
Why Every IMG Interested in Vascular Surgery Needs a Backup Plan
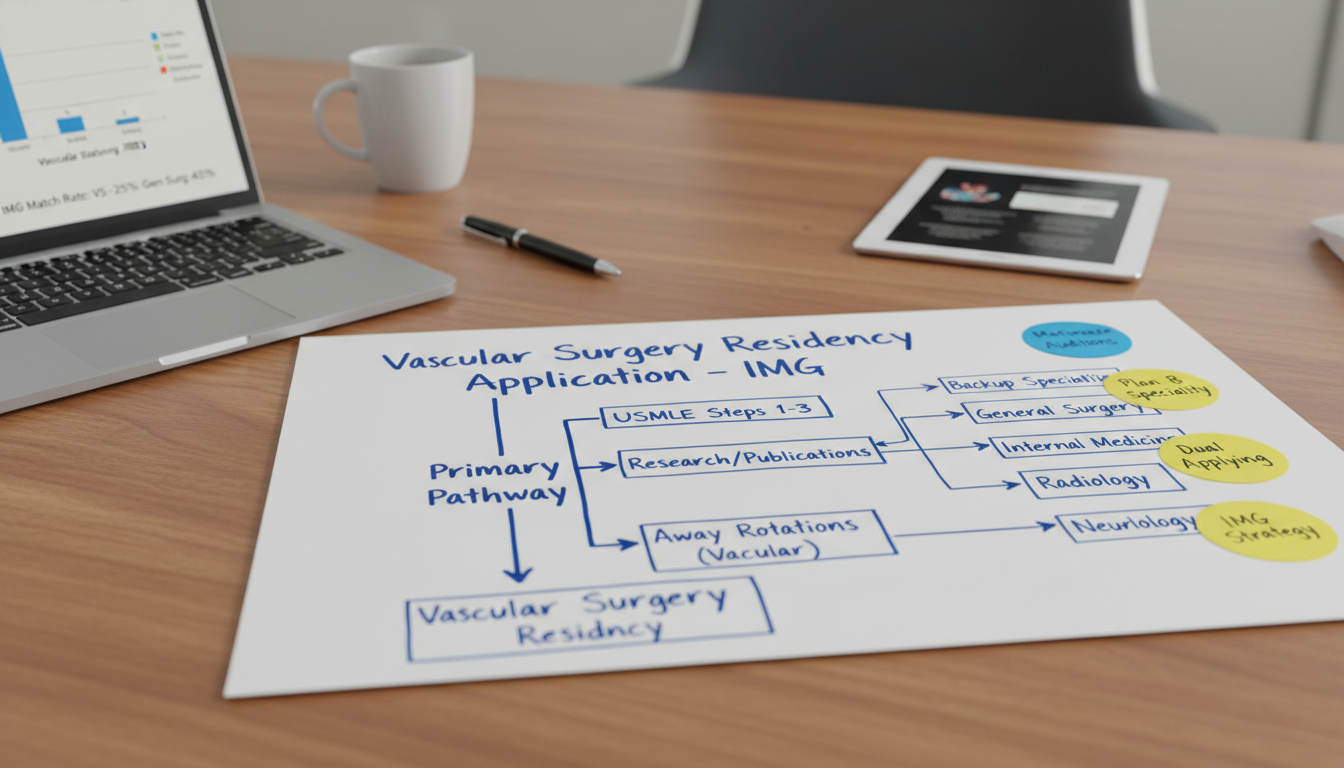
Vascular surgery is one of the most competitive surgical fields in the United States, and that competitiveness is amplified for an international medical graduate (IMG). Even well-qualified candidates sometimes go unmatched in vascular surgery residency or an integrated vascular program. That reality makes structured backup specialty planning not just “nice to have” but essential risk management.
As an IMG residency applicant, you are investing a huge amount of time, money, and emotional energy into this process. A carefully designed backup specialty or dual applying residency strategy protects that investment and maximizes your chances of:
- Matching into some ACGME-accredited residency in the US
- Staying aligned with your long‑term goal of caring for patients with vascular disease
- Avoiding costly, demoralizing gaps or repeated failures to match
This IMG residency guide will walk you through how to select and structure your plan B specialty choices, how to dual apply wisely, and how to communicate your strategy without undermining your primary interest in vascular surgery.
Understanding the Competitiveness of Vascular Surgery for IMGs
Before building a backup plan, you need a realistic understanding of where vascular surgery stands in the residency landscape—especially for IMGs.
Key structural features of vascular surgery training
There are two main pathways:
Integrated Vascular Surgery Residency (0+5)
- Enter straight from medical school
- 5 years total
- Highly competitive and relatively few positions
- Most programs heavily favor US MD graduates with strong academic metrics
Traditional Pathway (5+2)
- 5-year General Surgery residency + 2-year Vascular Surgery fellowship
- More total training positions overall (because of general surgery)
- Opens additional entry points for IMGs (e.g., prelim or categorical general surgery)
For an IMG, direct entry into an integrated vascular program is particularly challenging due to:
- Limited number of spots
- Preference for US-based clinical experience and letters
- Heavy emphasis on research, especially vascular‑specific
This doesn’t mean it’s impossible—but it does mean that most IMGs who ultimately become vascular surgeons do so through the 5+2 route, often after first matching into general surgery or another surgical specialty that keeps vascular doors open.
What this means for your backup strategy
Because of the structure and competitiveness of vascular surgery:
Your plan B specialty should ideally:
- Keep you close to vascular patients, procedures, or surgical care
- Offer realistic match chances for an IMG
- Still allow pathways to fellowship training if you remain interested in vascular disease
A dual applying residency strategy (vascular surgery + a related specialty) is often the safest approach, especially if:
- Your USMLE scores are not in the top percentile ranges
- You have limited US research or clinical experience
- You are not strongly geographically flexible
Principles of Smart Backup Specialty Planning for IMGs
Before naming specific specialties, understand the guiding principles that make a backup plan effective.
1. Realistic self-assessment
Be brutally honest about your application:
Scores and exams
- USMLE Step 2 CK: Below-average? Average? Strong?
- Any failures or attempts on Step or OET?
Clinical experience
- US clinical experience (USCE): observerships vs hands‑on electives
- Any vascular or surgical rotations in the US?
Research
- Publications, especially related to vascular surgery, general surgery, cardiology, radiology, or critical care?
- Quality (peer-reviewed vs. posters only)?
Visa status
- Needing J‑1 vs open to H‑1B?
- Countries of citizenship that may be viewed differently by some programs?
The more “red flags” or gaps you have (low scores, attempts, limited USCE, visa needs), the more conservative your backup specialty plan must be.
2. Alignment with long-term vascular interests
A backup specialty is not just “anything I can match into.” For both career satisfaction and strategy, you want specialties that:
- Still interact with vascular disease (e.g., peripheral arterial disease, aneurysms, venous thromboembolism)
- Offer procedural opportunities if you like interventions (e.g., IR, cardiology, neurology with stroke, critical care)
- Allow involvement in multidisciplinary vascular teams
This alignment makes your story coherent and your future options broader.
3. IMG friendliness and program volume
You should preferentially consider:
- Specialties with a higher proportion of IMG residents
- Specialties with many programs and larger class sizes, creating more total positions
- Programs with documented history of sponsoring visas
This doesn’t mean you abandon ambition—it means you calibrate ambition to opportunity.
4. Geographic and program flexibility
The narrower your geography (e.g., “only Northeast” or “only California”), the more you must compensate with:
- Stronger scores and stronger CV, or
- A more conservative backup strategy with more applications and broader specialty list
If you’re highly flexible about location, your chances improve considerably in most fields.

Best Backup and Plan B Specialties for Vascular‑Interested IMGs
Below are the major categories of backup options and how they relate to vascular surgery. Your optimal plan B specialty will depend on your profile, risk tolerance, and primary interests.
1. General Surgery – The Classic and Most Direct Backup
Why it’s a strong choice:
- Most direct route to 5+2 vascular fellowship
- High overlap with vascular surgery cases, especially in large academic centers
- Allows you to maintain your “surgical identity”
- Many programs with prelim and categorical positions
Pros for IMGs:
- Many general surgery programs are open to IMGs, especially community-based and university-affiliated community programs
- Prelim years can sometimes be a foothold into categorical positions or later vascular opportunities
Cons:
- Still competitive for categorical spots, especially at academic programs
- Training is long and demanding; lifestyle can be challenging
- Matching into a weaker general surgery program doesn’t guarantee you’ll later match into a vascular fellowship
Who should strongly consider this plan B specialty:
- IMG applicants with:
- Solid Step 2 CK score (ideally >235–240 for competitive settings; lower may still work in community programs)
- Surgical research or vascular research
- Strong letters from surgeons or vascular surgeons
- Demonstrated hands-on surgical interest and experience
Practical strategy:
Dual apply to:
- Integrated vascular programs where competitive
- A broad range of general surgery programs (especially those known to accept IMGs)
In your personal statement and interviews for general surgery:
- Emphasize your interest in a broad surgical foundation
- Mention vascular as an interest, but avoid implying you see general surgery as merely a “stepping stone”
2. Interventional Radiology or Diagnostic Radiology
Why IR/Dx Radiology can be relevant:
- Vascular and interventional radiology (VIR) is heavily involved in endovascular procedures—angioplasty, stenting, embolization, thrombolysis
- Diagnostic radiologists interpret vascular imaging (CTA, MRA, Doppler US) daily
- Maintains a strong connection with vascular disease management
Pros for IMGs:
- High degree of procedural work in IR for students who love interventions
- Radiology can be more IMG-friendly than some surgical subspecialties, depending on the region
Cons:
- Interventional Radiology itself is highly competitive—often not a “low-risk” backup
- Requires comfort with physics, imaging, and often more solitary reading work in diagnostic roles
- Some radiology programs are not IMG-friendly; you must research carefully
Who this fits best:
- IMGs with:
- Interest in imaging and minimally invasive procedures
- Strong test scores and possibly research in imaging, IR, or vascular topics
- Flexibility in location and type of program
Practical strategy:
Consider dual applying to:
- Vascular surgery (integrated)
- Diagnostic radiology (and possibly IR tracks if your profile is strong enough)
Emphasize in radiology applications your interest in vascular imaging, multidisciplinary collaboration, and longitudinal patient care.
3. Internal Medicine with Cardiology or Vascular Medicine Focus
Why this is a powerful yet flexible plan B specialty:
- Internal medicine (IM) is one of the most IMG-friendly specialties overall
- Cardiology, vascular medicine, and critical care all deal heavily with vascular disease:
- Peripheral artery disease
- Heart failure and CAD
- Thrombosis, embolism, aneurysmal disease
- You can remain deeply engaged in vascular pathophysiology, guideline development, and even endovascular procedures (in some cardiology subspecialties)
Pros for IMGs:
- Many programs with a high proportion of IMGs and established visa support
- Strong job market and flexible career scaffolding
- Easier to match than vascular surgery or integrated vascular programs, especially for applicants with mid-range to lower Step scores
Cons:
- You may give up open surgical practice
- Procedural opportunities depend on future fellowship (e.g., interventional cardiology) and local institutional setup
- Longer path if you later decide to pursue advanced interventional work
Who should seriously consider this as a plan B specialty:
- IMGs who:
- Have mid-range Step scores or some application weaknesses that make a purely surgical path risky
- Enjoy medicine, pathophysiology, and longitudinal patient care
- Are open to a non-surgical but still vascular‑focused career
Practical strategy:
Dual apply to:
- Vascular surgery (integrated or selective traditional pathways)
- A robust list of internal medicine programs, prioritizing IMG-friendly institutions
In IM personal statements and interviews:
- Emphasize your passion for vascular disease prevention and management
- Highlight your understanding of multidisciplinary care: surgeons, cardiologists, internists, radiologists working together
This dual applying residency approach provides a safer floor while keeping your vascular interest central to your narrative.
4. Neurology with Stroke/Neurointerventional Focus
Relevance to vascular care:
- Stroke is fundamentally a cerebrovascular disease
- Vascular neurology and neurointerventional subspecialties perform:
- Thrombectomies
- Aneurysm coiling
- Management of intracranial and extracranial vascular pathology
Pros:
- Neurology is moderately IMG-friendly, especially community and some academic programs
- Clear vascular focus in stroke and neurocritical care
- Growing interventional field in neuroradiology and endovascular neurosurgery
Cons:
- Pathway to hands-on endovascular interventions may be long and competitive
- Strong emphasis on neurology, which is different in feel from general surgery and vascular surgery
Who this fits:
- IMGs who:
- Are comfortable with complex neuroanatomy and critical care
- Like acute, time‑sensitive decision making
- Are open to primarily cognitive and consultative work with select interventional opportunities
Practical use as a backup:
- It can serve as a secondary plan B after IM or general surgery, especially if you also have neurology rotations or experience.
5. Anesthesiology and Critical Care
Connection to vascular surgery:
- Anesthesiologists often manage intraoperative care for major vascular cases (aortic repair, carotid endarterectomy, limb revascularization)
- Critical care specialists (many from anesthesia or IM backgrounds) manage post-op vascular patients in ICU
- You maintain close proximity to vascular surgery teams and major procedures
Pros for IMGs:
- Anesthesiology has become more competitive, but many programs still accept IMGs
- Good lifestyle relative to many surgical specialties
- Strong job market
Cons:
- Depending on program and region, anesthesia can still be quite competitive
- Not a direct path back into being a primary operating surgeon
Best for:
- IMGs who:
- Enjoy physiology, hemodynamics, and acute care
- Are comfortable relinquishing primary surgeon role but staying in the OR/procedure environment
How to Execute a Dual Applying Residency Strategy Without Hurting Your Chances
Dual applying residency is powerful but must be done carefully, especially as an international medical graduate targeting a vascular surgery residency or integrated vascular program.
1. Tailor your personal statements
Create separate personal statements:
Vascular Surgery / General Surgery PS:
- Emphasize:
- Your long-term interest in operating
- Vascular cases that inspired you
- Technical dexterity, OR experiences, vascular research
- Mention broader surgery (for general surgery PS) so you don’t appear overly narrow or uninterested in non-vascular cases
- Emphasize:
Medicine / Radiology / Other PS:
- Emphasize:
- Your interest in vascular pathology from a diagnostic, preventive, or systemic perspective
- Collaborative care with surgeons
- How you value continuity and longitudinal outcomes, not just the operation
- Emphasize:
Avoid copying language between statements; programs frequently detect generic or mismatched narratives.
2. Manage letters of recommendation strategically
Aim for:
- 3–4 letters total, but assign them strategically in ERAS:
- Surgery-focused letters (vascular or general surgeons): For vascular surgery, integrated vascular program applications, and general surgery programs.
- Non-surgical letters (medicine, radiology, neurology, etc.): For those specific specialties.
If you are dual applying to vascular surgery and internal medicine:
- Use 3–4 letters total, but different subsets for each application type:
- For vascular/general surgery: 2–3 surgery letters + 0–1 IM letter (if they know you well)
- For IM: 2–3 IM letters + 0–1 surgery letter (especially if the surgeon can comment on your work ethic, clinical reasoning, and teamwork)
3. Be honest but tactful when asked about backup specialties
Programs may ask directly or indirectly about your plans.
At vascular surgery or integrated vascular interviews:
- Emphasize:
- “Vascular is my primary goal; I have shaped my training and research toward this path.”
- “I understand that match is competitive, so I have applied widely and thought carefully about programs—but my central commitment is to vascular care.”
- You do not need to give detailed information about every specialty you applied to.
- Emphasize:
At backup specialty interviews (e.g., IM):
- Don’t say, “I’m only here because I might not match vascular.”
- Instead:
- “I’m very interested in vascular disease, and I see internal medicine as a powerful way to impact those patients through prevention, risk factor management, and multidisciplinary care. I could see myself very happy in this role.”
You must be able to convincingly explain why you would be satisfied in that plan B specialty.
4. Application numbers and distribution
Because vascular surgery is extremely competitive (especially integrated):
Most IMGs should consider 100+ total applications across all specialties, distributed roughly as:
If you’re a strong applicant (excellent scores, US research, strong US letters):
- 30–50 integrated vascular / vascular-related general surgery programs
- 40–60 general surgery (categorical + prelim where needed)
- Optionally, 20–40 IM or other backup specialties
If you’re moderate or lower in competitiveness (borderline scores, limited USCE, visa needs):
- 10–20 integrated vascular programs (very targeted)
- 40–70 general surgery (especially community, IMG-friendly)
- 60–100 internal medicine and/or other strongly IMG-friendly fields as a robust backup
Adjust based on finances and ERAS costs, but remember: applications are cheaper than repeating a full match cycle.
Timeline and Stepwise Plan for IMG Backup Specialty Preparation
A structured timeline keeps you from panicking late in the season.
12–18 months before application
Decide on primary focus on vascular surgery
Identify 1–2 probable plan B specialties aligned with vascular care
Plan US clinical experiences in:
- Vascular surgery or general surgery
- Internal medicine, cardiology, radiology, or neurology (as relevant)
Start research projects in vascular, surgery, or your backup’s domain.
9–12 months before application
Confirm your dual applying residency strategy
Take Step 2 CK and aim for your best possible score
Secure letters from both:
- Surgeons (vascular or general)
- Physicians in your backup field
Begin drafting different versions of personal statements.
3–6 months before ERAS opens
- Finalize list of vascular surgery residency programs and integrated vascular programs
- Build IMG-friendly program lists for backup specialties (using NRMP data, FREIDA, institutional websites, alumni input)
- Clarify visa policies for each program
- Ensure your CV emphasizes your vascular focus but remains adaptable.
Application season
- Submit separate, tailored applications to each specialty
- Respond early to all interview invites
- Attend as many realistic interviews as possible, both in primary and backup fields
- Keep notes after each interview to assist with ranking later.
Rank list phase
Construct multiple scenarios:
- If you had only vascular interviews, ranking is straightforward
- If you have both vascular and backup specialty interviews, ask:
- Would you prefer a low-tier vascular or high-tier IM/radiology/other program?
- What geographic or visa priorities matter most?
Rank in true order of your preferences; the algorithm works in your favor if you are honest.
Frequently Asked Questions (FAQ)
1. As an IMG, is vascular surgery too competitive to even try?
Not necessarily. Many IMGs have successfully matched into vascular surgery, especially via the general surgery → vascular fellowship pathway. However, treating vascular surgery as your only option is risky. You should absolutely apply if you are passionate and reasonably competitive, but simultaneously build a strong backup (e.g., general surgery and/or internal medicine) to preserve your chances of training in the US.
2. What is the best backup specialty for an IMG aiming at vascular surgery?
There is no single “best” plan B specialty, but commonly strong options include:
- General Surgery – most direct surgical backup and route to a 5+2 vascular fellowship
- Internal Medicine – safest and most IMG-friendly option with strong vascular overlap (cardiology, vascular medicine)
- Radiology / IR – for applicants who love imaging and endovascular work
The choice depends on your competitiveness, interests, and willingness to consider non-surgical careers.
3. Will dual applying hurt my chances of matching vascular surgery?
If done properly, no. Programs expect applicants to protect themselves in a competitive environment. Problems only arise if:
- You send a medicine-style personal statement to a vascular surgery program, or vice versa
- You openly express that you are not committed to their specialty and see it only as a backup
- Your letters or experiences seem misaligned with your stated goals
Thoughtful, well-separated applications that still tell a coherent story about your interest in vascular disease are unlikely to harm you.
4. If I match into a backup specialty, is my dream of vascular surgery over?
Not always. Many physicians find genuine satisfaction in their backup field and choose to stay. But pathways remain:
- From general surgery, you can still aim for a vascular surgery fellowship
- From internal medicine, you can specialize in vascular medicine, cardiology, or critical care and remain central to vascular patient care
- From radiology, you can train in vascular/interventional radiology
Even if you never become a board-certified vascular surgeon, you can still build a career that is heavily focused on vascular disease and procedural work.
Thoughtful backup specialty planning doesn’t mean you lack confidence; it means you are approaching a highly competitive field with maturity and strategy. As an international medical graduate with a passion for vascular surgery, a well-designed dual applying residency and plan B specialty approach gives you more pathways to become the kind of vascular-focused physician you want to be—whether your title eventually reads “vascular surgeon,” “vascular medicine specialist,” “interventional radiologist,” or something in between.





















