology match?
Not automatically. Many applicants quietly pursue dual applying residency strategies. The risk comes when:
- Your urology application appears diluted (generic statement, few urology‑specific letters).
- You spend so much time on backup applications that your urology preparation suffers (fewer auditions, incomplete research projects).
- A program explicitly discovers you are uninterested or only lukewarm about urology.
If you keep your urology application focused and strong and manage your time well, dual applying does not inherently damage your chances.
3. What is the most common backup specialty for urology applicants?
There is no single universal answer, but many urology‑interested MD graduates lean toward:
- General surgery (especially if highly procedure‑oriented)
- Internal medicine (if drawn to complex medical and oncologic care)
- Occasionally radiation oncology, emergency medicine, or a TY/prelim year
The “best” backup is not what’s popular—it’s the plan B specialty you could realistically see yourself practicing long‑term if urology doesn’t work out.
4. Should I take a dedicated research year instead of applying with a backup specialty?
A research year can be a powerful way to strengthen a future urology application, especially if you:
- Have weak or no urology research
- Need more time to secure strong letters and audition rotations
- Can join a productive, supportive urology research team
However, a research year does not guarantee a future urology match, and it delays your income and training. For some, a direct dual application with a backup specialty makes more sense; for others, a research year followed by urology re‑application is better. Discuss this decision with your mentors, taking into account your financial situation, goals, and current application strength.
Thoughtful backup specialty planning does not mean you are giving up on urology; it means you are treating your career with the seriousness and foresight it deserves. As an MD graduate, you have multiple viable paths to a rewarding life in medicine—urology is one of them, but not the only one. By approaching the urology match and your plan B specialty strategically, you protect both your aspirations and your future.





















