
Why Backup Specialty Planning Matters for IMGs Targeting Urology
For an international medical graduate, urology residency in the United States is both exciting and high‑risk. Urology is a small, competitive field with limited positions, early match timelines, and strong preference for home‑program or U.S. graduates. Even highly qualified IMGs can struggle to secure a spot on their first attempt.
That’s why a carefully designed backup specialty strategy is essential. It is not a sign of weakness or lack of confidence—it is risk management. A solid IMG residency guide always emphasizes two truths:
- You should give your primary dream (urology) a full, honest attempt.
- You should protect your long‑term career with a realistic, well‑planned Plan B specialty if urology does not work out.
This article will walk you through:
- Understanding your specific risk profile as an IMG urology applicant
- Choosing appropriate backup fields and whether to dual apply
- Coordinating timelines between the urology match and the NRMP Main Match
- Structuring away rotations, exams, and letters to serve both plans
- Creating a year‑by‑year roadmap and avoiding common pitfalls
The goal is not to talk you out of urology. The goal is to help you pursue urology intelligently—without leaving yourself unprotected if the match outcome is unfavorable.
Understanding Your Risk Profile as an IMG Urology Applicant
Before choosing a backup specialty, you must understand how competitive you are for urology specifically as an international medical graduate.
Key Factors That Determine Risk
Consider the following dimensions honestly:
Medical school background
- U.S.-IMG (Caribbean or U.S.-affiliated school) vs non‑U.S. IMG
- School reputation and clinical exposure in the U.S.
- Percentage of alumni who successfully match into competitive specialties
Standardized test performance
- USMLE Step 1 (even though pass/fail, performance signal still matters)
- USMLE Step 2 CK score: For urology, a strong score (often ≥ 240–245) is very helpful. Lower scores raise risk significantly, especially for IMGs.
Clinical experience and mentorship in urology
- U.S. urology rotations or observerships
- Hands‑on surgical experience (if permissible)
- Strong letters from urologists at known U.S. institutions
Research productivity in urology
- Urology‑specific publications, abstracts, conference presentations
- Involvement with a known academic urologist or department
- Evidence of academic commitment to the field
Visa status
- U.S. citizen, permanent resident, or requiring visa (J‑1/H‑1B)
- Visa need significantly reduces program list for IMGs in most specialties, including urology.
Timing and attempts
- First‑time applicant vs repeat urology applicant
- Years since graduation (YOG): many programs prefer ≤ 5 years since graduation.
Rough Self‑Assessment Categories
These categories are not official, but they can help guide your backup planning.
Relatively strong IMG urology candidate
- Step 2 CK ≥ 245
- Recent graduate (≤ 3–4 years)
- 1–3 U.S. urology rotations with strong letters
- At least a few urology research projects or case reports
- No major red flags, visa feasible
→ Reasonable to pursue urology aggressively, but still wise to plan backup.
Moderate‑risk IMG urology candidate
- Step 2 CK ~ 230–244
- Some U.S. clinical exposure, but limited urology‑specific experience
- Minimal urology research, or older YOG
- Needs visa or has minor red flags
→ Strongly consider a structured dual applying residency strategy with a realistic Plan B specialty.
High‑risk IMG urology candidate
- Step 2 CK < 230, or significant exam failures
- Older YOG (> 5–7 years)
- Little or no U.S. experience
- Weak or no urology research; needs visa
→ Urology can still be a long‑term goal, but primary focus may need to shift to a more attainable specialty first (e.g., internal medicine) plus strategy to re‑enter urology later via research or fellowship.
Being honest with yourself at this stage will help shape your backup plan wisely, rather than emotionally.
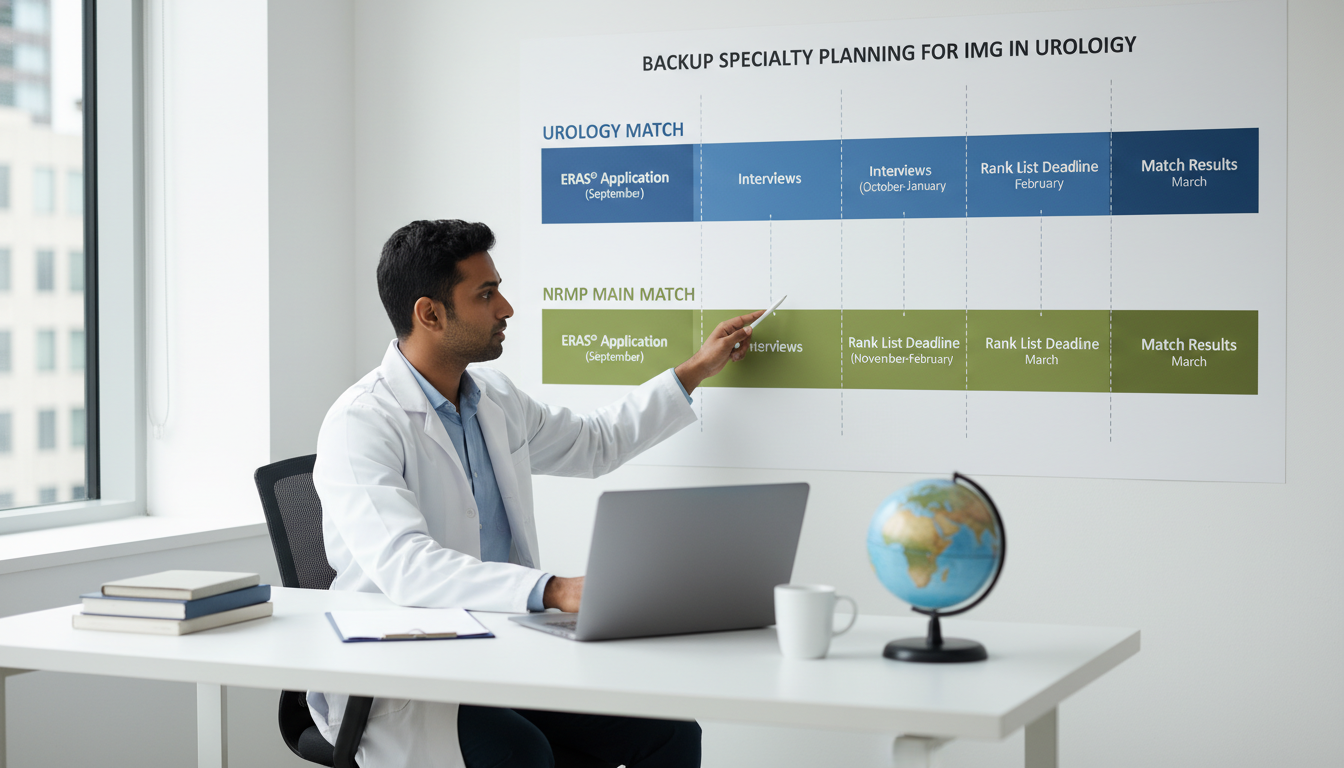
How the Urology Match Interacts with Backup Specialty Planning
To design your backup plan, you must understand the structure and timeline of the urology match relative to the NRMP Main Match.
Urology’s Early Match: Key Features
- Urology participates in a separate match administered by the American Urological Association (AUA), but it is now synchronized with ERAS for application submission.
- Interviews typically occur earlier than many other specialties (often late fall).
- Rank list certification and the urology match results are usually released before the NRMP rank list deadline.
Practical impact for IMGs:
You can apply to urology and a NRMP specialty (e.g., general surgery, internal medicine) in the same season. You will know your urology match result before having to finalize your NRMP rank list.
This structure makes dual applying much more feasible: you can commit fully to urology while applying simultaneously to a backup specialty that participates in the NRMP Main Match.
Common Dual‑Application Pathways with Urology
Here are some typical combinations IMGs consider:
Urology + General Surgery
Logical overlap in surgical interest; both competitive and require strong scores and letters.Urology + Internal Medicine
Very different day‑to‑day work, but IM is more accessible for IMGs and offers nephrology or oncology pathways related to GU disease.Urology + Transitional Year (TY) / Preliminary Surgery
Can be used to stay in the system, improve your profile, and reapply to urology later.Urology + Family Medicine (FM)
For high‑risk or late‑career IMGs who still want a U.S. clinical role but recognize lower odds in urology.
The best backup specialty for you depends on your risk profile and your genuine tolerance for an alternate career path.
Choosing a Backup Specialty: Strategy for IMG Urology Applicants
The central question: If I do not match urology this year, what path will still give me a meaningful, sustainable career—and possibly a second chance at urology if I want it?
Core Principles for Choosing a Plan B Specialty
It must be a specialty you can tolerate—or ideally, enjoy.
You may spend your entire career in this field if you never transition to urology.It should be realistic given your profile as an IMG.
There is no point backing up urology with another equally or more competitive field (e.g., dermatology, plastic surgery) if your metrics are average.It should share some overlap with your interests or skills.
Overlap can be clinical (e.g., surgery, nephrology), procedural (e.g., IR), or patient population.It should provide leverage if you re‑target urology or related areas later.
Look for fields that allow you to work with urologic patients, manage related conditions, or collaborate with urologists.
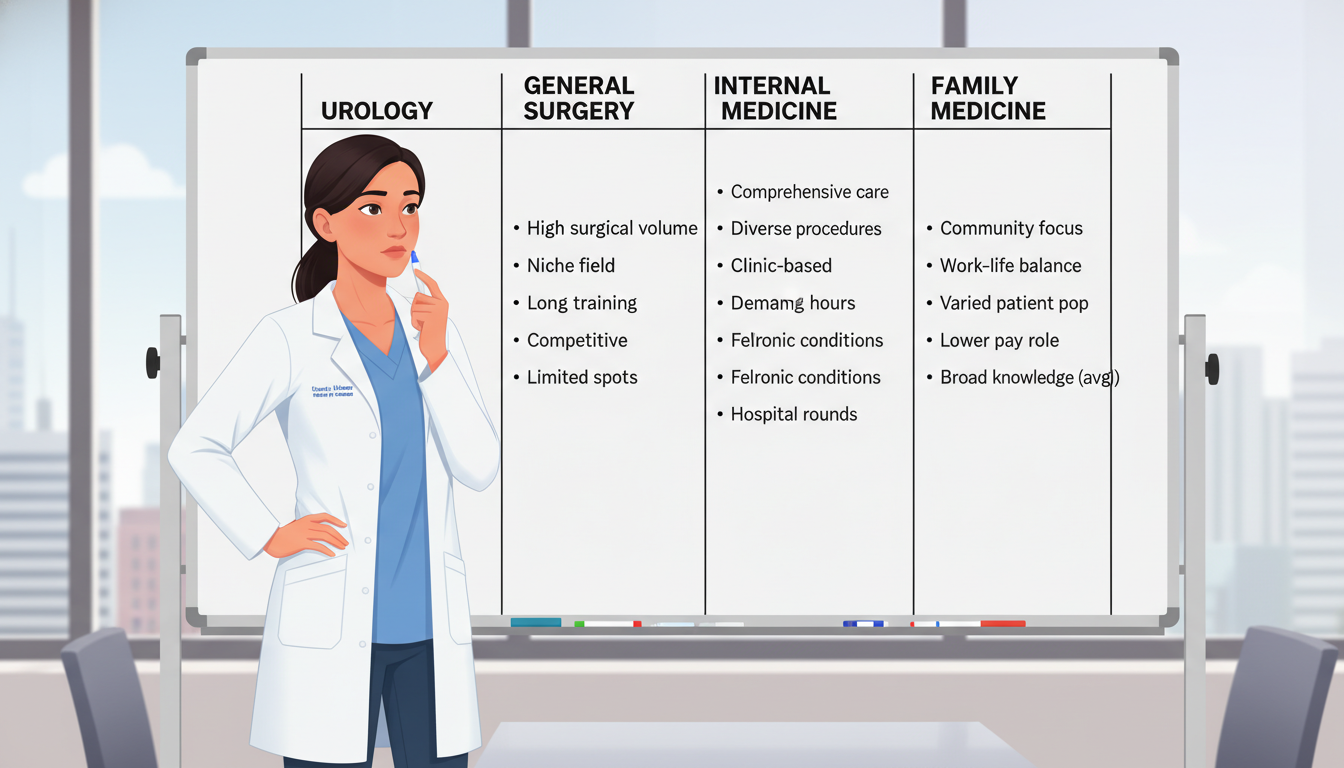
Common Plan B Specialty Options for IMG Urology Applicants
Below are some frequently considered Plan B specialties, with pros, cons, and fit for IMGs.
1. General Surgery
Why it’s attractive:
- Similar operative environment and surgical mindset
- You can subspecialize later in fields with GU overlap (e.g., surgical oncology involving GU tumors at some centers).
- Many skills (OR management, peri‑operative care, endoscopy) transfer directly.
Concerns:
- Also competitive for IMGs, especially at university programs.
- Long training (5+ years) and physically demanding.
- Letters and research often need to be surgery‑specific, not just urology‑specific.
Best for:
IMGs with strong Step scores, good surgical rotations, and genuine interest in surgery even beyond urology.
2. Internal Medicine
Why it’s attractive:
- One of the more attainable specialties for IMGs overall.
- Broad clinical exposure, stable career paths.
- You can gear your career toward GU‑related fields (e.g., nephrology, oncology, palliative care for GU cancers).
Concerns:
- Very different from operative urology; fewer procedures (although specialties like cardiology, GI, and pulmonary are more procedural).
- If surgery is your true passion, you must seriously consider whether you’ll be satisfied in IM.
Best for:
Candidates who like complex medical reasoning, chronic disease management, and want a stable and versatile career backup.
3. Transitional Year (TY) / Preliminary Surgery
Why it’s attractive:
- Offers a one‑year foothold in the U.S. system.
- You can build U.S. experience, strengthen letters, improve research output, and reapply to urology or another field.
- Useful for those determined to reattempt competitive specialties.
Concerns:
- Not a long‑term specialty by itself; you must have a clear plan for the next step.
- Prelim positions can be intense with limited support.
- No guarantee of transitioning to a categorical urology or surgery position later.
Best for:
Relatively strong IMGs who narrowly miss urology, and for whom a second attempt is realistic and supported by mentors.
4. Family Medicine
Why it’s attractive:
- Often more receptive to IMGs and visa‑requiring applicants.
- Shorter training (3 years) and broad scope of practice.
- You can develop a niche in men’s health, sexual dysfunction, LUTS, prostate cancer survivorship, or primary care urology.
Concerns:
- Far removed from the OR and major surgeries.
- Financial and lifestyle differences compared with procedural/surgical fields.
Best for:
High‑risk or later‑career IMGs who primarily want a guaranteed clinical career in the U.S. and are flexible with specialty choice.
5. Other Less Common Backups
- Pathology: Can work closely with urologists on GU specimens, but limited patient contact.
- Radiation Oncology: Strong GU overlap but quite competitive and shrinking job market in some regions.
- Interventional Radiology (IR): GU interventions, but extremely competitive, often harder for IMGs than urology.
For most IMG urology hopefuls, the practical backup specialty shortlist is:
General Surgery, Internal Medicine, TY/Prelim Surgery, or Family Medicine.
How to Execute a Dual‑Application Strategy Without Diluting Your Urology Application
The central challenge of dual applying residency is balance. You must present a strong narrative and portfolio for urology, while also being competitive in your Plan B specialty—without sending mixed signals to programs.
1. Personal Statements: Separate and Focused
- Write two distinct personal statements:
- One fully dedicated to urology: your exposure, reasons for choosing it, research, and long‑term goals.
- One tailored to your backup field (e.g., internal medicine) that feels authentic and not obviously “second choice.”
Tip:
Do not mention your plan to apply to urology in the internal medicine personal statement. Programs want to see commitment to their specialty.
2. Letters of Recommendation: Mix Strategically
For urology applications:
- Aim for 3–4 letters, with at least 2 from urologists who know you well.
- A strong letter from a general surgeon can also help; it shows operative performance and work ethic.
For your backup specialty:
- Try to secure 1–2 letters from faculty in that field (e.g., IM attendings) if possible.
- If that’s impossible, a letter from a urologist emphasizing your clinical reasoning, professionalism, and team skills is still better than nothing.
ERAS Tip:
You can assign letters selectively to each program; design your letter sets so urology programs mostly see urology letters, while IM/surgery programs see at least one letter from their own specialty.
3. Research and CV Positioning
- It’s acceptable (and normal) that your research is heavily urology‑focused if that’s your dream.
- When interviewing in the backup field, frame your research as evidence of:
- Academic curiosity
- Experience in clinical trials, data analysis, or quality improvement
- Commitment to learning complex disease processes
Programs care more about how you did the research and what it shows about your work ethic than about the topic itself.
4. Rotations and Electives
If you have limited U.S. clinical time, you need to be deliberate:
Minimum for urology:
- At least 1–2 dedicated urology rotations or observerships in the U.S., ideally at institutions that accept or have matched IMGs.
For the backup specialty:
- Try to obtain at least one rotation in that field. For example:
- An inpatient internal medicine month
- A general surgery or trauma surgery rotation
- This gives you a legitimate basis to speak about your interest and secure letters.
- Try to obtain at least one rotation in that field. For example:
Avoid spreading yourself so thin that you don’t impress anyone deeply. Depth in a few well‑chosen experiences beats superficial exposure everywhere.
5. Program List Strategy
For urology, apply broadly, focusing especially on:
- Programs known to have matched IMGs in recent years
- Community or hybrid academic‑community programs
- Institutions or states more open to visa sponsorship
For your backup specialty, apply very broadly:
- Many IMGs underestimate how many applications they need: 80–120+ is common for IM or FM; even more for general surgery if your profile is marginal.
- Prioritize programs with a history of IMG matching and, if necessary, visa support.
6. Interview Season Management
- Urology interviews often come early and can cluster.
- Accept as many urology interviews as you reasonably can—each one is valuable given the small number of programs.
For the backup specialty:
- Don’t cancel all non‑urology interviews while you’re still uncertain about your urology chances.
- Prioritize interviews at programs most realistic for you (IMG‑friendly, visa‑friendly).
After the urology match results come out:
If you match urology:
- Withdraw from NRMP and inform any NRMP programs where you interviewed, professionally and promptly.
If you do not match urology:
- Pivot fully to your backup specialty.
- Use your remaining time before NRMP rank deadline to:
- Attend all backup interviews you can.
- Update programs (when appropriate) to reinforce your commitment to their specialty.
Long‑Term Strategy: If You Don’t Match Urology
Even with excellent planning, some IMGs will not match into urology—either on the first attempt or at all. How you respond is crucial.
Option 1: Reapply to Urology After Strengthening Your Profile
This path makes sense if:
- You came close (e.g., some interviews, strong feedback, but no match).
- Mentors in urology honestly encourage another attempt.
- You are prepared to significantly strengthen your application.
Common ways to improve:
Research Year in Urology
- Join a research group at a U.S. urology department.
- Aim for publications, conference presentations, and strong mentorship.
- Demonstrate serious academic commitment.
Preliminary Year or TY with Strong Surgical Exposure
- Excel clinically, especially in surgical or urologic rotations.
- Build relationships with urology departments for letters and potential openings.
Improve Testing/Certifications
- Higher Step 2 CK (if retake allowed in rare situations or if Step 3 is pending).
- Complete Step 3 early, which can be attractive for visa‑requiring candidates.
Reapplication should be deliberate, not automatic. If your profile is very weak, repeated unsuccessful attempts can harm you.
Option 2: Commit to Your Backup Specialty and Build a Satisfying Career
If mentors and your own reflection suggest that urology is not realistic, you can channel your urology passion into niches within your Plan B field:
In Internal Medicine:
- Specialize in nephrology or oncology with a focus on GU diseases.
- Work closely with urologists managing stone disease, BPH, or GU cancers.
- Run multidisciplinary clinics with urology partners.
In Family Medicine:
- Develop a men’s health clinic focusing on erectile dysfunction, BPH screening, and post‑prostatectomy primary care.
- Become the go‑to physician in your community for GU primary care issues.
In General Surgery:
- Take on cases with overlapping domains, collaborate on complex pelvic surgeries, and engage in multidisciplinary tumor boards with urology.
Your training and passion for urology do not disappear; they simply shape your practice in a different specialty.
Frequently Asked Questions (FAQ)
1. Is it “bad” to dual apply to urology and another specialty as an IMG? Will programs see me as less committed?
Dual applying is common, especially in competitive fields like urology. Programs understand that applicants must protect their careers. The key is how you present yourself: each program should feel that you are genuinely interested in their specialty and program. Using specialty‑specific personal statements and letters, and being honest (but not oversharing) in interviews, will prevent you from looking unfocused.
2. Which is the best backup specialty for an IMG targeting urology?
There is no single best option. It depends on your risk profile and personal preferences:
- If you love surgery and are relatively strong: General Surgery or Prelim/TY.
- If your metrics are average and you want stability: Internal Medicine.
- If you are high‑risk or need a more IMG‑friendly route: Family Medicine.
Choose a Plan B specialty in which you could realistically see yourself practicing long term.
3. How many programs should I apply to in my backup specialty?
As an IMG, think in terms of broad application numbers:
- Internal Medicine: often 80–120+ programs
- Family Medicine: 60–100+ programs, depending on your profile
- General Surgery: 80–150+ for many IMGs, particularly if scores are not exceptional
These are approximate ranges, not strict rules. Your advisor or mentor can refine this based on your specific metrics and visa needs.
4. I matched into my backup specialty, but I still dream of urology. Can I switch later?
Switching from one residency to another (e.g., IM to urology) is possible but uncommon and complex. Realistically:
- Most residents who remain in their matched specialty complete that training and build a career there.
- If you are serious about switching, you’ll need:
- Strong urology mentors and advocates
- Evidence of exceptional performance in your current program
- An available slot (often due to attrition) in a urology residency
Consider the cost—emotional, financial, and logistical—before betting on this path. For many, it is healthier to fully commit to excelling in the specialty where they matched.
By planning your backup specialty thoughtfully, aligning it with your risk profile, and executing a strategic dual applying residency approach, you can pursue urology ambitiously while still protecting your long‑term future as an international medical graduate.





















